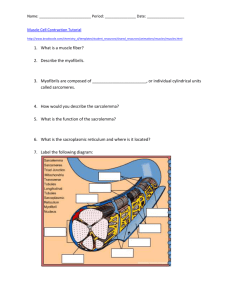
A. Anatomy of a whole muscle (many cells)-review on your... 1. Fascicles & endomysium- muscle cells ("fibers") are arranged in
advertisement
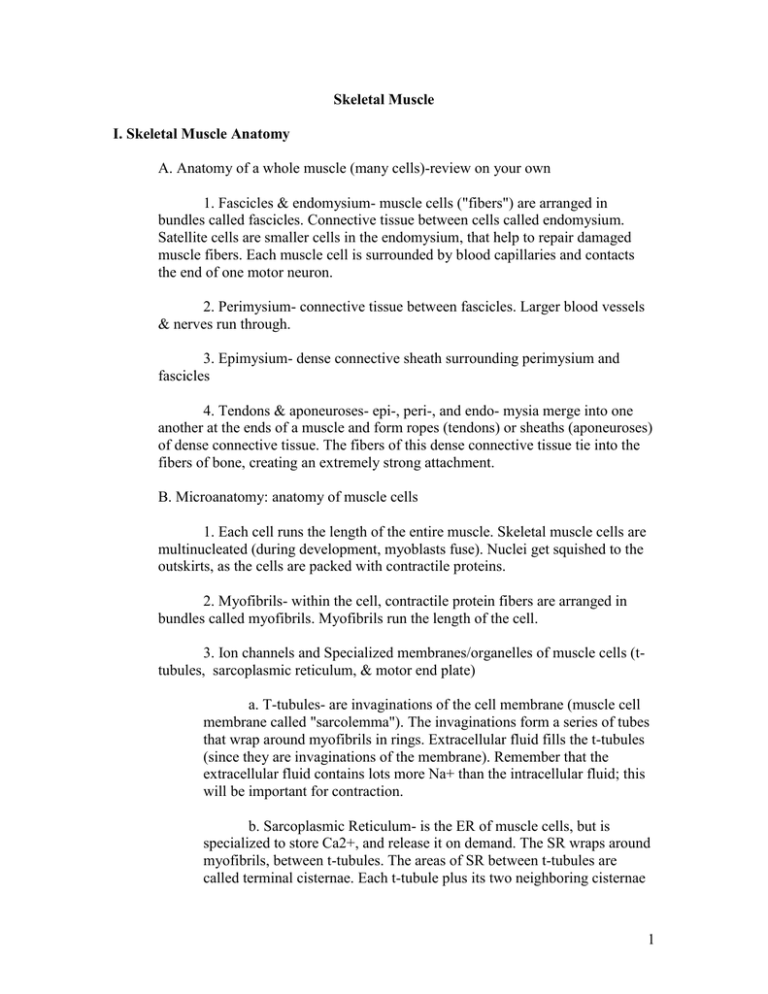
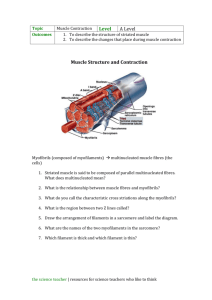
Skeletal Muscle I. Skeletal Muscle Anatomy A. Anatomy of a whole muscle (many cells)-review on your own 1. Fascicles & endomysium- muscle cells ("fibers") are arranged in bundles called fascicles. Connective tissue between cells called endomysium. Satellite cells are smaller cells in the endomysium, that help to repair damaged muscle fibers. Each muscle cell is surrounded by blood capillaries and contacts the end of one motor neuron. 2. Perimysium- connective tissue between fascicles. Larger blood vessels & nerves run through. 3. Epimysium- dense connective sheath surrounding perimysium and fascicles 4. Tendons & aponeuroses- epi-, peri-, and endo- mysia merge into one another at the ends of a muscle and form ropes (tendons) or sheaths (aponeuroses) of dense connective tissue. The fibers of this dense connective tissue tie into the fibers of bone, creating an extremely strong attachment. B. Microanatomy: anatomy of muscle cells 1. Each cell runs the length of the entire muscle. Skeletal muscle cells are multinucleated (during development, myoblasts fuse). Nuclei get squished to the outskirts, as the cells are packed with contractile proteins. 2. Myofibrils- within the cell, contractile protein fibers are arranged in bundles called myofibrils. Myofibrils run the length of the cell. 3. Ion channels and Specialized membranes/organelles of muscle cells (ttubules, sarcoplasmic reticulum, & motor end plate) a. T-tubules- are invaginations of the cell membrane (muscle cell membrane called "sarcolemma"). The invaginations form a series of tubes that wrap around myofibrils in rings. Extracellular fluid fills the t-tubules (since they are invaginations of the membrane). Remember that the extracellular fluid contains lots more Na+ than the intracellular fluid; this will be important for contraction. b. Sarcoplasmic Reticulum- is the ER of muscle cells, but is specialized to store Ca2+, and release it on demand. The SR wraps around myofibrils, between t-tubules. The areas of SR between t-tubules are called terminal cisternae. Each t-tubule plus its two neighboring cisternae 1 are considered a functional unit, called a triad. This is important because when t-tubules allow Na+ into the cell from extracellular fluid, that event causes the neighboring cisternae to release Ca2+. The release of Ca2+ from the cisternae will start a contraction. c. Motor end plate: area of the sarcoplasm. Here is where the terminals of motor neurons “talk” to muscle cells and tell them to contract. The neurons release neurotransmitters (specifically, acetylcholine: Ach) onto the muscle cell at the motor end plate. The motor end plate contains an abundance of chemically-gated ion channels: Na+ channels that open when Ach binds. d. Ion channels/pumps- as previously stated, the motor end plate contains an abundance of chemically-regulated Na+ channels. The rest of the sarcoplasm, including along the t-tubules, contains voltage-regulated Na+ channels. The sarcoplasmic reticulum contains voltage-regulated Ca2+ channels, and active transport Ca2+ pumps. These are the only types of channels we will consider for muscle cells, but keep in mind that there are also gated K+ channels and Na+ and K+ leak channels. 4. The contractile units: sarcomeres. a. Myofibrils contain contractile proteins that are arranged into end-to-end units called sarcomeres. Each sarcomere produces a contraction. Sarcomeres are attached to each other. When a cell contracts, all sarcomeres along the myofibril contract in unison, and the entire cell shortens. b. Each sarcomere has a specific arrangement of protein filaments: i. The beginning and end of a sarcomere are deliniated by the Z-line: a mesh of intermediate filaments called connectins. Zlines CONNECT adjacent sarcomeres. ii. The center of each sarcomere contains a mesh of thick filaments (myosin) called the M-line. iii. Thin filaments (actin plus some other proteins) attach to the Z-line and run toward the central M-line, but don't reach the Mline. iv. Thick filaments (lots of myosins wrapped around each other) attach to the central M-line and run toward the Z-line, but don't reach the Z-line. 2 *The area where thin and thick filaments overlap, between the Zline and the M-line, is called the Zone of Overlap. This zone must be maintained in order for the sarcomere to be able to contract, because in a contraction, the thick and thin filaments interact. v. Titin filaments run from the M-line all the way to the Zline. They are connected to both. From the M-line, titin runs right down the center of the thick filaments. When the thick filaments end, titin continues on its own to the Z-line. Titin filaments move with the sarcomeres during contraction, and prevent the sarcomeres from stretching (lengthening) too much after contraction. They help to maintain the Zone of Overlap. vi. Banding patterns: because all of these proteins are located in specific areas of the sarcomere, and because some areas are denser with proteins than others, sarcomeres/myofibrils have patterns of light and dark areas. You need an extremely powerful microscope to detect these banding patterns; they are not the striations we see with our microscopes. a) Z-line: mesh of connectin, where titin and actin attach. The Z-lines of adjacent myofibrils attach to each other, and the Z-lines of peripheral myofibrils attach to the sarcolemma. This is what causes the visible striations we can see with our standard microscopes. b) I-band: area of thin fibers and titin only, no overlap of thin & thick. Includes the Z-line. c) A-band: start to finish of thick filaments, including the M line and the zone of overlap. d) Zone of overlap: where thick & thin fibers overlap e) H-band: area of thick filaments only, includes the M-line but not the zone of overlap. 3 II. Muscle Contraction A. The actual contraction (shortening) of a sarcomere: the relationship & design of thick and thin filaments 1. Muscle at rest Thick and thin filaments run parallel to one another. Thick filaments are composed of many strands of myosin. Each myosin contains a spring loaded bulbous "head" that sticks out from the thick filament. Thin filaments are composed of actin, tropomyosin, and troponin. Actin subunits have "active sites," areas that the myosin heads can bind to. At rest, tropomyosin covers those active sites, and myosin remains springloaded and unbound to actin. 2. When a contraction is initiated, Troponin moves tropomyosin out of the way. Myosin heads spring up and ratchet actin toward the M-line. The sarcomere contracts/shortens. All sarcomeres are affected and contract together. B. The whole process 1. Overview- Motor neurons release Ach onto a muscle cell. This causes Na+ chanels to open and Na+ rushes into the cell. Influx of Na+ causes SR to release Ca2+. Ca2+ binds to troponin, which causes troponin to move tropomyosin away from the active sites on actin. Myosin heads spring up, bind to the active sites, and ratchet actin. Meanwhile, Ach is destroyed by acetylcholinesterase, and Na+ is actively pumped back out of the cell. ATP is used to "recock" the myosin heads, or return them to their spring loaded positions. SR actively pulls Ca2+ back in, Ca2+ is removed from troponin, which causes tropomyosin to cover active sites again. -In more detail2. Neural stimulationKey words: neuromuscular junction, motor end plate, resting potential, action potential. Remember that "membrane potential" refers to the separation of charged particles on either side of a membrane. Potential is measured in volts, and cells maintain potentials in milliVolts (mV). Remember also that membrane potential is a form of stored energy, because those charged particles would MOVE across the membrane if they could. Ach causes Na+ channels at the motor end plate to open, and Na+ rushes in. The influx of positive charges (Na+) changes the voltage of the 4 membrane, or the membrane potential. This change in voltage causes more Na+ channels to open (voltage-regulated channels). This has a domino effect; as Na+ rushes into one area of the cell (starts at the motor end plate), adjacent areas open channels and so forth, until the entire membrane, INCLUDING THAT LINING T-TUBULES, is affected. *Side note: when you see the term "membrane permeability" for substances that can't cross by simple diffusion (that need protein channels), what that term refers to is how many channels are available to move the substance. For instance, we say a muscle cell changes its permeability to sodium in response to Ach. All that means is that more Na+ channels become available. 3. Calcium Release When the Na+ channels in the t-tubules of triads open (that is, when the action potential reaches a triad), voltage-regulated Ca2+ channels open in the terminal cisternae of the triad. Ca2+ rushes out and binds to troponin. 4. Contraction Ca2+ binds to troponin, which causes it to move tropomyosin from the active sites of actin. Myosin heads spring up and ratchet actin. ATP attaches to myosin head, detaching it from actin. ATP splits into ADP + Pi. The energy released causes the myosin head to recock into its spring-loaded ("high-energy") conformation. If another active site becomes available, it will go through the process again. The released ADP + Pi can be reconnected into ATP in one of three ways (section IV, "muscle energetics") 5. Acetylcholine breakdown In the meantime, Acetylcholinesterase has broken down Ach, almost immediately after its release. The Na+-K+ exchange pump has been busily pumping Na+ back out to restore ion concentrations. And, the SR actively pumps Ca2+ back in. Once all Ca2+ has been returned to the SR, the contraction ends. 6. Sarcomeres return to their resting lengths by gravity, opposing muscle action, and recoil of connective tissue. Titin prevents overstretching of sarcomeres, maintaining the Zone of overlap. 5 III. Muscle mechanicsA. Contraction cycles 1.Twitch- latent phase, contraction, relaxation -the next three "types" of contraction refer to WHEN subsequent neural stimuli are applied. Additional tension seen in subsequent contractions is caused by the fact that not all Ca2+ has been returned to the SR, and that enzyme activity and metabolism have started to step up.2. Wave summation & Incomplete tetanus 3. Treppe 4. Complete tetanus B. Contraction in whole muscles1. cells take turns contracting and relaxing, so that each cell can recover its ATP and fuel for making ATP between contraction cycles. 2. Motor units- each motor neuron controls several muscle cells scattered throughout a whole muscle (although each muscle cell is controlled by a single neuron). All muscle cells controlled by one motor neuron are referred to as a motor unit. When their common neuron is stimulated, all of them contract. When cells take turns resting and contracting, what's really happening is that some motor units are being stimulated while others are not. -Side note: strength of a whole muscle contraction (total tension) is determined by the total number of sarcomeres participating. That is determined by the number of myofibrils per muscle cell, the number of sarcomeres per myofibril, and the number of cells participating in the contraction. The more motor units called into action (“recruited”), the stronger the contraction. And the more myofibrils per cell, the stronger each cell can contract (you can change the amount of contractile fibers, but not the amount of cells, in a muscle).3. Muscle tone- in a whole muscle, some motor units are always active. Motor units of a muscle take turns. This causes muscles to always be "tone," or slightly tense, even when we're slouched on the couch basking in the warm glow of TV's warm glow. Muscle tone stabilizes joints and helps keep us warm (remember that heat is "lost" anytime energy is converted from stored to kinetic, which happens constantly with the transfer of ATP to ADP + Pi in active muscle). 6 C. Types of contractions- based on whole muscle length changes 1. Isotonic- muscle length changes a. Concentric- muscle shortens, tension overcomes resistance. b. Eccentric- muscle lengthens, tension is overcome by resistance, which pulls the muscle. Easiest to understand by thinking about opposing muscle action: When you lower a weight slowly, your biceps contracts to slow the movement of the forearm. Even though it's contracting, it's lengthening because the contraction of the triceps, gravity, and the weight of the...weight, are overcoming the tension produced by the biceps contraction. 2. Isometric- muscle does not change length, tension cannot overcome resistance but resistance doesn't come from a direction that pulls on muscle. Push your hands together in front of your chest; your muscles contract, but don't change length. IV. Muscle Energetics: what individual cells use for energy when A. Background- cells can use fatty acids & glucose for energy; that is, they can extract the energy from these substances and use that energy to add ADP + Pi, making ATP. Glucose can be used to make ATP via an anaerobic pathway (one that doesn't require oxygen): glycolysis. Glycolysis is relatively fast, but only yields two ATP for the cell to use. It does not require oxygen or available mitochondria. The biproducts of glycolysis, and fatty acids, can be used to make ATP via aerobic pathways (require oxygen). Aerobic respiration (making ATP) is relatively slow, but yields ~36 ATP per glucose. It also requires oxygen and mitochondria. B. Resting muscle cells- Use primarily aerobic pathways, and specifically mostly fatty acids, to generate ATP. Also prepare for the energy demands of contraction by: keeping enough ATP on hand for a couple seconds of contraction, storing glucose in the form of glycogen, and storing energy in the compound creatine phosphate (CP). CP stores energy, and the cell can use that energy to combine ADP and Pi extremely quickly, even more quickly than via glycolysis. A resting muscle fiber makes more ATP than it needs, and it uses the excess ATP to create all of the storage mentioned above (glycogen, CP). Cells must store energy in these forms because it simply can't make enough ATP, and store it directly, to power normal contractions. ATP doesn't store well (it breaks down relatively quickly). C. A muscle cell contracts 1. In the first few seconds of contractions, the cell uses its scant ATP reserves. 2. In the next few seconds (~15 sec), CP molecules split, and the energy released is used to reattach ADP & PO4, generating more ATP. 7 3. In the meantime, glucose molecules are being split (glycolysis) and aerobic respiration steps up. Glycolysis alone can generate enough ATP for about 2 minutes. 4. In the meantime, aerobic respiration has begun to extract energy from glycolysis’ leftovers and from fatty acids. Aerobic respiration starts to catch up with demands in a couple of minutes, and can supply energy for sustained periods of time. -Remember that cells take turns resting and contracting. Before ATP runs out, contracting cells relax, and relaxing cells take over. When energy demands are high, like when you're working out or running from a lion, more cells are called into action, and blood gets shunted to muscles which brings in more O2 and supports aerobic respiration. If you conduct a strong contraction "cold" (like suddenly lifting a heavy weight or scrambling up a tree to escape a lion that suddenly appears), you split tons of glucose suddenly. If you work up from lighter contractions to stronger contractions (like warming up or walking to find animal tracks before running to catch up to your prey), you split less glucose, and allow time for aerobic respiration to step up to meet energy demands.D. Types of muscle fibers (cells)- based on their primary energy source and speed of contraction. Whole muscles are composed of a mixture of these cell types. 1. Fast Glycolytic fibers Contract quickly, powerfully. Use mainly anaerobic pathways. Fatigue quickly. Few mitochondria & little myoglobin, lots of glycogen & myofibrils. Great for sudden, strong contractions; the type you might need to scramble up a tree to get away from a lion that suddenly appears, or to throw a boulder at that lion. Body builders love these types of fibers. Appear light, called white. 2. Slow Oxidative fibers Contract relatively slowly. Rely more on aerobic pathways. Lots of mitochondria & myoglobin, more capillaries. Less glycogen & myofibrils. Great for endurance contractions, like spending the day gathering berries & root vegetables. Marathon runners love these fibers. Appear red. 3. Fast Oxidative fibers (Intermediate fibers) Contract relatively quickly and powerfully, but don't fatigue as easily as fast fibers. Decent glycogen stores, but also plenty of mitochondria, mitochondria, and capillaries. You can change some of your fast fibers to intermediate fibers by participating in endurance exercise. In humans, many fibers are intermediate. Appear red. E. Please read “Effect of Exercise on Muscles,” pp 271-272. 8