Basic Anatomy & Physiology of the Lungs
advertisement
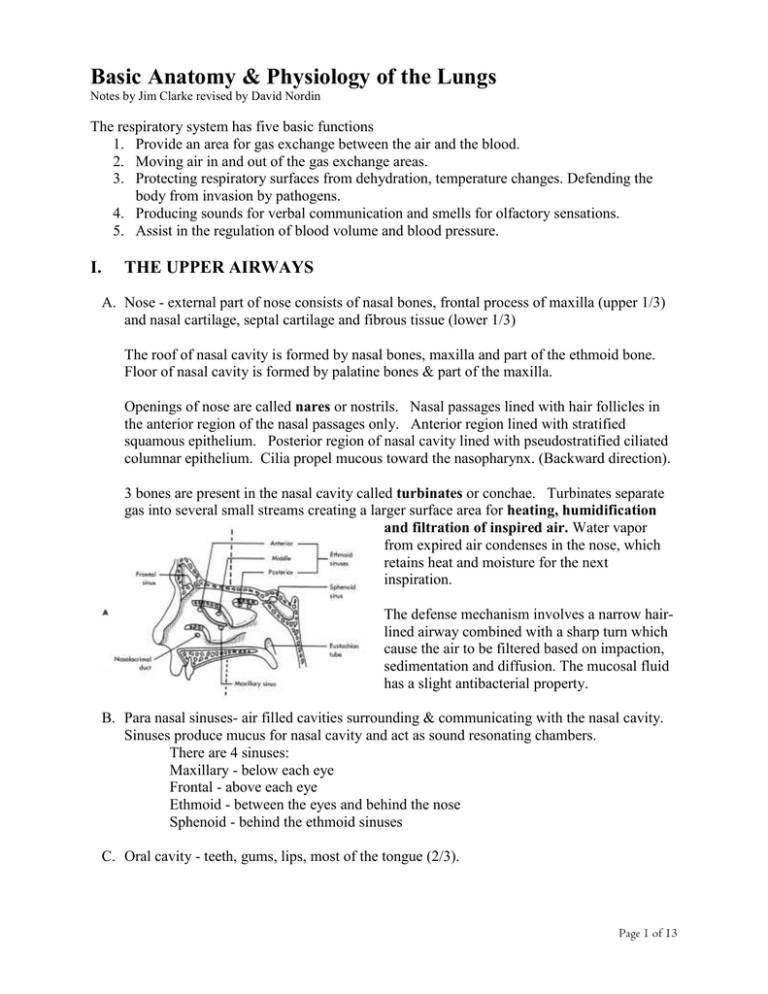
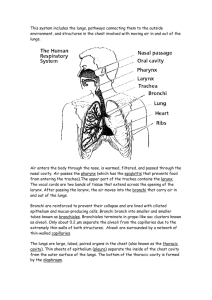
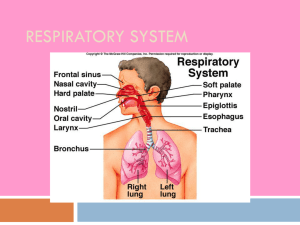
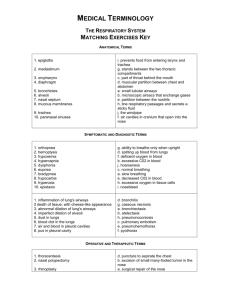
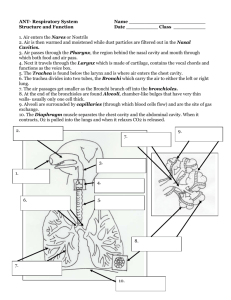
Basic Anatomy & Physiology of the Lungs Notes by Jim Clarke revised by David Nordin The respiratory system has five basic functions 1. Provide an area for gas exchange between the air and the blood. 2. Moving air in and out of the gas exchange areas. 3. Protecting respiratory surfaces from dehydration, temperature changes. Defending the body from invasion by pathogens. 4. Producing sounds for verbal communication and smells for olfactory sensations. 5. Assist in the regulation of blood volume and blood pressure. I. THE UPPER AIRWAYS A. Nose - external part of nose consists of nasal bones, frontal process of maxilla (upper 1/3) and nasal cartilage, septal cartilage and fibrous tissue (lower 1/3) The roof of nasal cavity is formed by nasal bones, maxilla and part of the ethmoid bone. Floor of nasal cavity is formed by palatine bones & part of the maxilla. Openings of nose are called nares or nostrils. Nasal passages lined with hair follicles in the anterior region of the nasal passages only. Anterior region lined with stratified squamous epithelium. Posterior region of nasal cavity lined with pseudostratified ciliated columnar epithelium. Cilia propel mucous toward the nasopharynx. (Backward direction). 3 bones are present in the nasal cavity called turbinates or conchae. Turbinates separate gas into several small streams creating a larger surface area for heating, humidification and filtration of inspired air. Water vapor from expired air condenses in the nose, which retains heat and moisture for the next inspiration. The defense mechanism involves a narrow hairlined airway combined with a sharp turn which cause the air to be filtered based on impaction, sedimentation and diffusion. The mucosal fluid has a slight antibacterial property. B. Para nasal sinuses- air filled cavities surrounding & communicating with the nasal cavity. Sinuses produce mucus for nasal cavity and act as sound resonating chambers. There are 4 sinuses: Maxillary - below each eye Frontal - above each eye Ethmoid - between the eyes and behind the nose Sphenoid - behind the ethmoid sinuses C. Oral cavity - teeth, gums, lips, most of the tongue (2/3). Page 1 of 13 Roof formed by hard and soft palate & uvula. Soft palate prevents food & liquid from entering nose during swallowing. Lined with stratified squamous epithelium. Palatine tonsils located adjacent to uvula on each side. Tonsils are collections of lymphoid tissue. D. The pharynx - located below the nasal cavity, behind the oral cavity and above the vocal cords. Strictly a passageway. Made up of 3 parts: 1. Nasopharynx - posterior to nasal cavity & superior to the soft palate. Lined with pseudostratified ciliated columnar epithelium. Adenoids (pharyngeal tonsils) located in posterior nasopharynx. Eustachian tubes (auditory tube) located here and connect middle ear to nasopharynx & serves to equalize pressure in the middle ear. 2. Oropharynx - lies between the soft palate superiorly and the base of the tongue inferiorly. Lingual tonsil located at the base of the tongue. Lined with stratified squamous epithelium, 3. Laryngopharynx- lies between the base of the tongue and the entrance to the esophagus. Lined with stratified squamous epithelium. Hyoid bone (horse-shoe shaped) lies at the base of the laryngopharynx. Provides support to the larynx (described below). II. THE LOWER AIRWAYS A. THE LARYNX - voice box located between base of tongue and the upper end of the trachea (wind pipe). Acts as a passageway for air; works as a protective mechanism against aspiration of food & liquids; generates sounds for speech. Cartilages of larynx: Thyroid - cover anterior larynx - upper thyroid cartilage connects to the hyoid bone with cartilaginous membrane material. Commonly called the ‘Adam’s Apple’ Epiglottis - spoon shaped fibro cartilage connected only at the base of the spoon so that it can move up and down to open for speech and breathing and close during swallowing preventing aspiration of foods. There is a unique fold at the base of the epiglottis used as a key landmark for intubation called the vallecula. Cricoid - signet ring shaped located at the base of the thyroid cartilage. Is attached to the first c-shaped rings of the trachea itself. It is the only completely circular ring of cartilage Page 2 of 13 of the larynx. It comes in handy with intubations. Slight downward pressure by a second person forces it posteriorly and the glottis to be better viewed by the intubator. Also this act prevents regurgitation of stomach contents by occluding the esophagus situated just behind the larynx. Arytenoids - small pyramid shaped cartilages that provide support to the vocal folds (cords) at the base of larynx. The arytenoid cartilage allows changes in the tension on the vocal cords, allowing phonation and sphincter control, with the interaction of the laryngeal muscles. Cuneiform & Corniculates- located slightly above the arytenoids; they also provide support to the vocal folds. The Cricothyroid ligament/membrane is the emergency procedure location for an upper airway complete occlusion. You can insert a large bore needle or cut with scalpel to provide an emergency airway for suctioning, supplemental oxygen and ventilate the patient. Vocal folds (cords) - Composed of central true cords and lateral false cords (ventricular folds). Vocal cords attach superiorly to the posterior surface of the thyroid surface and inferiorly to the arytenoid cartilage. The space between the cords is called the glottis. In the adult the glottis is the narrowest point in the larynx. In the infant, the cricoid cartilage is the narrowest part of the larynx. The part of the larynx just above the vocal cords is lined with stratified squamous epithelium. Below the vocal cords, the mucosa is lined with pseudostratified ciliated columnar epithelium. Laryngeal musculatureExtrinsic muscles pull down the larynx & hyoid bone to a lower position in the neck. Intrinsic muscles - control the movements of the vocal cords. Closure (adduction) of the vocal cords (sealing off the airway) occurs during lifting, pushing, coughing, throat-clearing, defecation, urination and child-birth. This is also called Valsalva's maneuver. B. THE TRACHEOBRONCHIAL TREE 1. Histology of airways - airways are generally composed of 3 layers: a. Epithelial layer - lining layer (innermost). Composed of ciliated pseudostratified columnar epithelium. Cilia begin to disappear as airways become very small in diameter (< 1 mm). The bronchial glands are the main producers of secretions in the respiratory tract. Interspersed between these are mucous secreting cells called goblet cells. The mucous produced by goblet cells covers the epithelial lining. Additional mucous is also produced by sub-mucosal glands (see Lamina propria). The mucous is composed of two layers - a watery outer layer called the sol layer and a sticky viscous inner layer called the gel layer. Normally cilia should beat within the thin sol layer allowing the mucous to move easily up towards the throat Each day we produce about 100 ml of mucous. Mucous normally moves at about 2 cm/minute. The process of mucous movement is called the mucociliary escalator. Page 3 of 13 Common things causing cilia to beat slowly or inconsistently thereby decreasing mucous movement are: Cigarette smoking dehydration Positive pressure ventilation endotracheal suctioning High oxygen concentration hypoxia Pollutants certain drugs (atropine) / Anesthetics At the bottom of the epithelial cells is a lining called the basement membrane. This acts as a border between the epithelial layer and the next layer called the: b. Lamina propria layer (sub-mucosal layer) contains: loose fibrous tissue, tiny blood vessels, lymphatic vessels, sub-mucosal glands and nerve fibers. Also present are bands of spiral smooth muscle fibers that wrap around the airway. These muscles are present in virtually all airways, however they are most important to the smaller airways at which point cartilage is no longer present (< 1 mm in diameter). When smooth muscle fibers are irritated that may contract and cause something called bronchospasm. Also located in the laminal layer are mast cells. These are messenger cells that when irritated (as occurs during allergic asthma attacks) may break open releasing many very potent chemicals (including histamine) that create swelling and bronchospasm itself. c. Cartilaginous layer - outermost layer. It progressively diminishes as airways extend out into the lungs and is generally totally absent in airways less than 1 mm in diameter. This layer provides support to airways. There are 2 major types of airways: Cartilaginous & Non-cartilaginous. Cartilaginous airways - usually larger than 1 mm in diameter these airways are generally called bronchi. Bronchi are surrounded by connective tissue sheaths. Cartilage present in airway walls provides support and/or protection (preventing collapse). All bronchi are supplied with blood by the bronchial arteries. Non-cartilaginous airways – do not have a ring for support but instead use traction of the surrounding elastic tissues and gas pressure gradient to keep the airways open. 2. Conducting Zone Trachea - 11 to 14 cm in length; 1.5 to 2.5 in diameter. Splits (bifurcates) into the main stem bronchi at the second anterior rib (at the level of the angle of Louis). The bifurcation is called the carina. Trachea is made up 16 to 20 C-shaped rings. The trachea shares a common posterior wall at the incomplete part of the c-shaped rings with the esophagus. Page 4 of 13 Main-stem bronchi - right main-stem goes to the right lung; left main-stem to left lung. Cshaped rings make up the outermost layer of each main stem bronchi. The angle from midline of the right mainstem is about 25 degrees while the angle from midline for the left mainstem is between 40 - 60 degrees. As a result aspirated materials tend to enter the right mainstem bronchi. Main-stem bronchi are referred to as the tracheobronchial tree's first generation. Lobar bronchi- right lung has three sections called lobes (upper, middle and lower). Each section or lobe is supplied by lobar bronchi. Lobar bronchi have cartilaginous plates in their walls rather than c-shaped rings. This is the second generation. Segmental bronchi- each lobe is divided into a variety of smaller areas called segments. Each segment is supplied by a respective airway. There are 10 segments in the right lung and 8 segments in the left lung. This is the third generation. Sub-segmental bronchitracheobronchial tree separates into progressively smaller airways from Generation four through nine. These bronchi range in size from 1-4 mm in diameter. Entering the noncartilaginous airways zone Non-cartilaginous airways - usually smaller than 1 mm in diameter. Connective tissue sheaths and cartilage are no longer present. Noncartilaginous airways are present between generations 10 through 23. Types of non-cartilaginous airways Bronchioles- Generations 10-15. These airways are not very rigid since no cartilage is Page 5 of 13 present and are prone to narrowing in disease. Bronchioles are generally surrounded and pass through the parts of the lungs that are made up of air sacs (alveoli). The air sacs tend to hold the airways open (tethering effect). Bronchioles receive their blood supply from the bronchial arteries. Terminal bronchioles - Generations 16-20. These are the last purely conducting airways. No gas exchange occurs in these structures. The average diameter is about 0.5 mm. Cilia begin to disappear and epithelium changes to a cuboidal flat shape. Some terminal bronchioles may have small openings or channels in their walls called Canals of Lambert that connect with adjacent air sacs. Clara cells are present in terminal bronchiole walls. These cells may act to detoxify inhaled gases. They receive their blood supply from pulmonary capillaries. Each terminal bronchiole is supplied by its own respective pulmonary capillary. 3. Gas Exchange Zone Respiratory bronchioles- Generations 21-23. These airways have actual alveolar sacs imbedded in their walls where gas exchange is taking place. No cilia are present. Each respiratory bronchiole branches into three: Alveolar ducts- each respiratory bronchiole bifurcates into 3 alveolar ducts. Each terminal bronchiole with its complement of 3 respiratory bronchioles; 9 alveolar ducts and 1 pulmonary capillary is called the "primary lobule" or acinus. Each primary lobule has about 2000 alveoli. The area where gas exchange occurs is called the "lung parenchyma". There are approximately 300 million alveoli in the normal adult lungs creating a surface area of approximately 70 square meters. Pulmonary capillaries cover about 80% of the surface of each alveolus. There are several forms of intercommunication channels so the alveoli are not ‘deadended’. 1. Intersegmental bronchioles – provide a collateral gas movement and even distribution of gases. 2. Pores of Kohn- these are small openings between alveoli allowing air, certain cells and fluid to move between adjacent air sacs. The numbers of pores tend to increase with age indicating that these may be the result of the aging process. 3. Canals of Lambert - connections of adjacent bronchioles allowing for "collateral airflow". Alveoli - made up of 3 types of cells Page 6 of 13 Type 1- these are flat, very thin, fried-egg like cells that make up the largest part (95%) of the alveolar walls. They have no known metabolic function. Type 2- these are infrequent cells (5%) that are cuboidal in shape. They are highly metabolic and are responsible for producing pulmonary surfactant. Surfactant is critical in maintaining the open structure of alveoli by decreasing surface tension forces and preventing collapse of air-sacs. Premature newborns tend to have an abnormally low number of type 2 cells and as a result their alveoli tend to collapse during breathing. Type 3- (alveolar macrophage) this is actually a scavenger cell created in bone marrow that migrates to the lungs. These cells engulf material that manages to land on the alveolar surface. 4. Interstitium This is the term given to the spaces between alveoli. This area tends to be gel-like and is composed of a web-like network of collagen fibers. The interstitium is broken down into 2 compartments. 1. Tight space - the micro-thin areas in between alveolar walls and their respective pulmonary capillaries. 2. Loose space - the areas occupied by lymphatic, nerve fibers, vessels and that is not involved in gas exchange. This area can hold a significant amount of non-vascular lung fluid. III. FLUID CIRCULATION IN THE LUNGS Lymphatic - Drain excess fluid and white cells from the interstitial spaces (both deep and superficial vessels). They help to keep the lung "dry". Also it plays a role (with the phagocytes) in removing bacteria, foreign material and cell debris via the lymph fluid. This is why your lymph glands are swollen with some types of infectious diseases. It drains into the thoracic duct. If the vessels are overloaded and swollen with excessive fluid they can be seen on X-ray as Kerley A or B lines. They normally can’t be seen on X-ray. Bronchial circulation - the bronchial arteries provide nutrition to airways and tissues Page 7 of 13 down to the level of the terminal bronchioles. Bronchial veins drain this same area. Pulmonary circulation - Arterioles and capillaries bringing blood to alveoli in order to take part in gas exchange. Pulmonary arteries carry de-oxygenated blood (low in oxygen & high in carbon dioxide) from the right ventricle of the heart to the lungs. Pulmonary veins carry oxygenated blood (high in oxygen & low in carbon dioxide) back from the lungs to the left atrium of the heart. This is ‘opposite’ of normal systemic arteries and veins. Pressures in the normal pulmonary circulatory system average about one sixth of that in the systemic circulation. Even thought the amount of blood is the same, the pulmonary system offers much less resistance. High pulmonary resistance is related to right heart failure and cor pulmonale. The normal Partial Pressure of Oxygen (PaO2) is 80 - 100 mmHg (torr). The normal PaCO2 is 35 - 45 mmHg (torr). The normal PvO2 is 40 mmHg (torr). The normal PvCO2 is 45 mmHg (torr). The above values are for adults. Virtually all of the output from the right heart (cardiac output is denoted with the symbol (Q) passes through the lungs- normal Q at rest is approximately 5-6 l/m. IV. THORACIC CAVITY & WALL The thorax consists of three compartments: 1. Mediastinum 2. Right pleural cavity 3. Left pleural cavity The thoracic cavity is formed by the ribs & sternum anteriorly and the ribs and spine posteriorly. It is narrower at the top and wider at the bases. The superior margin is at the thoracic inlet at the base of the neck. The inferior margin is formed by the diaphragm. The thoracic cage serves two purposes. First, its bony structure protects the vital organs inside. Secondly, breathing is facilitated with expansion and contraction of chest volume for breathing (moving air in and out of lungs). Thoracic cage is made up of: a. The ribs: There are 12 ribs; 7 are true ribs (articulating directly with the sternum); 3 are false ribs (connecting with adjacent ribs and then with the sternum); 2 are floating ribs (they do not connect with the sternum). The true and false ribs are connected to the sternal body via the costo-chondral cartilage. Page 8 of 13 The ribs have a costal groove on the underside of each rib. This is where the arteries, veins and nerves run. When puncturing through the ribs with a needle during a thoracentesis the doctor must be on the top of the rib to avoid vessel and nerve damage. The ribs move simultaneously about two axis – often referred to as ‘pump handle’ and ‘bucket handle’ motion. b. The sternum: Is a dagger-like structure that provides protection. Averages 18 cm in length. Has 3 parts: the upper manubrium, the body, and the lower xyphoid process. Important landmarks are the suprasternal notch and the Angle of Louis. c. And the vertebral bodies of the thoracic spine. V. LUNGS AND PLEURA The lungs a paired, cone shaped organs. They are 90% gas and 10% tissue. The left lung is somewhat narrower because of the heart. The right lung is slightly elevated and thus shorter, due to the liver. The right lung has upper, middle and lower lobes. The left lung only has an upper and lower lobe. They extend from the diaphragm to 1 to 2 cm above the clavicles. They are divided into lobes which are separated by one or more fissures. The right ling has the extra fissure (because it has the extra lobe). The lingual of the left lobe corresponds to the missing middle lobe of the right lung. Each lobe is subdivided into segments. The right lung has 10 segments and the left only 8 segments. Lung landmarks of note are the apex, the bases, and the costophrenic angle. The lungs are covered with a very thin lining layer of mesothelial tissue called the visceral pleura. The interior surface of the thoracic cavity is also lined with a very thin mesothelial layer of tissue called the parietal pleura. The two pleural surfaces adhere to one another based upon a slight suction. These cells produce a lubricating fluid that allows the lungs to smoothly glide over the surface of the thoracic cavity. The space between the pleural layers is referred to as the intra-pleural space. Normally this is a "potential" space and as such it should have no air present. Fluid entering the pleural space is normally drained via lymphatic vessels. The lungs, in addition to gas exchange, perform other functions. 1. They are a blood reservoir for the left ventricle of the heart 2. The lungs filter the blood and traps particles before they inflict damage to other parts of the body (e.g. A clot traveling to the brain causing a stroke) 3. The lungs play an active role in metabolism. They are responsible for synthesis, activation, inactivation and detoxification of many bioactive substances. a. Heparin, histamine and serotonin are stored or synthesized in the lung b. Angiotensin is converted to its active form in the lung c. Adenosine triphosphate (ATP) and norepinephrine ar partly removed from the blood and inactivated by the lungs. VI. MEDIASTINUM & HILUM Mediastinum is the area between the lungs; below the thoracic inlet to the thorax and above the diaphragm. It contains the heart; thymus gland; major vessels (pulmonary artery and Page 9 of 13 pulmonary veins; ascending & descending aorta; inferior & superior vena cava); nerves; trachea; esophagus and lymph nodes. Hilum - the spot at which the main-stem bronchi enter each lung. VII. BREATHING MUSCLES Inspiratory- primary muscles: Diaphragm and abdominals. Diaphragm is innervated via the phrenic nerve. Phrenic nerve exits the spine at points between C2 & C5. Phrenic nerve bifurcates into two limbs once it enters the thoracic cavity, transits across the thoracic cavity with each limb going to one-half of the diaphragm. Each one-half is referred to as a "hemi-diaphragm". The diaphragm is a very energy efficient muscle and rarely tires (except in chronic lung disease). The diaphragm only moves 1 to 2 cm during normal breathing but accounts of 75% of the change in thoracic volume. The diaphragm may become flattened (and less efficient) with air trapping with obstructive diseases (COPD). Abdominal breathing is taught to patients as an efficient breathing method. The internal intercostals are used during exercise so is not considered primary. Accessory muscles of inspiration: 1. Neck muscles - scalenes, sternocleidomastoids, trapezius. 2. Chest muscles - pectoralis major. These muscles are used by patients suffering from lung disease during periods of exacerbation (a sudden worsening). They are very energy inefficient. These muscles consume more oxygen and produce more CO2 than the primary muscles of inspiration. Expiratory muscles - normally exhalation is passive. Only during exercise or stress does it become an active process. Abdominal muscles used are the rectus abdominus; internal & external obliques and the transverse abdominus. These muscles squeeze the abdominal contents and push up against the bottom of the diaphragm. The external intercostals also assist by decreasing thoracic size during exhalation. Page 10 of 13 VIII. LUNG VOLUMES & CAPACITIESTIDAL VOLUME (Vt) - the amount of air exhaled during normal relaxed breathing. (In adults is about 350 to 600 ml). VITAL CAPACITY (VC) - the maximum amount of air that can be exhaled after first taking a maximal inhalation. (Normally between 3000 to 6000 ml's in adults). RESIDUAL VOLUME (RV) the amount of air remaining in the lungs after a maximal exhalation. This volume will never "comeout". Therefore it cannot be directly measured. Other "indirect" techniques must be used to determine its size. TOTAL LUNG CAPACITY (TLC) - the amount of air present in the lungs at the point at which a person has taken a maximal inhalation and is holding that volume in their lungs. This is the sum of the RV + VC. Also must be indirectly measured. EXPIRATORY RESERVE VOLUME (ERV) - the additional amount of air that can be forcibly exhaled after first completing a relaxed exhalation. INSPIRATORY RESERVE VOLUME (IRV) - the additional amount of air that can be inhaled after completing a normal inhalation. FUNCTIONAL RESIDUAL CAPACITY (FRC) - the amount of air present in the lungs after a normal relaxed exhalation. This is the sum of the RV + ERV. INSPIRATORY CAPACITY (IC) - the amount of air that can be maximal inhaled after completing a relaxed exhalation. This is the sum of the Vt + IRV. IX. GAS PICKUP AND DELIVERY The problem of delivering oxygen (and nutrients) to the cells and removing carbon dioxide (and waste products) is solved by a handy transport system where oxygen is bound to hemoglobin and carbon dioxide is chemically bound or transported in the plasma of the blood. Thus the body had developed and excellent gas exchange transport system. Page 11 of 13 X. CONTROL OF BREATHING Central control - via the brain stem & medulla. This area receives impulses from "sensors" located in the brain and peripherally; interprets the received impulses and sends out messages to the respiratory muscles initiating breathing and controlling the depth and rhythmicity of breathing. Central Chemoreceptors - located in the brain stem, they are sensitive to cerebral spinal pH. Since pH is most related to arterial carbon dioxide levels, the central chemoreceptors are indirectly sensing PaCO2. As PaCO2 rises, breathing rate & depth should increase and visa versa. The central chemoreceptors normally account for how we breathe. Peripheral Chemoreceptors - located at the bifurcation of the internal & external carotid arteries in the neck. These specialized cells measure the PaO2 of blood and the arterial pH in the circulating blood. Normally they are not active unless the PaO2 drops below 60-70 mmHg (torr). The lower the PaO2 drops below 60 mmHg, the more active they become. When active, the peripheral chemoreceptors send impulses to the medulla causing the rate & depth of respiration to increase. If the arterial pH drops below 7.35, the same event occurs. XI. VENTILATION TERMS MINUTE VENTILATION (VE) - THE VOLUME OF AIR EXHALED BY A PATIENT IN ONE MINUTE. MAY BE CALCULATED BY MULTIPLYING THE RESPIRATORY RATE TIMES THE TIDAL VOLUME. (A dot "." appearing above any symbol means "per unit time" usually per minute. . Vt x R.R. = VE DEADSPACE - (Vds) the volume of each breath taken that does not take place in gas exchange. (Usually is referred to as the anatomic deadspace.) This amount corresponds to the volume of air present in conducting airways like the nose, pharynx, larynx, trachea, mainstem bronchi, segmental bronchi, sub-segmental bronchi & terminal bronchioles. ALVEOLAR VENTILATION - ( VA) - the volume of air that actually takes part in gas exchange each minute. . (VT - Vds) x R.R. = VA Under normal conditions at rest this volume is 4-5 liters/minute in adults. The V/Q ratio - expresses the relationship between the amount of ventilation going to the lungs in the form of the air that we breathe compared to the amount of blood flow passing through the lungs at the same time. Since normal VA (alveolar minute ventilation) is 4 l/m and normal Cardiac Output (Q) is 5 l/m, the normal V/Q ratio is expressed as 0.8. (There are no units to this number.) Page 12 of 13 In disease states of the heart &/or lungs, the V/Q value may be greater than .8 or less than .8. If it is > .8 it is called HIGH V/Q. If it is < .8 it is called LOW V/Q. Patients who are experiencing problems with low oxygen levels frequently are suffering from LOW V/Q. Page 13 of 13