Lecture 7 Animal Virology
advertisement
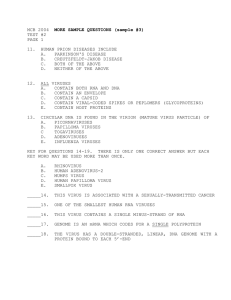
Lecture 7 Animal Virology The problem with Polio: Virus cultivation • 1949: Enders, Weller and Robbins grew poliovirus in cultured (non-neuronal) cells Major breakthrough • Enabled discovery of new viruses and large scale vaccine development • Basic technology for molecular and cell biology • Enables growth of large amounts of pure virus, making possible studies on virus composition and structure Cell culture • Most common method used to propagate viruses. • Cells can grow as monolayers or in suspension cultures. • Primary cell culture – From animal tissues. Limited to 5-20 cell divisions • Diploid cell lines – Homogeneous population of a single type. Typically derived from tumors. Can divide up to 100 times. Remain diploid • Continuous cell lines. – Immortal cells derived from tumors or mutagenesis of primary cells. Aneupolid. Don’t resemble progenitors. Can be tumorigenic. Many types, e.g. HeLa (Henrietta Lacks), HEp-2 (Hu. Epithelial), BHK (Baby Hamster Kidney). Different types of cell culture used in virology A. Primary human foreskin fibroblasts B. Established (immortalized) mouse fibroblasts (NIH 3T3) C. Continuous (transformed) line of human epithelial cells (HeLa) Note differences in morphologies among the primary, established and transformed cell lines. HeLa cells overgrow one another – loss of contact inhibition. The Immortal Life of Henrietta Lacks – HeLa Cells • Her name was Henrietta Lacks, but scientists know her as HeLa. • She was a poor black tobacco farmer whose cells— taken from her cervical cancer at Johns Hopkins without her knowledge in 1951—became one of the most important tools in medicine. • Vital for developing the polio vaccine, cloning, gene mapping, in vitro fertilization, and most recently vaccines against human papilloma virus, which causes cervical cancer, the disease to which she succumbed. • Henrietta’s cells have been bought and sold by the billions, yet she remained virtually unknown, and her family could not afford health insurance. • The book addresses numerous issues regarding the legacies of slavery, issues of race, class and education, and medical ethics. • A movie produced by Oprah Winfrey is currently in production. Cytopathology of virus infections Cytopathology A. Timecourse of polio infection. Note how cells round up and die. Cytopathology B. Syncytium formation induced by Murine leukemia virus. Embryonated eggs • Many viruses grow very well in embryonated chicken eggs. • Robust yield enables use for research and vaccine production Terms describing viral infection of cells Multiplicity of Infection (m.o.i.) • Ratio of input virus to the number of target cells in an infection. • Usually used to describe the infection of a particular cell type grown on a plate or in culture. • Can be used to statistically evaluate the total number of cells that will be infected and the number of viruses that will infect each cell during an infection. Lytic infection- Virus enters cell and usurps cellular machinery to rapidly multiply and in the process kill the cell (many flu and cold viruses). Terms describing viral infection of cells PFU: plaque forming unit • Lysis of cells (lytic infection) creates holes in the monolayer of cells. • Called ‘plaques’ • PFU = the concentration of Viral plaques. The red region is the viruses that can form solidified blood agar, while the white plaques in a volume of a spots are the plaques. The viruses spread through the agar, destroying virus stock. the blood cells within the agar and 1 4 12 13 5 15 16 25 26 3 7 6 14 23 24 2 19 8 17 18 20 21 28 29 27 9 10 11 22 30 31 32 generating these characteristic spots. Terms describing viral infection of cells CFU: colony forming unit • Some viruses can ‘transform’ cells • i.e. allow them to grow when they otherwise would not (lecture 26) • Cells that grow form colonies • CFU is a measure of viruses per volume of stock that can transform cells. Terms describing infections of an organism Acute infection- Rapid onset of disease symptoms result in eradication of the virus or death of the infected animal (cold and flu viruses, ebola). Terms describing infections of an organism Persistent infection • Virus remains associated with the cell without rapidly multiplying or killing the cell. • Three types – (1) virus genome persists within the cell but virus is not released, ex. Some retroviruses. – (2) Virus is released sporadically but remains in a so called "latent" state most of the time (herpes simplex). – (3) Virus is continually released without lysis of host cell, ex. hepatitis B virus. Some bacteriophages (lambda) have developed complex molecular systems to that sense when the conditions warrant a shift. Terms describing infections of an organism • Two classes of persistent infections – Chronic Infection- prolonged infection in which the organism is not immediately killed and the virus is not eradicated (hepatitis, HTLV, HIV). Always symptomatic. – Latent infection – chronic infection that can be periodically reactivated. e.g. herpes simplex virus. Sporadically symptomatic. Terms describing virus transmission • Zoonosis- disease which is naturally transmitted between vertebrate animals and man (rabies, hanta virus). • Often, but not always transferred by an insect vector (arboviruses). Insect transfer can be: – Mechanical transmission - virions transferred directly with no propagation in insect. – Propagative transmission - virus replicates in othropod (insect vector) prior to transfer. Often the virus will first infect the gut cells of the insect and then be transferred the salivary glands to be transmitted during feeding. – Those viruses not transferred by insects may be by direct contact (rabies for example), or contact with bodily wastes or fluids (hantavirus for example). Quantitation of virus activity in whole animals • Infectious dose50 (ID50) – Dose required to infect 50% of the inoculated animals. With most viruses several PFU are required to infect an animal. • Lethal dose50(LD50) – The dose required to kill 50% of the inoculated animals. • Incubation period – The time between the initial infection and the onset of disease symptoms. – Can range from a few days (cold viruses) to years (HIV) at times (show HIV typical curve showing viremia and onset of disease. How do viruses enter? Skin: Not common, however, can enter thru: • small wounds in skin like insect bites (yellow fever virus) • large wounds (rabies from animal bites) More generally, thru epithelial cells How do viruses enter? Entry thru respiratory tract epithelia • Depth of entry may be important, Coxsackie virus cause a nasal cold if only to nose but deeper inhalation of a contaminate mist can cause a sever chest cold. • Many viruses that enter through epithelium may cause may cause more generalized disease (example, African swine fever, smallpox, mumps, measles, rubella). Entry through epithelium of alimentary tract • mouth, esophagus, intestinal mucosa • Some cause local disease • ex. diarrhea by orbi and rotaviruses • Others cause more general (Hepatitis A virus). Entry thru reproductive tract: Venereal • HSV-2, HIV, HTLV-1 Modes of transmission • Horizontal transmission: from one organism to another via direct or indirect contact – Transmission via secretions of epithelial cells e.g. Herpesviruses including Herpes 1 (cold sores) and Epstein-Barr virus (EBV) which can cause mononucleosis (kissing disease). Modes of transmission • Vertical transmission- transfer of virus form parent to offspring. – blood exchange through the placenta (HIV, cytomegalovirus, rubella) – congenitally (HSV), – direct inheritance of germ line integrated virus (mouse type B and C retroviruses). Modes of transmission • Nosocomial transmission: occurs in a clinical setting • Iatrogenic transmission: occurs during a medical procedure.