Assessing Borderline Personality Disorder in the Primary Care Setting Date: 11/13/2014
advertisement

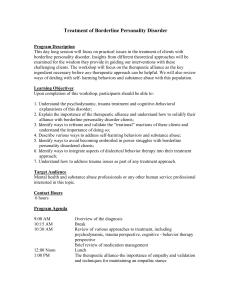
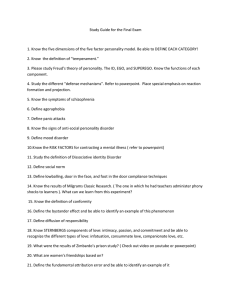
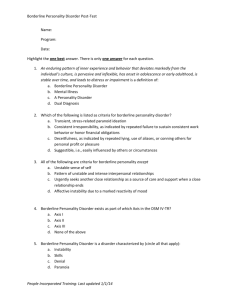
Assessing Borderline Personality Disorder in the Primary Care Setting Presented by: Jonathan Betlinski, MD Date: 11/13/2014 Disclosures and Learning Objectives • Learning Objectives – – – Be able to list the diagnostic criteria for Borderline Personality Disorder Know at least 3 mental health comorbidities of BPD Know at least 3 physical health comorbidities of BPD Disclosures: Dr. Jonathan Betlinski has nothing to disclose. Assessing Borderline Personality Disorder • • • • • Review epidemiology Review mental health comorbidities Review physical health comorbidities Review Prognosis Review diagnostic criteria • Next Week's Topic Borderline Personality Disorder • 1-4% of the general population • 8-27% in outpatient mental health (15-51% inpatient) • 6% of a primary care clinic population (or 26%???) – 21% current suicidal ideation – 21% Bipolar Disorder – 36% Major Depressive Disorder – 57% Anxiety Disorder – 50% had no mental health treatment that year – 43% not recognized by PCP has having any emotional or mental health problems. http://archinte.jamanetwork.com/article.aspx?articleID=210746 Borderline Personality Disorder Co-Occurs • 60% have MDD • 70% have Dysthymic Disorder • 25% have Eating Disorders • 35% meet criteria for Substance Abuse • 15% Bipolar Disorder • 25% Antisocial Personality Disorder • 25% Narcissistic Personality Disorder • Up to 80% have suicidal behaviors • 4-9% die from suicide http://www.nimh.nih.gov/health/publications/borderline-personalitydisorder/Borderline_Personality_Disorder_508_141959.pdf http://www.nami.org/Template.cfm?Section=By_Illness&Template=/TaggedPage/TaggedPageDisplay.cfm&TPLID=54& Borderline Personality Disorder • Higher rates of common health problems – – – – – • Diabetes Hypertension Chronic Back Pain Arthritis Fibromyalgia May be due to medication-induced obesity http://www.nimh.nih.gov/health/publications/borderline-personalitydisorder/Borderline_Personality_Disorder_508_141959.pdf Borderline Personality Disorder • • • • • • Fewer PCP visits per year Lower mental/emotional health ratings Similar physical health self-rating Much higher rates of hospitalization Much higher rates of mental health care Much higher rates of psychiatric medications http://archinte.jamanetwork.com/article.aspx?articleID=210746 Borderline Personality Disorder, Prognosis • • • • • • • First five years are most crisis-ridden 60% readmitted within the first 6 months 35% readmission in 18-24 months 40-50% remission in 2 years 85% remission in 10 years After remission, only 6% relapse 25% achieve social stability http://www.borderlinepersonalitydisorder.com/documents/A_BPD_Brief_REV2011.pdf http://www.nimh.nih.gov/health/publications/borderline-personalitydisorder/Borderline_Personality_Disorder_508_141959.pdf Borderline Personality Disorder, DSM-IV TR A pervasive pattern of instability of interpersonal relationships, self image, and affects, and marked impulsivity beginning by early adulthood and present in a variety of contexts, as indicated by 5 (or more) of the following: • Frantic efforts to avoid abandonment • A pattern of unstable, intense relationships • Identity disturbance • Impulsivity in potentially damaging areas • Recurrent suicidal behaviors • Chronic feelings of emptiness • Inappropriate intense anger or difficulty controlling anger • Transient paranoia or severe dissociative symptoms http://www.psi.uba.ar/academica/carrerasdegrado/psicologia/sitios_catedras/practicas_profesionales/820_clinica_tr_pe rsonalidad_psicosis/material/dsm.pdf Borderline Personality Disorder, DSM-5 Impairments in personality (self and interpersonal) functioning AND the presence of pathological personality traits. These criteria must be met: • Significant impairments in personality functioning • Impairments in self functioning (a or b) • Identity (unstable self image, chronic emptiness, dissociative states, self-criticism) • Self-direction (instability in goals, aspirations, values or career plans) • • AND Impairments in interpersonal functioning (a or b) • Empathy (and hypersensitivity) • Intimacy (intense, unstable, and conflicted close relationships, alternating extremes) Pathological Personality Traits in the following domains • Negative Affectivity, characterized by • Emotional lability • Anxiousness • Separation insecurity • Depressivity http://www.psi.uba.ar/academica/carrerasdegrado/psicologia/sitios_catedras/practicas_profesionales/820_clinica_tr_pe rsonalidad_psicosis/material/dsm.pdf Borderline Personality Disorder, DSM-5 • Disinhibition, characterized by • Impulsivity • Risk-taking • Antagonism, characterized by • Hostility • These impairments are relativity stable across time and consistent across situations • The impairments are not better understood as normative for developmental stage or socio-cultural environment • The impariments are not solely due to the direct physiologic effects of a substance or a general medical condition http://www.psi.uba.ar/academica/carrerasdegrado/psicologia/sitios_catedras/practicas_profesionales/820_clinica_tr_pe rsonalidad_psicosis/material/dsm.pdf Summary • Borderline Personality Disorder – – – • More common in Primary Care settings Commonly misunderstood Can disrupt care Borderline Personality Disorder – – Gets better! Accurate recognition increases chances for recovery http://www.nami.org/Template.cfm?Section=Borderline_Personality_Disorder_(BPD)&Template=/ContentManagement/ ContentDisplay.cfm&ContentID=81017 The End! Next Week's Topic: Treatment of Borderline Personality Disorder