GLOBAL EPIDEMIOLOGY OF CAPSULAR GROUP W MENINGOCOCCAL
advertisement
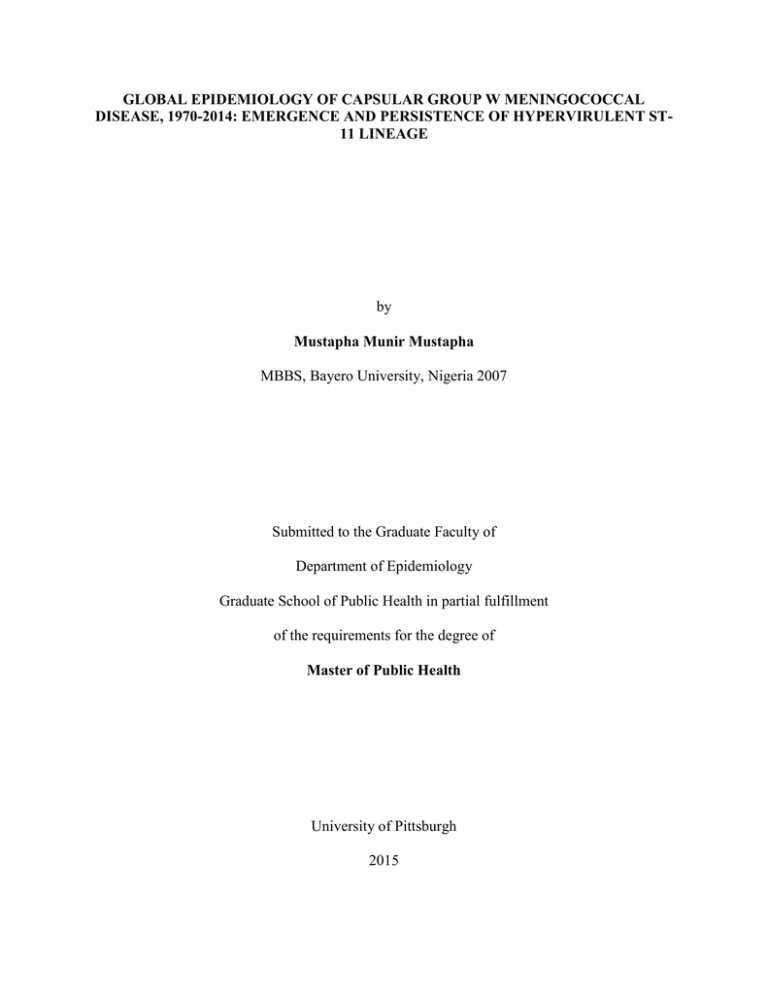
GLOBAL EPIDEMIOLOGY OF CAPSULAR GROUP W MENINGOCOCCAL DISEASE, 1970-2014: EMERGENCE AND PERSISTENCE OF HYPERVIRULENT ST11 LINEAGE by Mustapha Munir Mustapha MBBS, Bayero University, Nigeria 2007 Submitted to the Graduate Faculty of Department of Epidemiology Graduate School of Public Health in partial fulfillment of the requirements for the degree of Master of Public Health University of Pittsburgh 2015 UNIVERSITY OF PITTSBURGH Graduate School of Public Health This essay is submitted by Mustapha Munir Mustapha on December 1st, 2015 and approved by Essay Advisor: Lee H. Harrison, MD Professor, Departments of Epidemiology and Medicine Graduate School of Public Health and School of Medicine University of Pittsburgh Essay Reader: Maria Mori Brooks, PhD Associate Professor, Department of Epidemiology Graduate School of Public Health University of Pittsburgh Essay Advisor: Jane W Marsh, PhD Research Associate Professor, Department of Medicine School of Medicine University of Pittsburgh ii Copyright by Mustapha Munir Mustapha 2015. iii Essay Advisor: Lee H Harrison, MD GLOBAL EPIDEMIOLOGY OF CAPSULAR GROUP W MENINGOCOCCAL DISEASE, 1970-2014: EMERGENCE AND PERSISTENCE OF THE HYPERVIRULENT ST-11 LINEAGE Mustapha M Mustapha, MPH University of Pittsburgh, 2015 ABSTRACT Following an outbreak in Mecca Saudi Arabia in 2000, meningococcal strains expressing capsular group W (W) emerged as a major cause of invasive meningococcal disease (IMD) worldwide. The Saudi Arabian outbreak strain (Hajj clone) belonging to the ST-11 clonal complex (cc11) is similar to W cc11 causing occasional sporadic disease before 2000. Since 2000, W cc11 has caused large meningococcal disease epidemics in the African meningitis belt and endemic disease in South America, Europe and China. Traditional molecular epidemiologic typing suggested that a majority of current W cc11 burden represented global spread of the Hajj clone. However, recent whole genome sequencing (WGS) analyses revealed significant genetic heterogeneity among global W cc11 strains. While continued spread of Hajj-related strains occurs in the Middle East, the meningitis belt and South Africa have co-circulation of the Hajj clone and other unrelated W cc11 strains and South America, the UK and France share a genetically distinct W c11 strain. Other W lineages persist in low numbers in Europe, North America and the meningitis belt. In summary, WGS is helping to unravel the complex genomic epidemiology of group W meningococcal strains. Wider application of WGS and strengthening iv of global IMD surveillance is necessary to monitor the continued evolution of group W lineages. There is need for a vaccine that is protective against group W in the meningitis belt. Public Health relevance: This essay presents a critical review of studies reporting IMD surveillance data spanning four decades and places in context the recent findings of WGS studies to the epidemiology of group W IMD. This report will be of use to Public Health surveillance and policy professionals in several countries currently facing a rise in number of W cc11 cases and persistence of sporadic group W cases. Data presented in this review also provides evidence in support of introduction of group W in the African meningitis belt. v TABLE OF CONTENTS BACKGROUND AND SIGNIFICANCE ................................................................................................. 1 Neisseria Meningitidis .......................................................................................................................... 1 Public Health Significance .................................................................................................................... 2 Aims ...................................................................................................................................................... 4 MOLECULAR CHARACTERISTICS OF GROUP W ......................................................................... 6 Multilocus sequence typing (MLST) .................................................................................................... 6 Outer membrane proteins (OMP), PorA, PorB, and FetA. ................................................................... 6 Whole Genome Sequencing (WGS) ..................................................................................................... 7 Factor H binding protein (FHbp) .......................................................................................................... 8 16S ribosomal RNA gene (16S)............................................................................................................ 9 “Capsular switching” ............................................................................................................................ 9 GLOBAL INCIDENCE OF MENINGOCOCCAL GROUP W DISEASE ........................................ 10 Group W IMD incidence, 1970 – 1999................................................................................................... 10 Group W incidence: 2000 and beyond .................................................................................................... 13 Saudi Arabia (Hajj) 2000-2001 .......................................................................................................... 13 Middle East: endemic W following Hajj epidemics. ........................................................................... 14 Africa: emergence of W cc11 epidemics ............................................................................................. 14 USA and Canada................................................................................................................................. 17 Asia ..................................................................................................................................................... 18 Australia and New Zealand................................................................................................................. 19 DISCUSSION ............................................................................................................................................ 21 CONCLUSION ......................................................................................................................................... 22 vi BIBLIOGRAPHY ..................................................................................................................................... 23 vii LIST OF FIGURES Figure 1: Meningitis belt, 2006 ...................................................................................................... 3 Figure 2: Molecular typing of invasive capsular group W N. meningitidis in Brazil, 1990-2005.. ....................................................................................................................................................... 12 Figure 3: Distribution of confirmed N. meningitidis in Taiwan, 1996-2002.. .............................. 13 Figure 4. Distribution of capsular groups among confirmed invasive meningococcal disease cases, meningitis belt 2003-2015. ................................................................................................. 16 Figure 5. Global occurrence of capsular group W cc11 meningococcal disease, 2000-2014. ..... 20 viii BACKGROUND AND SIGNIFICANCE Neisseria Meningitidis Neisseria meningitidis (meningococcus), an important cause of bacterial meningitis and sepsis worldwide shows dynamic changes in strain distribution over time [1]. The 13 African countries of the ‘meningitis belt’ have the highest incidence of endemic disease and periodic epidemics occur in this region (Figure 1) [2]. The major meningococcal virulence factor is the polysaccharide capsule, which is the target of capsular group-specific vaccines [3] Capsular groups A, B, C, W (formerly W-135), Y and X cause almost all invasive meningococcal disease (IMD). Other virulence factors include major outer membrane proteins (OMP) PorA, PorB, FetA, FHbp and lipooligosaccharide [4, 5]. N. meningitidis undergoes genetic change through point mutation, phase variation, homologous recombination and acquisition of genetic material from both within and outside Neisseria species [4, 6]. These phenomena result in substantial genetic variability even among meningococcal isolates of the same lineage and facilitate emergence and persistence of virulent lineages [7, 8]. N. meningitidis capsular group W (W) was first observed among military recruits in the United States in the late 1960s [9, 10]. The pathogenic potential of group W was recognized by the midlate 1970s [11, 12]. W emerged as a major global cause of IMD following a global outbreak that began among Hajj pilgrims in Mecca, Saudi Arabia in 2000 which resulted in over 400 cases and 52 deaths; previously, group W had not been known to cause outbreaks [13]. The Hajj outbreak strain was characterized as clonal complex (cc) 11, PorA antigen gene type P1.5,2, with a distinct pulsed field gel electrophoresis (PFGE) pattern and 16S ribosomal RNA (16S) type 31 [14]. Since 2000 several W epidemics have occurred in the meningitis belt and case clusters have 1 been reported in South Africa, South America, Europe, United States and China [15-21]. Surveillance studies have shown that group W strains are associated with high high case fatality [18, 22], younger age groups [21, 23-28], and atypical clinical features such as arthritis and pericarditis [20, 29-34]. For example, the median age of patients with group W IMD in South Africa 2000-2005 was 5 years compared to 21 years among cases with group A disease [21]. In Burkina Faso in 2002 – 2003, 62% of W cases were in children <5years old compared to 7% of group A cases [35]. Molecular surveillance studies using traditional genotyping techniques suggested that the current global burden of W cc11 represented continued spread of the epidemic Hajj clone [36, 37]. However, recent data based on whole genome sequencing (WGS) suggest that the molecular epidemiology of W cc11 is more complex [38]. In this review, we examine the global distribution and molecular characteristics of group W from 1970-2015 with emphasis on the emergence of endemic and epidemic W cc11 disease since 2000. Public Health Significance IMD is often a fatal disease; mortality rates range between 5-10% with survivors suffering from long term sequelae such as hearing loss and other neurologic deficits, limb amputation, and renal damage [39, 40]. Transmission is through close contact with airway droplets of asymptomatically colonized individuals. Risk factors for IMD are close contact with an IMD patient, cigarette smoking, kissing, immune complement deficiency and crowding in bars, dormitories or large human gatherings [1]. Jafri et al [41] classified global meningococcal disease incidence pattern into countries with epidemic and/or high endemic disease with incidence rates >10 cases per 100,000 population that 2 comprise most African countries, Uruguay, New Zealand and Mongolia. The highest incidence rates of 100-1000 per 100,000 are witnessed during occasional epidemics across 21 countries [42] in Africa collectively referred to as the ‘meningitis belt’ (Figure 1) [2]. Moderate endemic rates are between 2-10 cases per 100,000 population and occur in South Africa, some European countries, Brazil, Cuba and Australia. Remaining countries have low endemic rates (<2/100,000). Figure 1: Meningitis belt, 2006 (Source: U.S. Centers for Disease Control and Prevention) The epidemiologic pattern of meningococcal disease differs by capsular group over time [43]. Capsular group A is most common cause of epidemic meningitis; for example, an outbreak of group A meningococcal disease in 1996 in the meningitis belt resulted in over 250,000 cases and 3 25,000 deaths [44]. Group B causes sporadic disease and small outbreaks in low to moderate endemic countries [45, 46] but is very uncommon in the meningitis belt. Group C also causes sporadic disease and small case clusters globally [47], although group C strains occasionally cause large epidemics in the meningitis belt [48]. In recent decades, groups W and Y have emerged to cause significantly higher number of meningococcal disease cases globally [13, 17, 20, 49-52] while smaller group X [53, 54] epidemics have occurred in the meningitis belt. IMD is a rapidly progressive disease that can cause death within 24-48 hours in previously healthy individuals or may lead to serious sequelae among survivors [55]. Additionally, outbreaks of meningococcal disease cause substantial economic cost and societal disruption [56, 57]. Vaccines remain the primary control strategy against meningococcal disease [58]. Laboratory surveillance of circulating meningococcal strains is critical for monitoring trends, informing vaccine policy, timely detection of outbreaks, and understanding the emergence of new IMD strains. Aims This essay reviews the global distribution of group W meningococcal disease across five decades with a focus on the recent emergence of the W cc11 in recent decades as a major cause of meningococcal disease globally. A comparative review of current and historic molecular typing approaches used to classify group W strains is also presented. The aim is to provide Public Health personnel, microbiologists and epidemiologists with a reference framework that will assist in critical evaluation and interpretation of local meningococcal incidence and surveillance reports in order to make sound evidence-based public health decisions. 4 Surveillance data presented in this essay, combined with the recent success with the control of group A disease in the meningitis belt [59], make a compelling case for the introduction of a multivalent protein conjugate vaccine that covers group W strains in the meningitis belt where several thousand cases of IMD are caused by W strains. We also propose strengthening global meningococcal disease surveillance and broader application of whole genome characterization given the limitation of conventional genotyping approaches in discriminating group W strains. 5 MOLECULAR CHARACTERISTICS OF GROUP W Multilocus sequence typing (MLST) MLST is the method of choice for determining the genetic lineage of N. meningitidis [60]. Strains of the same sequence type (ST) share a common lineage and closely related STs are grouped under the same clonal complex (cc). Cc11 is a globally widespread, hyperinvasive cc comprised of strains expressing capsular groups B, C, W and Y [61, 62]. Historically, cc11 was more commonly associated with capsular group B in the 1960s [63, 64] and with group C from the early 1970s [65, 66]. Group W strains represented only a very small proportion of cc11 strains in the 1970s-1990s [61]. Following the Hajj 2000 epidemic [13], cc11 became the predominant W lineage globally and the only group W lineage associated with epidemic disease. Sporadic group W belonging to other clonal complexes have occurred at low levels globally [36, 67] including cc22 in North America [46, 68] and Europe [37, 69, 70]; cc175 in the meningitis belt [54, 71, 72] and cc174 in Brazil [36]. Outer membrane proteins (OMP), PorA, PorB, and FetA. PorA and PorB are virulence determinants and the basis of serologic classification of meningococci. Meningococcal serotype and serosubtype are based on antigenic properties of PorB and PorA respectively [61]. Serologic classification has been superseded by gene sequence typing curated by the PubMLST database (pubmlst.org/neisseria/) [73]. Sequence variation within the porA gene, combined with MLST is a powerful tool for molecular surveillance [73, 74]. The porB [75] and fetA [76] genotypes are often used to further characterize invasive meningococcal strains. The W cc11 lineage is characterized by a remarkably stable outer membrane allelic profile P1.5,2:F1-1:2-2 (PorA VR1,VR2:FetA:PorB) despite global spread and 6 different epidemiologic patterns over four decades [14, 15, 17, 21, 37, 70, 77, 78]. Although the P1.18 porA allele predominates among W cc22 strains [46, 69, 70, 79], OMP allelic profile variability among W cc22 isolates is consistent with non-clonal, sporadic disease (http://pubmlst.org/neisseria/) [37, 46]. Pulse field gel electrophoresis (PFGE): PFGE [80] has been used by some molecular epidemiologic studies [14, 36, 81, 82] to discriminate W cc11 Hajj outbreak strains from endemic strains. Six of 19 (32%) sporadic preHajj W cc11 isolates were indistinguishable by PFGE from the Hajj clone with remaining 13 isolates having >85% PFGE similarity to the Hajj clone [14]. Also, non-Hajj related W cc11 from Cameroon in 1999-2000 had 2-3 band differences from Hajj clone by PFGE [82]. It was not clear whether strains with ≥3 PFGE band differences compared to the Hajj clone isolated from France [37], Burkina Faso [83] and Brazil [36] in 2000-2003 represented continued expansion of the Hajj clone. Thus, PFGE was able to discriminate between W isolates belonging to different clonal complexes but was less discriminatory for epidemic and sporadic W cc11 strains. Despite this limitation, PFGE has been utilized to describe W strains as likely descendants of the Hajj clone [36, 83]. Whole Genome Sequencing (WGS) WGS data are now publically available for several hundreds of genomes and are increasingly applied to the study of molecular epidemiology of global meningococcal lineages [87, 88]. Indepth genomic comparison of group B, C and W cc11 strains using genome-wide allelic profiling [89, 90] revealed that W cc11 strains were phylogenetically distinct from C and B strains. Phylogenetic studies [38, 90] also show that the W cc11 forms a distinct branch within 7 cc11, suggesting that a majority of current and historic W cc11 strains shared a common origin, likely through a historic capsular switching event [91]. WGS studies have further discriminated W cc11 strains into a number of distinct phylogenetic clusters. Based on allelic profiles of 1546 core genomes, Lucidarme et al [90] classified W cc11 into Anglo-French Hajj strains; Burkina Faso/North Africa strain and South American/UK strain (Table 1). Similarly, based on antigenic profiles, SNP and core genome phylogenetic analyses, Mustapha et al [91] discriminated W cc11 strains linked to the Hajj outbreak from non-Hajj related endemic clusters and showed that the Hajj cluster acquired a number of unique virulence factors through allelic exchange. In summary, these studies demonstrate significant genetic diversity within W cc11 lineage and that genetically distinct sub-lineages were associated with different geographic and epidemiologic settings. Factor H binding protein (FHbp) FHbp is a meningococcal surface protein and one of the polysaccharide capsule-independent antigens used in vaccines that were developed for prevention of group B disease [5]. There is marked variability in the fHbp gene among W cc11 strains globally. The Hajj clone and descendant strains shared FHbp protein 9 (variant group 1); non-Hajj related W cc11 strains shared FHbp proteins belonging to variant groups 2 and 3; FHbp 22 is predominant among nonHajj strains in Chile, Argentina, and Europe while strains from Africa and Brazil shared FHbp 23 and 151 respectively (http://pubmlst.org/neisseria/) [18, 20, 38, 92, 93]. Substantial fHbp gene diversity could be a common characteristic shared by cc11 strains regardless of capsular group given that group C cc11 strains from Canada were recently shown to exhibit extensive fHbp gene diversity [94]. 8 16S ribosomal RNA gene (16S) 16S sequencing showed promise in discriminating the Hajj clone from sporadic W cc11. The Hajj clone contained 16S type 31 while sporadic W cc11 had 16S types 13 and 14 [14, 36]. “Capsular switching” The expression of a different polysaccharide capsule through allelic exchange of capsular genes, has been linked with an increased incidence of meningococcal disease [84, 85]. In 1970-1999, cc11 genetic lineage was most commonly associated with invasive group C strains [61, 86]. This observation suggested that W cc11 strains arose through C→W capsular switch, although the true direction of the genetic exchange is unknown. 9 GLOBAL INCIDENCE OF MENINGOCOCCAL GROUP W DISEASE Group W IMD incidence, 1970 – 1999 Capsular group W was associated with sporadic IMD cases globally in the 1970s through the mid-1990s. However, some surveillance data from the African meningitis belt, UK, Brazil and Taiwan suggest an increase in W cc11 in the mid- to late 1990s, predating the Hajj 2000 epidemic. Active surveillance in the United States identified W in 3% and 4% of invasive meningococcal isolates from 1989-1991 [95] and 1992-1996 [96] respectively. In Canada W caused 3-6% of annual reported IMD cases in 1997-1999 [97] and <1% of IMD cases in Quebec, 1991-1992 [98]. In Australia 6% of 66 IMD isolates in 1971-1980[99] and 8.2% of 110 IMD isolates in 1977-1987 [100] belonged to group W. In Netherlands, W strains predominantly with PorB serotype 2a, represented <2.5% of all IMD isolates in 1959-1983 [101, 102] and 19801990[103]; W strains with phenotype 2a:P1.2,5 caused 3.5% of IMD in Poland, 1995-1996 [104]. In Italy, W strains represented 3.6% of 56 confirmed IMD cases in Italy 1994 [105] and <1% in 1999-2001 [106] Sporadic W cases caused <8% of IMD cases in Norway and Denmark in the 1970s [107]; in Greece, 1996-1997 [108]; East Germany, 1971-1984[109] and Scotland 1972-1982 [110]. In England and Wales, average annual W cases increased to 42 cases/year in 1996/97-1998/99 compared to 18 cases/year in 1993/94-1995/96 [47] Some sporadic W strains from 1970-1999 from UK [14], France [37], Netherlands and Sweden [70] were found to be genetically similar to the Hajj clone by various molecular typing methods [14, 37, 70]. In Sweden, P1.18 subtype, associated with cc22 was also common among sporadic W strains [70]. 10 In summary, diverse W strains, including strains genetically similar to the Hajj clone caused a small proportion of IMD cases across Europe and North America during 1970-1999. In the African meningitis belt, W cc11 was identified in 3.1% of 349 endemic meningococcal disease strains from Senegal and Niger in 1981-1982 [111] and 7.3% of 41 strains from the Gambia [112]. In 1992-1995, an unexpectedly high proportion of W cc11 (43%) was observed in a small sample of 14 endemic case isolates in Gambia [113]. In Brazil, W represented <2% of all meningococcal disease isolates from 1990-2001 [36]. The proportion of Brazilian W cc11 isolates increased from 35% of 63 W isolates in 1990-1995 to 80% of 56 W isolates in 19961999 [36], while the proportion of cc174 declined from 52% to 16% among W isolates (Figure 2). All 67 W cc11 strains from Brazil in 1990-1999 were indistinguishable from the Hajj clone by porA and fetA genotyping but differed from the Hajj clone by both16S and PFGE [36]. Laboratory surveillance in Taiwan identified W cc11 among 30% (16/53) of confirmed IMD cases in 1996-1999 (Figure 2B) [114] while rare W cases were reported from Malaysia [115], Indonesia[14] and Thailand [116] in the 1980s and 1990s. W strains have been identified among disease isolates in Saudi Arabia throughout the 1990s [117-119]. Group W comprised 13% of IMD case isolates in Saudi Arabia in 1994-1999 [119] and a small proportion (<10%) of IMD isolates in Egypt [120], Israel [121] and Kuwait [122] in the 1980s and 1990s. These data demonstrate that W strains were endemic to the Middle East and W cc11 cases existed in parts of Asia since the 1980s. 11 Figure 2: Molecular typing of invasive capsular group W N. meningitidis in Brazil, 1990-2005. Based on data from Lemos et al [36]. 12 Figure 3: Distribution of confirmed N. meningitidis in Taiwan, 1996-2002. Based on data from Chiou et al [114]. Group W incidence: 2000 and beyond Saudi Arabia (Hajj) 2000-2001 During the Hajj 2000 outbreak, over 400 cases of W cc11 disease were recorded among pilgrims and their close contacts across 16 different countries in Europe, Africa, Middle East, Southeast Asia and the United States (Figure 5). This represented the first known outbreak of group W disease [13, 22, 123, 124]. In 2001, a similar outbreak among pilgrims from Saudi Arabia occurred with 106 meningococcal cases reported that were indistinguishable from the 2000 Hajj clone by MLST, porA and fetA genotyping [22, 125] and by PFGE [14, 37, 70]. In 2002, a quadrivalent polysaccharide vaccine that covers W capsular antigen was made a visa requirement 13 for all pilgrims traveling to Saudi Arabia, where no subsequent W outbreaks have been reported [22, 125]. Middle East: endemic W following Hajj epidemics. Following the 200-2001 epidemics in Saudi Arabia, W became a leading cause of endemic meningococcal disease across the Middle East [126]. While Saudi Arabia witnessed a decline in meningococcal disease from 338 cases in 2000 to 6 cases in 2009, reports from Qatar, Oman, Kuwait and United Arab Emirates indicated that W was the most commonly identified meningococcal group in 2001-2009 [122, 126]. It is unclear whether these endemic W cases represented spread and persistence of the Hajj clone. Laboratory surveillance of IMD strains identified W cc11 in 4.5% of 67 IMD isolates from Egypt, 1998-2003 [120] and 38.1% of 333 confirmed pediatric IMD cases in Turkey, 2005-2012 [127]. WGS studies demonstrate that endemic W cc11 strains from Turkey represent continued spread of the Hajj clone [90]. Africa: emergence of W cc11 epidemics Cases of W cc11 among Hajj pilgrims and their contacts were reported across Africa in Morocco, Sudan, Chad, Central African Republic, and Burkina Faso in 2000 and 2001 [42, 124]. In 2001, disease caused by W cc11 was equally as common as group A in a non-representative sample of cases from outbreaks in Burkina Faso and Niger [128]. In 2002, the largest known W epidemic occurred in Burkina Faso, with over 12,000 cases and 1,400 deaths [78]. More than 80% of cases were due to W cc11 strains [56] with antigenic type P1.5,2 similar to the Hajj clone [78]. In 2003-2008, W cc11 epidemics subsided despite persistence of endemic cases [25, 42] [129]. Also, a substantial proportion of endemic W disease in the meningitis belt was caused by W cc175 [67, 81, 130]. These data demonstrate the presence of other clonal W lineages in the meningitis belt post Hajj. Further W cc11 epidemics were recorded across the meningitis belt in 14 2009-2014 [17, 24, 42, 131] making W the most commonly isolated capsular group across the meningitis belt in 2010-2014 (Figure 4). Genomic analyses [20, 38, 90] reveal that W cc11 in the meningitis belt were heterogeneous, with persistence of both the Hajj clone and strains unrelated to the Hajj outbreak. Hajj related W cc11 shared FHbp allele 9 while FHbp alleles 23 and 151 were predominant among non-Hajj endemic strains in the meningitis belt [38, 92]. Given the limited number of isolates characterized by whole genome sequencing, the relative contribution of the Hajj clone to W cc11 epidemics across the region is difficult to assess [17, 23, 132, 133]. The introduction of a highly effective group A polysaccharide-protein conjugate vaccine (MenAfriVac) in 2010 – 2014 led to a dramatic reduction in group A meningococci both in disease cases and asymptomatic carriage [59, 134] that could lead to elimination of group A epidemics within the region and underscores the importance of the recent emergence of W disease. 15 Figure 4. Distribution of capsular groups among confirmed invasive meningococcal disease cases, meningitis belt 2003-2015. On average, 9.3% of suspected meningitis cases had their cerebrospinal fluid (CSF) tested for common bacterial pathogens in 2005-2010 compared to 25.5% in 2011-2015. Others* depict all confirmed cases that were not group A or W in 2004-2009. Data from 2005 covers only weeks 118 while 2015 data covers the first 35 weeks of the year when most meningococcal disease cases occur. Based on publically available data from WHO (http://www.who.int/csr/disease/meningococcal/en/) [42]. Outside the meningitis belt, W strains, predominantly belonging to cc11, represented 9% of 350 IMD strains from South Africa in 1999-2002 [135]. In 2005, South Africa witnessed a doubling 16 of meningococcal disease incidence due to an increase in W cc11 [21]. Similarly, meningococcal disease incidence attributed to W cc11 increased in neighboring Mozambique from 2005-2008 [136]. Similar to the meningitis belt, South Africa also has co-circulation and persistence of non-Hajj endemic W cc11. More than 72% of W cc11 cases in South Africa in 2003-2013 were caused by strains representing continued spread of the Hajj clone [38] while 28% were phylogenetically diverse, non-Hajj related isolates that shared FHbp alleles 22, 151 and 4 (http://pubmlst.org/neisseria/) [38]. Genetic heterogeneity among non-Hajj W cc11 strains in South Africa could represent evolution of a historical strain over several decades or may be a result of multiple introductions of global W cc11 lineages. South America: Emergence of endemic W cc11 clusters. Southern Brazil, Argentina and Chile witnessed the emergence of W cc11 as a major cause of endemic meningococcal disease after 2003 [137]. Case clusters first appeared in southern Brazil where W represented 17.8% of all invasive strains in 2003-2005 compared to 3.2% in 1995-2002 [138]. In Argentina, W cases increased from 7% in 2006 to 50% of all isolates in 2008-2011 [49]. Similarly, the proportion of W cc11 increased in Chile from 6.6% in 2010 to 58.3% in 2012 [18]. Similar to UK, and France, W cc11 from Chile and Argentina also shared FHbp allele 22 [18, 90] while Brazil W cc11 strains had FHbp allele 151. USA and Canada No increase in endemic W in the United States was observed despite presence of Hajj related W cc11 cases in 2000 [14]. W made up 2.3% (48/1979) of all isolates identified through sentinel surveillance in the United States during 2000-2010 [46, 79]; cc22 predominated with only 2 cases of W cc11. However, a cluster of 14 W cc11 cases was reported in 2008-2009 in Florida [15]. WGS reveals that W cc11 from Florida were most genetically similar to South American 17 strains [38]. Low incidence rates of W disease (0.01-0.05 per 100,000) have persisted in Canada from 1990-2011 accounting for 5% of all IMD cases [139]. In Quebec 2009-2013, W cc22 represented 3.8% of 263 confirmed IMD cases [68]. Europe: emergence of endemic W cc11 clusters and persistence of sporadic W cc22 Cases of W cc11 among returning pilgrims and their close contacts were reported across several European countries in 2000 and 2001 [22, 123]. An overall increase in W disease occurred in France [140]. Among 101 W case isolates in France 45% (45/101) belonged to cc11 among which 32% (32/101) were indistinguishable from the Hajj clone by serotyping and PFGE [37]. In 2006-2008, W cc11 cases declined and were replaced by cc22 [29]. A cluster of imported W cc11 cases from the meningitis belt was reported in France during 2012 [16]. A similar increase in W cases related to the Hajj outbreak was seen in the England and Wales 2000-2002 [47]; W cases returned to pre-2000 levels in 2003 – 2008 and then increased again in 2009-2014, with 15% of all meningococcal disease cases in 2013-2014 being group W.[20] Over 67% of all W cases in the UK 2010-2013 belonged to cc11 while cc22 persisted as a cause of sporadic disease [20]. In Spain, W cc22 strains represented 1.6% of IMD cases in the Basque region, 1990-2004 [141]. Likewise in Italy, W persisted as a cause of sporadic IMD causing for 2.6% of IMD cases in 2006-2014 [142, 143] where cc22 predominated with fewer W cc11 isolates [69]. Recent W cc11 case clusters from the UK, Ireland and France 2009-2015 formed a common phylogenetic cluster with strains from Brazil, Chile and Argentina [90]. These data suggest that European W cc11 clusters represent continuing spread of the South American strain. Asia In Singapore, Hajj related and endemic W cc11 cases were reported in 2000-2002 [144] but have not been reported since 2003 suggesting disappearance of endemic W cc11 [144]. In Taiwan 18 2000-2001, average W cc11 case isolates increased to 34 cases/year compared to 4 cases/year in 1996-1999 [114]. Also, endemic W cc11 cases emerged in China (2011-2012) where 24.4% (11/45) confirmed IMD in 2011 -2012 cases were W cc11 [19]. Rare group W cases belonging to cc4821 have also occurred in China [145]. It is unclear whether W cc11 in Taiwan and China represent expansion of local endemic strains or continued global spread of the Hajj clone. A few W cases (<4) were also reported in Malaysia [115], India [146] and Japan [147]. In Korea, a cluster of three of W cc11 cases whose OMP genotype (P1.5-1,2-2:F3-9) differed from that of other global W cc11 strains was identified among military recruits [148]. These data demonstrate the complex molecular epidemiology of W strains, and the need to strengthen molecular surveillance of N. meningitidis in parts of Asia. Australia and New Zealand In Australia, W caused 1.5-5% of annual IMD cases in 1997-2012; group W isolates were of diverse porA genotypes including a few with P1.5,2 genotype similar to that found in global W cc11 strains [149]. Disease caused by W continued to be rare in New Zealand, accounting for 3.5% of 700 reported IMD cases in 2008-2013 [45]. One case of W:P1.5,2:cc11, identical to global W cc11 strains, was reported in New Zealand, while a cluster of W cc11 P1.7-2,4 cases genetically distinct from global W cc11 was reported in 2003 [85]. A New Zealand W cc11 P1.72,4 strain was shown to have arisen through capsular switching between locally endemic group C and a carriage group W strain.[85]. 19 Figure 5. Global occurrence of capsular group W cc11 meningococcal disease, 2000-2014. Blue boxes represent W cc11 strains with known epidemiologic and/or genetic link to the Hajj 2000 outbreak; red boxes represent W cc11 strains not linked to the Hajj outbreak and gray boxes represent W cc11 clusters with unknown link to the Hajj outbreak. 20 DISCUSSION Epidemic W cc11 IMD began with the 2000 Hajj outbreak. However, an upward trend in W cc11 sporadic cases occurred in the mid to late 1990s in the meningitis belt [82, 113], Brazil [36], UK [47] and Taiwan [114]. Application of WGS to molecular surveillance of meningococcal disease revealed that several W cc11 case clusters arose independent of the Hajj epidemic consistent with global multifocal emergence of W cc11 [20, 38, 90]. W cc11 was found to comprise a number of genetically and geographically diverse sub-lineages and different sub-lineages could coexist within the same country at the same time. W cc22 in Europe and North America and cc175 in Africa have persisted as a cause of a minority of disease cases. The Hajj, an annual gathering of over 2 million people from around the world is an ideal setting for the selection and rapid global dissemination of virulent meningococci. For example, in 1987, a Hajj-related meningococcal outbreak facilitated the spread of virulent group A cc5 meningococci from south Asia to sub-Saharan Africa [150]. Excessive crowding during the Hajj may have facilitated rapid, intense transmission of an antigenically novel strain within an immunologically naïve population [86]. The Hajj clone and its descendants shared a number of recombination events leading to allelic exchange within fHbp gene and metabolic genes, nor and aniA. These methobolic genes may be involved in nasopharyngeal survival of meningococci and could have played a role in increased virulence of the Hajj clone. It is also hypothesized that the polysaccharide group A/C vaccine requirement for Hajj pilgrims in the 1990s could have led to selection of a group W strain that had undergone capsular switching [86, 151]. Existence of multiple endemic clusters caused by strains unrelated to the Hajj epidemic suggests that different 21 genetic and/or environmental factors could be responsible for emergence and persistence of different sub-lineages in different epidemiologic settings. CONCLUSION Group W strains belonging to clonal complex (cc) 11 have emerged during the past 15 years as a major cause of global meningococcal disease. The recent success with the control of group A disease in the meningitis belt has led to the predominance of W as the cause of meningococcal disease in the region [59]. This, in combination with the emergence of disease caused by capsular groups X [54, 152] and C [48], underscore the need for polyvalent vaccines for the meningitis belt. Strengthened global meningococcal disease surveillance and broader application of whole genome characterization is needed given that conventional molecular typing does not sufficiently discriminate W cc11 strains. 22 BIBLIOGRAPHY [1] Harrison LH, Trotter CL, Ramsay ME. Global epidemiology of meningococcal disease. Vaccine. 2009;27 Suppl 2:B51-63. [2] Lapeyssonnie L. [Comparative epidemiologic study of meningococcic cerebrospinal meningitis in temperate regions and in the meningitis belt in Africa. Attempt at synthesis]. Med Trop (Mars). 1968;28:709-20. [3] Harrison OB, Claus H, Jiang Y, Bennett JS, Bratcher HB, Jolley KA, et al. Description and nomenclature of Neisseria meningitidis capsule locus. Emerg Infect Dis. 2013;19:566-73. [4] Stephens DS. Biology and pathogenesis of the evolutionarily successful, obligate human bacterium Neisseria meningitidis. Vaccine. 2009;27 Suppl 2:B71-7. [5] Pizza M, Rappuoli R. Neisseria meningitidis: pathogenesis and immunity. Curr Opin Microbiol. 2015;23:68-72. [6] Hao W, Ma JH, Warren K, Tsang RS, Low DE, Jamieson FB, et al. Extensive genomic variation within clonal complexes of Neisseria meningitidis. Genome Biology and Evolution. 2011;3:1406-18. [7] Buckee CO, Jolley KA, Recker M, Penman B, Kriz P, Gupta S, et al. Role of selection in the emergence of lineages and the evolution of virulence in Neisseria meningitidis. Proc Natl Acad Sci U S A. 2008;105:15082-7. [8] Kong Y, Ma JH, Warren K, Tsang RS, Low DE, Jamieson FB, et al. Homologous recombination drives both sequence diversity and gene content variation in Neisseria meningitidis. Genome Biology and Evolution. 2013;5:1611-27. [9] Evans JR, Artenstein MS, Hunter DH. Prevalence of meningococcal serogroups and description of three new groups. Am J Epidemiol. 1968;87:643-6. [10] Brundage JF, Ryan MA, Feighner BH, Erdtmann FJ. Meningococcal disease among United States military service members in relation to routine uses of vaccines with different serogroup-specific components, 1964-1998. Clin Infect Dis. 2002;35:1376-81. [11] Griffiss JM, Brandt BL. Disease due to serogroup W135 Neisseria meningitidis. Pediatrics. 1979;64:218-21. [12] Kleiman MB, Reynolds J, Steinfeld J, Allen SD, Smith JW. Meningitis caused by Neisseria meningitidis serogroup 135. Journal of clinical microbiology. 1978;8:621-2. [13] Taha MK, Achtman M, Alonso JM, Greenwood B, Ramsay M, Fox A, et al. Serogroup W135 meningococcal disease in Hajj pilgrims. Lancet. 2000;356:2159. [14] Mayer LW, Reeves MW, Al-Hamdan N, Sacchi CT, Taha MK, Ajello GW, et al. Outbreak of W135 meningococcal disease in 2000: not emergence of a new W135 strain but clonal expansion within the electophoretic type-37 complex. J Infect Dis. 2002;185:1596-605. [15] Doyle TJ, Mejia-Echeverry A, Fiorella P, Leguen F, Livengood J, Kay R, et al. Cluster of serogroup W135 meningococci, southeastern Florida, 2008-2009. Emerg Infect Dis. 2010;16:113-5. [16] Taha MK, Kacou-N'douba A, Hong E, Deghmane AE, Giorgini D, Okpo SL, et al. Travel-related Neisseria meningitidis serogroup W135 infection, France. Emerg Infect Dis. 2013;19:1030-2. [17] MacNeil JR, Medah I, Koussoube D, Novak RT, Cohn AC, Diomande FV, et al. Neisseria meningitidis serogroup W, Burkina Faso, 2012. Emerg Infect Dis. 2014;20:394-9. [18] Araya P, Fernandez J, Del Canto F, Seoane M, Ibarz-Pavon AB, Barra G, et al. Neisseria meningitidis ST-11 clonal complex, Chile 2012. Emerg Infect Dis. 2015;21:339-41. [19] Zhou H, Liu W, Xu L, Deng L, Deng Q, Zhuo J, et al. Spread of Neisseria meningitidis serogroup W clone, China. Emerg Infect Dis. 2013;19:1496-9. 23 [20] Ladhani SN, Beebeejaun K, Lucidarme J, Campbell H, Gray S, Kaczmarski E, et al. Increase in endemic Neisseria meningitidis capsular group W sequence type 11 complex associated with severe invasive disease in England and Wales. Clin Infect Dis. 2015;60:578-85. [21] von Gottberg A, du Plessis M, Cohen C, Prentice E, Schrag S, de Gouveia L, et al. Emergence of endemic serogroup W135 meningococcal disease associated with a high mortality rate in South Africa. Clin Infect Dis. 2008;46:377-86. [22] Hahne SJ, Gray SJ, Jean F, Aguilera, Crowcroft NS, Nichols T, et al. W135 meningococcal disease in England and Wales associated with Hajj 2000 and 2001. Lancet. 2002;359:582-3. [23] Collard JM, Maman Z, Yacouba H, Djibo S, Nicolas P, Jusot JF, et al. Increase in Neisseria meningitidis serogroup W135, Niger, 2010. Emerg Infect Dis. 2010;16:1496-8. [24] Collard JM, Issaka B, Zaneidou M, Hugonnet S, Nicolas P, Taha MK, et al. Epidemiological changes in meningococcal meningitis in Niger from 2008 to 2011 and the impact of vaccination. BMC Infectious Diseases. 2013;13:576. [25] Traore Y, Njanpop-Lafourcade BM, Adjogble KL, Lourd M, Yaro S, Nacro B, et al. The rise and fall of epidemic Neisseria meningitidis serogroup W135 meningitis in Burkina Faso, 2002-2005. Clin Infect Dis. 2006;43:817-22. [26] Ceyhan M, Yildirim I, Balmer P, Borrow R, Dikici B, Turgut M, et al. A prospective study of etiology of childhood acute bacterial meningitis, Turkey. Emerg Infect Dis. 2008;14:1089-96. [27] Barra GN, Araya PA, Fernandez JO, Gabastou JM, Hormazabal JC, Seoane M, et al. Molecular Characterization of Invasive Neisseria meningitidis Strains Isolated in Chile during 2010-2011. PloS One. 2013;8:e66006. [28] Efron AM, Sorhouet C, Salcedo C, Abad R, Regueira M, Vazquez JA. W135 invasive meningococcal strains spreading in South America: significant increase in incidence rate in Argentina. Journal of clinical microbiology. 2009;47:1979-80. [29] Gaschignard J, Levy C, Deghmane AE, Dubos F, Muszlak M, Cohen R, et al. Invasive serogroup w meningococcal disease in children: a national survey from 2001 to 2008 in France. The Pediatric infectious disease journal. 2013;32:798-800. [30] Brasier AR, Macklis JD, Vaughan D, Warner L, Kirshenbaum JM. Myopericarditis as an initial presentation of meningococcemia. Unusual manifestation of infection with serotype W135. The American journal of medicine. 1987;82:641-4. [31] Ejlertsen T, Vesterlund T, Schmidt EB. Myopericarditis with cardiac tamponade caused by Neisseria meningitidis serogroup W135. Eur J Clin Microbiol Infect Dis. 1988;7:403-4. [32] Apfalter P, Horler R, Nehrer S. Neisseria meningitidis serogroup W-135 primary monarthritis of the hip in an immunocompetent child. Eur J Clin Microbiol Infect Dis. 2000;19:475-6. [33] Faye A, Mariani-Kurkdjian P, Taha MK, Angoulvant F, Antonios M, Aubertin G, et al. Clinical features and outcome of pediatric Neisseria meningitidis serogroup W135 infection: a report of 5 cases. Clin Infect Dis. 2004;38:1635-7. [34] Osuorah D, Shah B, Manjang A, Secka E, Ekwochi U, Ebenebe J. Outbreak of serotype W135 Neisseria meningitidis in central river region of the Gambia between February and June 2012: a hospitalbased review of paediatric cases. Niger J Clin Pract. 2015;18:41-7. [35] Parent du Chatelet I, Traore Y, Gessner BD, Antignac A, Naccro B, Njanpop-Lafourcade BM, et al. Bacterial meningitis in Burkina Faso: surveillance using field-based polymerase chain reaction testing. Clin Infect Dis. 2005;40:17-25. [36] Lemos AP, Harrison LH, Lenser M, Sacchi CT. Phenotypic and molecular characterization of invasive serogroup W135 Neisseria meningitidis strains from 1990 to 2005 in Brazil. The Journal of Infection. 2010;60:209-17. [37] Taha MK, Giorgini D, Ducos-Galand M, Alonso JM. Continuing diversification of Neisseria meningitidis W135 as a primary cause of meningococcal disease after emergence of the serogroup in 2000. Journal of clinical microbiology. 2004;42:4158-63. 24 [38] Mustapha MM, Marsh JW, Krauland MG, Fernandez JO, de Lemos APS, Dunning Hotopp JC, et al. Genomic Epidemiology of Hypervirulent Serogroup W, ST-11 Neisseria meningitidis. EBioMedicine. 2015;2:1447-55. [39] Jusot JF, Tohon Z, Yazi AA, Collard JM. Significant sequelae after bacterial meningitis in Niger: a cohort study. BMC Infectious Diseases. 2013;13:228. [40] Rosenstein NE, Perkins BA, Stephens DS, Popovic T, Hughes JM. Meningococcal disease. The New England Journal of Medicine. 2001;344:1378-88. [41] Jafri RZ, Ali A, Messonnier NE, Tevi-Benissan C, Durrheim D, Eskola J, et al. Global epidemiology of invasive meningococcal disease. Population health metrics. 2013;11:17. [42] Weekly feedback bulletin on cerebrospinal meningitis. Meningitis Weekly Bulletin. http://www.who.int/csr/disease/meningococcal/epidemiological/en/index.html: World Health Organization; 2002-2015. [43] Halperin SA, Bettinger JA, Greenwood B, Harrison LH, Jelfs J, Ladhani SN, et al. The changing and dynamic epidemiology of meningococcal disease. Vaccine. 2012;30 Suppl 2:B26-36. [44] Teyssou R, Muros-Le Rouzic E. Meningitis epidemics in Africa: a brief overview. Vaccine. 2007;25 Suppl 1:A3-7. [45] Team HI. The epidemiology of meningococcal disease in New Zealand 2008-2013. Meningococcal Disease Reports: Institute of Environmental Science and Research Limited; 2014. [46] Wang X, Shutt KA, Vuong JT, Cohn A, MacNeil J, Schmink S, et al. Changes in the Population Structure of Invasive Neisseria meningitidis in the United States After Quadrivalent Meningococcal Conjugate Vaccine Licensure. J Infect Dis. 2015. [47] Meningococcal Reference U, Gray SJ, Trotter CL, Ramsay ME, Guiver M, Fox AJ, et al. Epidemiology of meningococcal disease in England and Wales 1993/94 to 2003/04: contribution and experiences of the Meningococcal Reference Unit. J Med Microbiol. 2006;55:887-96. [48] Funk A, Uadiale K, Kamau C, Caugant DA, Ango U, Greig J. Sequential outbreaks due to a new strain of Neisseria meningitidis serogroup C in northern Nigeria, 2013-14. PLoS currents. 2014;6. [49] Sorhouet-Pereira C, Efron A, Gagetti P, Faccone D, Regueira M, Corso A, et al. Phenotypic and genotypic characteristics of Neisseria meningitidis disease-causing strains in Argentina, 2010. PloS One. 2013;8:e58065. [50] Harrison LH, Jolley KA, Shutt KA, Marsh JW, O'Leary M, Sanza LT, et al. Antigenic shift and increased incidence of meningococcal disease. J Infect Dis. 2006;193:1266-74. [51] Hedberg ST, Toros B, Fredlund H, Olcen P, Molling P. Genetic characterisation of the emerging invasive Neisseria meningitidis serogroup Y in Sweden, 2000 to 2010. Euro Surveillance : Bulletin Europeen sur les Maladies Transmissibles = European Communicable Disease Bulletin. 2011;16. [52] Broker M, Jacobsson S, Kuusi M, Pace D, Simoes MJ, Skoczynska A, et al. Meningococcal serogroup Y emergence in Europe: update 2011. Human vaccines & immunotherapeutics. 2012;8:190711. [53] Materu S, Cox HS, Isaakidis P, Baruani B, Ogaro T, Caugant DA. Serogroup X in meningococcal disease, Western Kenya. Emerg Infect Dis. 2007;13:944-5. [54] Delrieu I, Yaro S, Tamekloe TA, Njanpop-Lafourcade BM, Tall H, Jaillard P, et al. Emergence of epidemic Neisseria meningitidis serogroup X meningitis in Togo and Burkina Faso. PloS One. 2011;6:e19513. [55] Stephens DS, Greenwood B, Brandtzaeg P. Epidemic meningitis, meningococcaemia, and Neisseria meningitidis. Lancet. 2007;369:2196-210. [56] Decosas J, Koama JB. Chronicle of an outbreak foretold: meningococcal meningitis W135 in Burkina Faso. The Lancet Infectious Diseases. 2002;2:763-5. [57] Mohammed I, Nasidi A, Alkali AS, Garbati MA, Ajayi-Obe EK, Audu KA, et al. A severe epidemic of meningococcal meningitis in Nigeria, 1996. Trans R Soc Trop Med Hyg. 2000;94:265-70. [58] Harrison LH. Vaccine prevention of meningococcal disease: making slow progress. Clin Infect Dis. 2006;43:1395-7. 25 [59] Kristiansen PA, Diomande F, Ba AK, Sanou I, Ouedraogo AS, Ouedraogo R, et al. Impact of the Serogroup A Meningococcal Conjugate Vaccine, MenAfriVac, on Carriage and Herd Immunity. Clin Infect Dis. 2012. [60] Maiden MC, Bygraves JA, Feil E, Morelli G, Russell JE, Urwin R, et al. Multilocus sequence typing: a portable approach to the identification of clones within populations of pathogenic microorganisms. Proc Natl Acad Sci U S A. 1998;95:3140-5. [61] Caugant DA. Population genetics and molecular epidemiology of Neisseria meningitidis. APMIS : Acta Pathologica, Microbiologica, et Immunologica Scandinavica. 1998;106:505-25. [62] Wang JF, Caugant DA, Morelli G, Koumare B, Achtman M. Antigenic and epidemiologic properties of the ET-37 complex of Neisseria meningitidis. J Infect Dis. 1993;167:1320-9. [63] Poolman JT, Lind I, Jonsdottir K, Froholm LO, Jones DM, Zanen HC. Meningococcal serotypes and serogroup B disease in north-west Europe. Lancet. 1986;2:555-8. [64] Caugant DA, Bol P, Hoiby EA, Zanen HC, Froholm LO. Clones of serogroup B Neisseria meningitidis causing systemic disease in The Netherlands, 1958-1986. J Infect Dis. 1990;162:867-74. [65] Whalen CM, Hockin JC, Ryan A, Ashton F. The changing epidemiology of invasive meningococcal disease in Canada, 1985 through 1992. Emergence of a virulent clone of Neisseria meningitidis. JAMA : the journal of the American Medical Association. 1995;273:390-4. [66] Pinner RW, Gellin BG, Bibb WF, Baker CN, Weaver R, Hunter SB, et al. Meningococcal disease in the United States--1986. Meningococcal Disease Study Group. J Infect Dis. 1991;164:368-74. [67] Caugant DA, Kristiansen PA, Wang X, Mayer LW, Taha MK, Ouedraogo R, et al. Molecular characterization of invasive meningococcal isolates from countries in the African meningitis belt before introduction of a serogroup A conjugate vaccine. PloS One. 2012;7:e46019. [68] Law DK, Lefebvre B, Gilca R, Deng S, Zhou J, De Wals P, et al. Characterization of invasive Neisseria meningitidis strains from Quebec, Canada, during a period of increased serogroup B disease, 2009-2013: phenotyping and genotyping with special emphasis on the non-carbohydrate protein vaccine targets. BMC Microbiol. 2015;15:143. [69] Neri A, Fazio C, Carannante A, Mastrantonio P, Stefanelli P. Diversity of Neisseria meningitidis invasive isolates in Italy in the period 2008-2010. J Prev Med Hyg. 2012;53:109-12. [70] Molling P, Backman A, Olcen P, Fredlund H. Comparison of serogroup W-135 meningococci isolated in Sweden during a 23-year period and those associated with a recent hajj pilgrimage. Journal of clinical microbiology. 2001;39:2695-9. [71] Massenet D, Inrombe J, Mevoula DE, Nicolas P. Serogroup W135 meningococcal meningitis, Northern Cameroon, 2007-2008. Emerg Infect Dis. 2009;15:340-2. [72] Nicolas P, Djibo S, Moussa A, Tenebray B, Boisier P, Chanteau S. Molecular Epidemiology of Meningococci Isolated in Niger in 2003 Shows Serogroup A Sequence Type (ST)-7 and Serogroup W135 ST-11 or ST-2881 Strains. Journal of clinical microbiology. 2005;43:1437-8. [73] Jolley KA, Brehony C, Maiden MC. Molecular typing of meningococci: recommendations for target choice and nomenclature. FEMS Microbiol Rev. 2007;31:89-96. [74] Harrison OB, Brueggemann AB, Caugant DA, van der Ende A, Frosch M, Gray S, et al. Molecular typing methods for outbreak detection and surveillance of invasive disease caused by Neisseria meningitidis, Haemophilus influenzae and Streptococcus pneumoniae, a review. Microbiology. 2011;157:2181-95. [75] Bash MC, Lesiak KB, Banks SD, Frasch CE. Analysis of Neisseria meningitidis class 3 outer membrane protein gene variable regions and type identification using genetic techniques. Infection and Immunity. 1995;63:1484-90. [76] Thompson EA, Feavers IM, Maiden MC. Antigenic diversity of meningococcal enterobactin receptor FetA, a vaccine component. Microbiology. 2003;149:1849-58. [77] Lemos AP, Brandao AP, Gorla MC, Paiva MV, Simonsen V, Melles CE. Phenotypic characterization of Neisseria meningitidis strains isolated from invasive disease in Brazil from 1990 to 2001. J Med Microbiol. 2006;55:751-7. 26 [78] Koumare B, Ouedraogo-Traore R, Sanou I, Yada AA, Sow I, Lusamba PS, et al. The first large epidemic of meningococcal disease caused by serogroup W135, Burkina Faso, 2002. Vaccine. 2007;25 Suppl 1:A37-41. [79] Harrison LH, Shutt KA, Schmink SE, Marsh JW, Harcourt BH, Wang X, et al. Population structure and capsular switching of invasive Neisseria meningitidis isolates in the pre-meningococcal conjugate vaccine era--United States, 2000-2005. J Infect Dis. 2010;201:1208-24. [80] Kaufmann ME. Pulsed-field gel electrophoresis. Methods Mol Med. 1998;15:33-50. [81] Massenet D, Birguel J, Azowe F, Ebong C, Gake B, Lombart JP, et al. Epidemiologic pattern of meningococcal meningitis in northern Cameroon in 2007-2010: contribution of PCR-enhanced surveillance. Pathog Glob Health. 2013;107:15-20. [82] Fonkoua MC, Taha MK, Nicolas P, Cunin P, Alonso JM, Bercion R, et al. Recent increase in meningitis Caused by Neisseria meningitidis serogroups A and W135, Yaounde, Cameroon. Emerg Infect Dis. 2002;8:327-9. [83] Njanpop-Lafourcade BM, Parent du Chatelet I, Sanou O, Alonso JM, Taha MK. The establishment of Neisseria meningitidis serogroup W135 of the clonal complex ET-37/ST-11 as an epidemic clone and the persistence of serogroup A isolates in Burkina Faso. Microbes and Infection / Institut Pasteur. 2005;7:645-9. [84] Swartley JS, Marfin AA, Edupuganti S, Liu LJ, Cieslak P, Perkins B, et al. Capsule switching of Neisseria meningitidis. Proc Natl Acad Sci U S A. 1997;94:271-6. [85] Beddek AJ, Li MS, Kroll JS, Jordan TW, Martin DR. Evidence for capsule switching between carried and disease-causing Neisseria meningitidis strains. Infection and Immunity. 2009;77:2989-94. [86] Kelly D, Pollard AJ. W135 in Africa: origins, problems and perspectives. Travel Medicine and Infectious Disease. 2003;1:19-28. [87] Harrison OB, Bray JE, Maiden MC, Caugant DA. Genomic Analysis of the Evolution and Global Spread of Hyper-invasive Meningococcal Lineage 5. EBioMedicine. 2015;2:234-43. [88] Toros B, Hedberg ST, Unemo M, Jacobsson S, Hill DM, Olcen P, et al. Genome-Based Characterization of Emergent Invasive Neisseria meningitidis Serogroup Y Isolates in Sweden from 1995 to 2012. Journal of clinical microbiology. 2015;53:2154-62. [89] Jolley KA, Maiden MC. BIGSdb: Scalable analysis of bacterial genome variation at the population level. BMC Bioinformatics. 2010;11:595. [90] Lucidarme J, Hill DM, Bratcher HB, Gray SJ, du Plessis M, Tsang RS, et al. Genomic resolution of an aggressive, widespread, diverse and expanding meningococcal serogroup B, C and W lineage. The Journal of Infection. 2015. [91] Mustapha MM MJ, Fernandez JO, de Lemos APS, Wang X, Mayer LW, Harrison LH. Capsular Switching and Global Spread of Neisseria Meningitidis Serogroup W, ST-11. International Pathogenic Neisseria Conferences, IPNC. Asheville, North Carolina, USA: IPNC; 2014. [92] Pajon R, Fergus AM, Koeberling O, Caugant DA, Granoff DM. Meningococcal factor H binding proteins in epidemic strains from Africa: implications for vaccine development. PLoS Neglected Tropical Diseases. 2011;5:e1302. [93] Ispasanie E, Pluschke G, Hodgson A, Sie A, MacLennan C, Koeberling O. Characterization of vaccine antigens of meningococcal serogroup W isolates from Ghana and Burkina Faso from 2003 to 2009. F1000Res. 2014;3:264. [94] Tsang RS, Hoang L, Tyrrell G, Horsman G, Wylie J, Jamieson FB, et al. Genetic and antigenic characterization of Canadian invasive Neisseria meningitidis serogroup C (MenC) case isolates in the post-MenC conjugate vaccine era, 2009-2013. J Med Microbiol. 2015;64:174-9. [95] Jackson LA, Wenger JD. Laboratory-based surveillance for meningococcal disease in selected areas, United States, 1989-1991. MMWR CDC Surveill Summ. 1993;42:21-30. [96] Rosenstein NE, Perkins BA, Stephens DS, Lefkowitz L, Cartter ML, Danila R, et al. The changing epidemiology of meningococcal disease in the United States, 1992-1996. J Infect Dis. 1999;180:1894901. 27 [97] Squires SG, Deeks SL, Tsang RS. Enhanced surveillance of invasive meningococcal disease in Canada: 1 January, 1999, through 31 December, 2001. Can Commun Dis Rep. 2004;30:17-28. [98] Ringuette L, Lorange M, Ryan A, Ashton F. Meningococcal infections in the Province of Quebec, Canada, during the period 1991 to 1992. Journal of clinical microbiology. 1995;33:53-7. [99] Hansman D. Meningococcal disease in South Australia: incidence and serogroup distribution 19711980. J Hyg (Lond). 1983;90:49-54. [100] Munro R, Dorman D, Daley D, Tomlinson P. Meningococcal serogroups in New South Wales, 1977-1987. Med J Aust. 1988;149:360-2. [101] de Marie S, Poolman JT, Hoeijmakers JH, Bol P, Spanjaard L, Zanen HC. Meningococcal disease in The Netherlands, 1959-1981: the occurrence of serogroups and serotypes 2a and 2b of Neisseria meningitidis. The Journal of Infection. 1986;12:133-43. [102] Spanjaard L, Bol P, de Marie S, Zanen HC. Association of meningococcal serogroups with the course of disease in the Netherlands, 1959-83. Bull World Health Organ. 1987;65:861-8. [103] Scholten RJ, Bijlmer HA, Poolman JT, Kuipers B, Caugant DA, Van Alphen L, et al. Meningococcal disease in The Netherlands, 1958-1990: a steady increase in the incidence since 1982 partially caused by new serotypes and subtypes of Neisseria meningitidis. Clin Infect Dis. 1993;16:23746. [104] Tyski S, Grzybowska W, Lind I. Active surveillance of meningococcal meningitis in Poland. Cent Eur J Public Health. 1998;6:219-24. [105] Salmaso S, Mastrantonio P, Scuderi G, Congiu ME, Stroffolini T, Pompa MG, et al. Pattern of bacterial meningitis in Italy, 1994. Eur J Epidemiol. 1997;13:317-21. [106] Mastrantonio P, Stefanelli P, Fazio C, Sofia T, Neri A, La Rosa G, et al. Serotype distribution, antibiotic susceptibility, and genetic relatedness of Neisseria meningitidis strains recently isolated in Italy. Clin Infect Dis. 2003;36:422-8. [107] Peltola H, Jonsdottir K, Lystad A, Sievers CJ, Kallings I. Meningococcal disease in Scandinavia. Br Med J (Clin Res Ed). 1982;284:1618-21. [108] Kremastinou J, Tzanakaki G, Kansouzidou A, Pagalis A, Danielides V, Kouppari G, et al. Recent emergence of serogroup C meningococcal disease in Greece. FEMS Immunol Med Microbiol. 1999;23:49-55. [109] Grahlow WD, Ocklitz HW, Mochmann H. Meningococcal infections in the German Democratic Republic 1971-1984. Infection. 1986;14:286-8. [110] Fallon RJ, Brown WM, Lore W. Meningococcal infections in Scotland 1972-82. J Hyg (Lond). 1984;93:167-80. [111] Denis F, Rey JL, Amadou A, Saliou P, Prince-David M, M'Boup S, et al. Emergence of meningococcal meningitis caused by W 135 subgroup in Africa. Lancet. 1982;2:1335-6. [112] Greenwood BM, Smith AW, Hassan-King M, Bijlmer HA, Shenton FC, Hughes AS, et al. The efficacy of meningococcal polysaccharide vaccine in preventing group A meningococcal disease in The Gambia, West Africa. Trans R Soc Trop Med Hyg. 1986;80:1006-7. [113] Kwara A, Adegbola RA, Corrah PT, Weber M, Achtman M, Morelli G, et al. Meningitis caused by a serogroup W135 clone of the ET-37 complex of Neisseria meningitidis in West Africa. Trop Med Int Health. 1998;3:742-6. [114] Chiou CS, Liao JC, Liao TL, Li CC, Chou CY, Chang HL, et al. Molecular epidemiology and emergence of worldwide epidemic clones of Neisseria meningitidis in Taiwan. BMC Infectious Diseases. 2006;6:25. [115] Raja NS, Parasakthi N, Puthucheary SD, Kamarulzaman A. Invasive meningococcal disease in the University of Malaya Medical Centre, Kuala Lumpur, Malaysia. J Postgrad Med. 2006;52:23-9; discussion 9. [116] Pancharoen C, Hongsiriwon S, Swasdichai K, Puthanakit T, Tangsathapornpong A, Lolekha S, et al. Epidemiology of invasive meningococcal disease in 13 government hospitals in Thailand, 1994-1999. Southeast Asian J Trop Med Public Health. 2000;31:708-11. 28 [117] El Bushra HE, Hassan NM, Al-Hamdan NA, Al-Jeffri MH, Turkistani AM, Al-Jumaily A, et al. Determinants of case fatality rates of meningococcal disease during outbreaks in Makkah, Saudi Arabia, 1987-97. Epidemiol Infect. 2000;125:555-60. [118] Yousuf M, Nadeem A. Meningococcal infection among pilgrims visiting Madinah Al-Munawarah despite prior A-C vaccination. J Pak Med Assoc. 2000;50:184-6. [119] Lingappa JR, Al-Rabeah AM, Hajjeh R, Mustafa T, Fatani A, Al-Bassam T, et al. Serogroup W135 meningococcal disease during the Hajj, 2000. Emerg Infect Dis. 2003;9:665-71. [120] Klena JD, Wasfy MO, Nada RA, Ahmed SF, Maksoud MA, Marfin A, et al. Characterization of Neisseria meningitidis isolates from Egypt using multilocus sequence typing. Trans R Soc Trop Med Hyg. 2012;106:309-14. [121] Dagan R, Isaachson M, Lang R, Karpuch J, Block C, Amir J. Epidemiology of pediatric meningitis caused by Haemophilus influenzae type b, Streptococcus pneumoniae, and Neisseria meningitidis in Israel: a 3-year nationwide prospective study. Israeli Pediatric Bacteremia and Meningitis Group. J Infect Dis. 1994;169:912-6. [122] Husain EH, Barakat M, Al-Saleh M. Trends and variations in the epidemiology of meningococcal disease in Kuwait 1987-2013. J Infect Public Health. 2015;8:441-7. [123] Aguilera JF, Perrocheau A, Meffre C, Hahne S, Group WW. Outbreak of serogroup W135 meningococcal disease after the Hajj pilgrimage, Europe, 2000. Emerg Infect Dis. 2002;8:761-7. [124] Meningococcal disease, serogroup W 135. Wkly Epidemiol Rec. 2000;75:173-80. [125] Meningococcal disease, serogroup W135 (update). Wkly Epidemiol Rec. 2001;76:213-4. [126] Memish ZA, Shibl AM. Consensus building and recommendations based on the available epidemiology of meningococcal disease in Gulf Cooperation Council States. Travel Medicine and Infectious Disease. 2011;9:60-6. [127] Ceyhan M, Gurler N, Ozsurekci Y, Keser M, Aycan AE, Gurbuz V, et al. Meningitis caused by Neisseria Meningitidis, Hemophilus Influenzae Type B and Streptococcus Pneumoniae during 2005-2012 in Turkey. A multicenter prospective surveillance study. Hum Vaccin Immunother. 2014;10:2706-12. [128] Taha MK, Parent Du Chatelet I, Schlumberger M, Sanou I, Djibo S, de Chabalier F, et al. Neisseria meningitidis serogroups W135 and A were equally prevalent among meningitis cases occurring at the end of the 2001 epidemics in Burkina Faso and Niger. Journal of clinical microbiology. 2002;40:1083-4. [129] Meningitis in Chad, Niger and Nigeria: 2009 epidemic season. Wkly Epidemiol Rec. 2010;85:4763. [130] Kristiansen PA, Ba AK, Sanou I, Ouedraogo AS, Ouedraogo R, Sangare L, et al. Phenotypic and genotypic characterization of meningococcal carriage and disease isolates in Burkina Faso after mass vaccination with a serogroup a conjugate vaccine. BMC Infectious Diseases. 2013;13:363. [131] Njanpop-Lafourcade BM, Hugonnet S, Djogbe H, Kodjo A, N'Douba A K, Taha MK, et al. Mobile microbiological laboratory support for evaluation of a meningitis epidemic in Northern Benin. PloS One. 2013;8:e68401. [132] Forgor AA, Leimkugel J, Hodgson A, Bugri A, Dangy JP, Gagneux S, et al. Emergence of W135 meningococcal meningitis in Ghana. Trop Med Int Health. 2005;10:1229-34. [133] Meningitis in Burkina Faso, Chad, Niger, Nigeria and Ghana: 2010 epidemic season. Wkly Epidemiol Rec. 2011;86:143-51. [134] Gamougam K, Daugla DM, Toralta J, Ngadoua C, Fermon F, Page AL, et al. Continuing effectiveness of serogroup A meningococcal conjugate vaccine, Chad, 2013. Emerg Infect Dis. 2015;21:115-8. [135] Coulson GB, von Gottberg A, du Plessis M, Smith AM, de Gouveia L, Klugman KP, et al. Meningococcal disease in South Africa, 1999-2002. Emerg Infect Dis. 2007;13:273-81. [136] Ibarz-Pavon AB, Morais L, Sigauque B, Mandomando I, Bassat Q, Nhacolo A, et al. Epidemiology, molecular characterization and antibiotic resistance of Neisseria meningitidis from patients </=15 years in Manhica, rural Mozambique. PloS One. 2011;6:e19717. [137] Abad R, Lopez EL, Debbag R, Vazquez JA. Serogroup W meningococcal disease: global spread and current affect on the Southern Cone in Latin America. Epidemiol Infect. 2014;142:2461-70. 29 [138] Weidlich L, Baethgen LF, Mayer LW, Moraes C, Klein CC, Nunes LS, et al. High prevalence of Neisseria meningitidis hypervirulent lineages and emergence of W135:P1.5,2:ST-11 clone in Southern Brazil. The Journal of Infection. 2008;57:324-31. [139] Li YA, Tsang R, Desai S, Deehan H. Enhanced surveillance of invasive meningococcal disease in Canada, 2006-2011. Canada Communicable Disease Report CCDR. 2014;40. [140] Antignac A, Ducos-Galand M, Guiyoule A, Pires R, Alonso JM, Taha MK. Neisseria meningitidis strains isolated from invasive infections in France (1999-2002): phenotypes and antibiotic susceptibility patterns. Clin Infect Dis. 2003;37:912-20. [141] Vicente D, Esnal O, Marimon JM, Gastesi C, Perez-Trallero E. Neisseria meningitidis W-135 in the Basque Country, northern Spain. Clin Microbiol Infect. 2006;12:812-5. [142] Stefanelli P, Fazio C, Neri A, Boros S, Renna G, Pompa MG, et al. Changing epidemiology of Infant Meningococcal Disease after the introduction of meningococcal serogroup C vaccine in Italy, 2006-2014. Vaccine. 2015;33:3678-81. [143] Bechini A, Levi M, Boccalini S, Tiscione E, Balocchini E, Canessa C, et al. Impact on disease incidence of a routine universal and catch-up vaccination strategy against Neisseria meningitidis C in Tuscany, Italy. Vaccine. 2012;30:6396-401. [144] Wilder-Smith A, Chow A, Goh KT. Emergence and disappearance of W135 meningococcal disease. Epidemiol Infect. 2010;138:976-8. [145] He B, Jia Z, Zhou H, Wang Y, Jiang X, Ma H, et al. CC4821 serogroup W meningococcal disease in China. Int J Infect Dis. 2014;29:113-4. [146] Devasena N PV. Neiserria Meningitis Due to W135 Strain from South India. Journal of Infectious Diseases and Therapy. 2014;02. [147] Hayakawa K, Itoda I, Shimuta K, Takahashi H, Ohnishi M. Urethritis caused by novel Neisseria meningitidis serogroup W in man who has sex with men, Japan. Emerg Infect Dis. 2014;20:1585-7. [148] Jo YM, Bae SM, Kang YH. Cluster of serogroup W-135 meningococcal disease in 3 military recruits. J Korean Med Sci. 2015;30:662-5. [149] Health AGDo. Australian Meningococcal Surveillance Programme annual reports. 2014. [150] Moore PS, Reeves MW, Schwartz B, Gellin BG, Broome CV. Intercontinental spread of an epidemic group A Neisseria meningitidis strain. Lancet. 1989;2:260-3. [151] Mueller JE, Borrow R, Gessner BD. Meningococcal serogroup W135 in the African meningitis belt: epidemiology, immunity and vaccines. Expert Rev Vaccines. 2006;5:319-36. [152] Boisier P, Nicolas P, Djibo S, Taha MK, Jeanne I, Mainassara HB, et al. Meningococcal meningitis: unprecedented incidence of serogroup X-related cases in 2006 in Niger. Clin Infect Dis. 2007;44:657-63. 30