Prognostic predictors of outcome in an operative series in traumatic... patients
advertisement

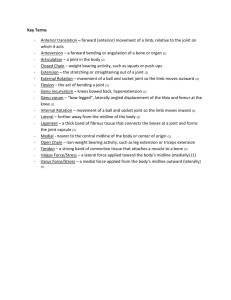
Prognostic predictors of outcome in an operative series in traumatic brain injury patients Running title: Prognostic predictors in traumatic brain injury Jinn-Rung, Kuo1, 2, 4, Che-Chuan, Wang 1, Chung-Ching, Chio1, Kao-Chang, Lin 3, 4 1 Institute of Clinical Medicine, School of Medicine, National Cheng-Kung University, Tainan, Taiwan; 2 Departments of Neurosurgery Chi-Mei Medical Center, Tainan, Taiwan 3 Departments of Neurology, Chi-Mei Medical Center, Tainan, Taiwan 4 Department of Biotechnology, Southern Taiwan University, Tainan, Taiwan; Corresponding author: Kao-Chang, Lin MD, Department of Neurology, Chi-Mei Medical Center, 901 Chung Hwa Road, Yung Kang City, Tainan, Taiwan 710 Tel: 886-6-2812811; Fax: 886-6-2828928 E-mail: kuo.ox@msa.hinet.net 1 Abstract Background/ Purpose: Although several prognostic factors for TBI have been evaluated, a useful predictive scoring model for outcome has yet been developed for TBI patients. The aim for this study, therefore, was to determine independent predictors and develop a multivariate logistic regression equation to determine prognosis in TBI patients. Methods: A total of 13 different variables were evaluated. All 84 patients in this study were retrospectively evaluated between October 2003 and January 2008 and all underwent craniectomy or craniotomy for haematoma removal and were fitted with intracranial pressure (ICP) microsensor monitors. By using univariate, multiple logistic regression and prognostic regression scoring equations it was possible to draw receiver-operating characteristic curves to predict Glasgow Outcome Scale (GOS) 6 months after TBI. Results: It was shown that older patients in particular those over 40 years of age, unresponsive pre-op pupil reaction, higher pre-op midline shift, higher injury severity score (ISS) and craniectomy were factors associated with poor outcome in patients with traumatic brain injury. Conclusions: These 5 variables can be used as independent predictors to predict the 6 months GOS in traumatic brain injury patients. Also, the five variables derived from multivariate logistic equation are clinically useful in predicting outcome in daily practice and act as a guideline in deciding whether or not to avoid performing decompressive craniectomy. Key words: traumatic brain injury, craniectomy, injury severity score, pupillary reaction, midline shift, prognositic factors 2 Introduction Traumatic brain injury (TBI), remains a critical public health challenge. 1 The annually TBIrelated death is 19.4 of 100,000 persons. 1 The prognosis of TBI can be predicted by a wide range of variables: age, neurological assessment (Glasgow coma scale), pupillary light reflex, injury severity score (ISS), 2 imaging study (degree of midline shift in computed tomography). 3-6 time elapsed from injury to surgery, 7 intra-operative cerebral perfusion pressure (CPP), 8 and whether or not the patient has undergone decompressive craniectomy. 9, 10 However, a useful outcome predictive scoring model has not been well established for TBI patients. The aim of this study is to determine independent predictors and develop a multivariate logistic regression equation to predict the prognosis in traumatic brain injury patients. These predictive variables are age, sex, injury severity score, neurological assessment, preoperative and postoperative imaging studies, and hemodynamic change during operation. Material and method Patients with TBI were retrospectively evaluated and enrolled from Oct 2003 to Jan 2008, in a medical center in southern Taiwan. This study was approved by the ethics committee of our hospital. A complete history was taken and a neurological assessment was performed on each patient. All patients received neuroimaging with computerized tomography (CT) and were evaluated for the initial GCS in the emergency room. They all underwent craniectomy or craniotomy for haematoma removal and an intracranial pressure (ICP) microsensor (Codman and Shurtlef, Inc., Rayman, MA, USA) was placed in the parenchyma of the ipsilateral frontal lobe of each patient. The key indications for craniectomy were as follows: a thickness of more than 1cm in cases of extracerebral hematoma and a volume more than 30 ml in cases of intracerebral hematoma, 3 a deviation of supratentorial midline shift > 5mm with lateral ventricle compression, disappearance of the basal cistern, and clinical aggravation. The mean arterial blood pressure (MAP) was monitored using standard pressure transducers. Cerebral perfusion pressure (CPP), cerebral circulatory-pressure index (CCPI) 11 and MAP values were recorded when the scalp was closed. Postoperatively, patients underwent CPP-guided management, with the aim of obtaining a CPP of 60 mmHg or more and ICP of 25 mmHg or less. The relationship between age, sex, injury severity score (ISS), admission Glasgow coma scale (GCS), preoperative GCS, preoperative brain CT midline shift, time interval from injury to operation, the values of MAP, ICP, CPP, and CCPI when scalp was closed, postoperative midline shift, postoperative cerebral infarction and Glasgow outcome score (GOS) at 6 months after TBI were evaluated. The midline shift on the CT scan was defined as the absolute distance (mm) that the septum pellucidum of the brain was displaced away from the midline, which was determined as an average by calculating the distance between both inner tables inside the skull.12 For convenience of data analysis, the presence of a fixed pupil was defined as unresponsive (<1 mm) to a light stimulus. The pupillary light reflex was divided into three categories including one pupil fixed, both pupils fixed and both pupils reactive. Time elapsed between injury and surgery was classified as very early surgery (less than 6 hours after injury), early surgery (between 6 and 24 hours) and late surgery (after 24 hours). The outcome of the patients at 6 months after injury was categorized according to the Glasgow outcome scale as: (1) death; (2) persistent vegetative state; (3) severe disability (conscious but disabled); (4) moderate disability (disabled but independent) and (5) good 4 recovery.13 A score of 4 to 5 was considered a favorable outcome (moderate disability or less) and a score of 1 to 3 was considered unfavorable (severe disability or death). Data were expressed as a mean ± standard deviation in some items. Student’s t-test, or chisquare test were used to assess statistical significance among all groups. Multiple logistic regression models were used for correlation between two continuous or categorical variables and the independent risk factors for poor outcome defined. Finally, logistic regression analysis was then used to establish a prognostic model and a receiver-operating characteristic curve 14 was then drawn based on the prognostic scoring model All data were analyzed using qualified statistical software (SPSS for Windows, Version 16, SPSS Inc., Chicago, Illinois, USA). A P-value of less than 0.05 was considered significant. Results In total, 84 traumatic brain injury patients were retrospectively evaluated. Traffic accidents had occurred in 74.0% of the cases. The mean age of the 84 patients (56 male and 28 female) was 40.8±18.6 years (range, 12–78 years). Male patients were significantly predominant at 66.7%. There were subdural hemorrhages in 52.4 % of the cases, epidural hemorrhages in 8.3 %, intracranial hematomas in 11.9 %, and mixed hemorrhages in 15.4 %. The average ISS was 27± 4.1. The overall 6 months GOS was 3.0±1.7. Patients and their clinical characteristics are summarized in Table 1. Table 2 shows that age (P<0.001), admission GCS (P<0.001), preoperative GCS (P<0.001), preoperative midline shift (P<0.001), postoperative midline shift (P<0.001), and ISS (P=0.005) were significantly associated with GOS at 6 months after injury by using student’s t-test for continuous variables. When chi-square or Fisher's exact statistics were used for categorical variables, it showed that pre-op pupil reaction (P <0.001), time interval from injury to 5 operation (P=0.002) and craniectomy (P=0.005) were significantly associated with 6 months GOS (Table 3). Multivariate logistic regression was then performed on the significant variables extracted from the previous step to determine the independent association of each variable with GOS at 6 months after injury. Thus, the final model contained five variables: age, pupil reaction, ISS, preoperative midline shift and decompressive craniectomy. These results showed age (OR= 1.12, CI= 1.05-1.19, P<0.001), pupil reaction (OR= 78.68, CI= 6.39-968.6, P= 0.001), preoperative midline shift (OR= 16.17, CI= 2.07-126.39, P=0.008), ISS (OR= 1.48, CI= 1.111.97, P=0.007) and craniectomy ([OR= 1.19, CI= 1.0-1.42, P<0.05) were independent of associations to GOS (Table 4). At the same time, a predicted probability (P) of having an unfavorable outcome was estimated by the multiple logistic regression model: Ln(P/1-P) = -19.86 + 2.78 x (craniectomy or craniotomy) + 0.11x (age in years) + 4.37x (pupil reaction) + 0.17x (preoperative midline shift in mm) + 0.39 x (ISS). The predictors of the model were selected by stepwise procedure. Using the receiver operating characteristic curve analysis (ROC) based on the prognostic model scoring, a cut point for prediction to an unfavorable outcome of P was defined as a value >=0.6. The equation’ sensitivity was 97.5%, and specificity 90.7% in predicting the unfavorable outcome at 6 months after TBI (AUC=0.96, 95% confidence interval 0.91-1.00) (Figure 1). Discussion A significant relationship between age and post-traumatic outcome has been reported.15, 16 Ono et al have demonstrated 15 in patients fewer than 40 years of age, the percentage of good outcome ranged from 33.9% to 48.7% in different lesions. On the other hand, poor outcome 6 ranging from 66.7% to 94.4% was predominant in patients over 40 years of age. In our study, in univariate analysis, the result showed age 32.6 ± 15.1 years in favorable and 48.5 ± 18.3 years in unfavorable outcome (P <0.001)). By multiple logistic regression models, the adjusted odd ratio (OR) in predicting the poor outcome was significant with age (OR= 1.12, CI= 1.05-1.19, P<0.001). In subgroup analysis, patients under 40 years of age, the percentage of good outcome was 67.5%. On the other hand, poor outcome was 70.5% in patients over 40 years of age. Our results revealed that age is an independent predictor to GOS in traumatic brain injury, which is consistent with the previous reports. Pupil reactivity to light stimulus correlated to outcomes that have been reported in several reports. Bilaterally absent pupillary light reflex was associated with a 56–90% mortality.17 Kuo et al demonstrated pupil reactivity to light has the most significant correlation with GOS (ρ= 0.727, P < 0:0001) when compared with coagulopathy and midline shift. It is believed that most patients classified as having both pupils fixed would have very poor outcome. 18 However, Carter et al reported that nearly 20% of patients with bilaterally absent pupillary response had favorable outcomes in a study of 89 cases. 19 The present study reveals the percentage of unfavorable outcome was 28.6% in both reactive pupils, 52.6% in one fixed pupil and 91.3% in both fixed pupils (P< 0.001). Table 4 disclosed the adjusted odd ratio (OR= 78.68, CI= 6.39-968.6, P= 0.001) in both fixed pupils versus at least one reactive pupil. These results were consistent to previous reports. In the subgroup analysis, 95% (GOS 1 30%, GOS 2+3 65%) unfavorable outcomes occurred in patients with unresponsive pupillary reaction in both pupils when undergoing life saving decompressive craniectomy. From our results, we recommended avoiding decompressive craniectomy procedure in such cases, because there is only very little benefit to neurologic status. 7 The prognosis of TBI can be predicted by GCS has been reported. 20 However, in our study, by multiple logistic regression modle, it disclosed that GCS is not independent predictor to GOS. In the subgroup analysis, we dichotomized preoperative GCS to binary variable by cut point 6, it revealed significantly correlated to favorable / unfavorable outcome (P < 0.001, chi-square test). Furthermore, GCS was also strongly correlated to pupil reaction (P < 0.001, chi-square test). Base on the strong correlation between GCS and pupil reaction finding, in model selection procedure, pupil reaction rather than GCS was selected into multiple regression analysis. The distance of brain CT midline shift is generally considered to indicate the severity of injury and has a risk factor with poor outcome. 21 Mass et al showed midline shift (1-5 mm, OR 1.36; CI 1.09-1.68; > 5mm, OR 2.20; CI 1.64-2.96) were strongly related to poor outcome. However, Lin et al contradicted it with results of (distance of midline shift ≧5 Vs < 5 mm, OR 2.63; CI 6.0-43.67, P=0.499). 22 In the present study, the results revealing poor outcome was significant with a preoperative midline shift on brain CT (OR= 1.19, CI= 1.001.42, P= 0.050). This discrepancy might be due to the existence of another independent factor which plays a more important role than midline shift but is in someway strongly correlated to it. However, in our study, results support the concept that the distance of brain CT midline shift is an index for severity of injury and is a risk factor for poor outcome. Injury severity score (ISS) is an index of overall severity useful for persons sustaining multiple injuries 2; and is one of the most important factors in predicting outcome after acute head injury.4 However, Ucar et al has not supported the idea.24 In our study, the result showed ISS 26.1± 2.7 for favorable and 28.6±4.8 for unfavorable outcomes (p=0.005). By multiple logistic regression models, the adjusted odd ratio (OR) in predicting the poor outcome was significant with ISS (OR= 1.48, CI= 1.11-1.97, P=0.007).This result provided 8 other evidence to support the idea that patients with a higher ISS would be at higher risk for secondary brain insult. This result also implies that no injuries in a primary and secondary survey for the trauma team in an emergency room should be overlooked because these extracranial insults could lead to irreversible secondary brain damage. Decompressive craniectomy has been historically considered a salvage procedure in TBI. Skoglund et al24 showed 68% patients of TBI had favorable outcome. However, Jiang et al showed 60.2% and Ucar et al 23 25 indicated 84% of patients’ experienced unfavorable outcome after decompressive craniectomy. In our study, the overall mortality rate and unfavorable outcome in craniectomy patients was 33.3% and 62.7% respectively. When comparing craniectomy with craniotomy patients, it shows craniectomy patients have a lower preoperative GCS (P=0.012); more unresponsive pupil reaction (P=0.013); higher ICP (P=0.001), lower CPP (P=0.011) and lower CCPI (P<0.001) when the scalp was closed, and higher postoperative cerebral infarction (P=0.037). These results seem to support the notion that the perioperative neurological status in decompressive craniectomy patients is more severe than in craniotomy. These results might explain why patients who underwent craniectomy in our study will lead to poor outcome and craniectomy is an independent predictive variable in GOS after TBI. To avoid under or over-estimated causal – effect relationships in univariate analysis resulting from confounders, multiple logistic regression model was performed to estimate the adjusted odd ratio. Craniectomy rather than craniotomy was more likely to get an unfavorable outcome after adjustment for age, pupil reaction, preoperative midline shift and ISS. In addition to the single factor analysis and multi-factorial prognostic analysis, in our study, we further combined an ROC curve and the multivariate logistic regression equation to evaluate the predictive accuracy of five variables in GOS. These results disclosed all five 9 variables, which had previously been shown to be related to survival, had strong accuracy in prognostic judgment with sensitivity 97.5% and specificity 90.7% in GOS. Since these five variables in the scoring model are clinically simple to attain in the acute stage after TBI, we consider therefore, that the derived equation is clinically useful to predict outcome in daily practice. There are limitations to these results because of the nature of the retrospective design. One of our significant findings from our study is patients with craniectomy rather than craniotomy were more likely to get an unfavorable outcome after adjustment for age, pupil reaction, preoperative midline shift and ISS. Clearly, the strategy of surgical procedure may be affected by experience of surgeons and patients’ condition. This issue needs to be addressed in prospective studies. Another limitation of this study is small sample size and heterogeneity of the patient population. Actually, the different types of TBI such as epidural hematoma, subdural hematoma and contusion hemorrhage have different outcomes. In our study, there were subdural hemorrhages in 52.4 % of the cases, epidural hemorrhages in 8.3 %, intracranial hematoma in 11.9 %, and mixed hemorrhages in 15.4 %. However, in our study, the outcome predictors such as age, sex, injury severity score, neurological assessment, preoperative and postoperative imaging studies, and hemodynamic change during operation are all important factors in any types of brain insults. In general, it seems reasonable to group these patients together. However, the subgroup analysis of an enriched population of different types of hemorrhage patients is needed to clarify the issue. Conclusions 10 Based on our findings, we conclude that the five factors; old age, unresponsive pre-op pupil reaction, higher pre-op midline shift, higher ISS and underwent craniectomy are factors associated with poor outcome in patients with traumatic brain injury. They can be used as independent predictors in assessing the 6-month GOS in traumatic brain injury patients. The five variables derived multivariate logistic equation is clinically useful to predict outcome in daily practice also. 11 References 1. Adekoya N, Thrurman DJ, White DD, et al: Surveillance for traumatic brain injury death – United states, 1989-1998. MMWR Surveill Summ 2002;51:1-14. 2. Baker SP, O’Neill B, Haddon W, et al. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 1974;14:187-96. 3. Eisenberg HM, Gary Jr HE, Aldrich EF et al. Initial CT findings in 753 patients with severe head head injury. A report from the NIH traumatic coma data bank. J Neurosurg 1990; 73: 688–98. 4. Signorini DF, Andrews PJ, Jones PA, et al. Predicting survival using simple clinical variables: a case study in traumatic brain injury. J Neurol Neurosurg Psychiatry 1999; 66:20-5. 5. Marshall LF, Gautille T, Klauber M et al. The outcome of severe closed head injury. J Neurosurg 1991; 75: S28–S36. 6. Phuenpathom N, Choomuang M, Ratanalert S. Outcome and outcome prediction in acute subdura hematoma. Surg Neurol 1993; 40: 22–5. 7. Seeling JM, Becker DP, Miller JD, et al. Traumatic acute subdural hematoma: major mortality reduction in comatose patients treated within four hours. N Engl J Med 1981;304:1511-8. 8. Kuo JR, Yeh TC, Sung KC, et al. Intraoperative applications of intracranial pressure monitoring in patients with severe head injury. JClinNeurosci 2006;13:218–23. 9. Timofeev I, Czosnyka M, Nortje J, et al. Effect of decompressive craniectomy on intracranial pressure and cerebraospinal compensation following traumatic brain injury. J Neurosurg 2008;108:66-73. 10. Howard JL, Cipolle MD, Anderson M, et al. Outcome after decompressive craniectomy 12 for the treatment of severe traumatic brain injury. J Trauma 2008;65:380-6. 11. Wronski J, Juniewicz H, Mierzwa J, et al. The concept of cerebral circulatory-pressure index(CCPI). Neurol Neurochir Psychiatr Pol 2000;6;80-8 12. Lobato RD, Rivas JJ, Gomez PA, et al. Head injury patients who talk and deteriorate into coma. Analysis of 211 cases studies with computerized tomography. J Neurosurg 1991; 75: 256-61. 13. Jennett B, Bond M. Assessment of outcome after severe brain damage: a practical scale. Lancet 1975; 1: 480-4. 14. Zweig MH, Campbell G. Receiver-operating characteristic (ROC) plots: a fundamental evaluation tool in clinical practice. Clin Chem 1993;39:561-7. 15. Ono JI, Yamaura A, Kubotoo M, et al. Outcome prediction in severe head injury: analyses of clinical prognostic factors J Clin Neurosci 2001;8:120-3. 16. Mosenthal AC, Livingstone DH, Lavery RF. et al. The effect of age on functional outcome in mild traumatic brain injury: 6- month report of a prospective muiti-center trial. J Trauma 2004;56:1042-8. 17. Brain Trauma Foundation, American Association of Neurological Surgery, Joint section in Neurotrauma and Critical care: Pupillary diameter and light reflex. J Neurotrauma 2000; 17:583–90. 18. Kuo JR, Chou TJ, Chio CC. Coagulopathy as a parameter to predict the outcome in head injury patients – analysis of 61 cases. Journal Clini Neurosci2004; 11: 710–4. 19. Carter BG, Butt W, Taylor A. Bilaterally absent papillary response: not always a bad sign. Anaesth Intensive Care. 2007;35:984-7. 20. Balestreri M, Czosnyka M, Chatfield DA, et al. Predictive value of Glasgow coma scale after brain trauma: change in trend over the past ten years. J Neurol 13 Neurosurg Psychiatry 2004;75:161-2. 21. Mass AIR, Steyerberg EW, Butcher I, et al. Prognostic value of computerized tomography scan characteristics in traumatic brain injury: result from the IMPACT study. J Trauma 2007;24:303-4. 22. Kuo JR, Wang CC, Chang CH, et al. The correlation of high D-dimer level with poor outcome in traumatic intracranial hemorrhage. Eur J Neurol 2007;14:1073-8. 23. Ucar T, Akyuz M, Kazan S, et alo. Role of decompressive craniectomy surgery in the management of severe head injuries: prognostic factors and patient selection. J Neurotrauma. 2005;22:1311-8. 24. Skoglund TS, Eriksson-Ritzen C, Jensen C, et al. Aspects on decompressive craniectomy in patients with traumatic head injury. J Trauma 2006;23:1502-9. 25. Jiang JY, Xu W, Li WP. et al. Efficacy of standard trauma craniectomy for refractory intracranial hypertension with severe traumatic brain injury: a multicenter prospective, randomized controlled study. J Neurotrauma. 2005;22:623-8. 14 ACKNOWLEDGMENTS The authors wish to express their gratitude to all of the participants from neurology, neurosurgery, emergency critical medicine, and the intensive care unit. They also thank Ms. Lin, Wen-Chun for her help on the statistical analysis. 15