Lab 43. Reproductive Physiology
advertisement

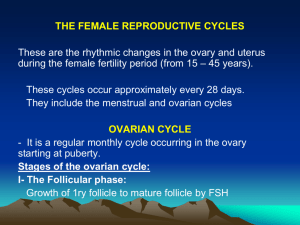
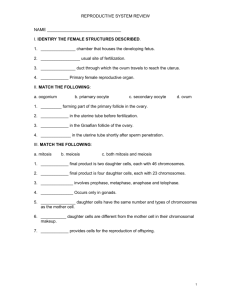
Lab 43. Reproductive Physiology • Be able to identify the following tissues microscopically: testes (seminiferous tubules), ovary (stages), sperm, mammary gland (active vs not), prostate gland. Be able to identify a follicle within an ovary. • Be able to identify the following structures on a model: testes, epididymis, ejaculatory duct, prostate gland, bladder, urethra; ovary, Fallopian tube, uterus, cervix, vagina, bladder, urethra Structure of the Testes Figure 28–4 Tunica Vaginalis • Serous membrane that lines scrotal cavity • Reduces friction between opposing surfaces: – parietal (scrotal) – visceral (testicular) Tunica Albuginea • Dense layer of connective tissue rich in collagen fibers • Deep to tunica vaginalis • Continuous with fibers surrounding epididymis • Fibers extend into substance of testis • Form fibrous partitions, or septa that converge near entrance to epididymis • Supports: – blood and lymphatic vessels of testis – efferent ductules Structures of Testes • Septa subdivide testis into lobules • Lobules contain about 800 slender and tightlycoiled seminiferous tubules: – Produce sperm – About 80 cm long each – Testis contains about 1/2 mile of tightly-coiled seminiferous tubules • Each Seminiferous Tubule Forms a loop connected to rete testis: a network of passageways • 15–20 large efferent ductules connect rete testis to epididymis The Seminiferous Tubules Figure 28–5b Connective Tissue Capsules • Surround tubules • Areolar tissue fills spaces between tubules • Spaces contain: – blood vessels – large interstitial cells (cells of Leydig) • Produce androgens (male sex hormones) including testosterone (most important androgen) Contents of Seminiferous Tubules • Spermatogonia (stem cells, near outer surface) • Spermatocytes at various stages of meiosis (primary, secondary) • Spermatids (immature) • Spermatozoa (mature) • Large sustentacular cells (Sertoli cells) – Are attached to tubular capsule – Extend to lumen between other types of cells – Secrete inhibin, ABP, MIF The Seminiferous Tubules Figure 28–5c Meiosis • In seminiferous tubules: begins with primary spermatocytes and produces spermatids (undifferentiated male gametes) • Basically, in meiosis one, you separate the homologues (meaning each of the resulting daughter cells gets only one of your two copies of chromosome #4 and one of your two copies of chromosome #21, etc. (Both cells contain 23 chromosomes with 2 chromatids each (reductional division) • Meiosis two is just like mitosis, only it is different than mitosis in somatic cells because there are only 23 chromosomes at this point yields 4 cells, each containing 23 chromosomes (equational division) Spermatogenesis Figure 28–7 Seminiferous Tubule • Using low power, take a look around (you don’t have to sketch what you see at low mag). • Locate, by sight: tunica vaginalis, tunica albuginea, septa, lobules, and the numerous seminiferous tubules. • On medium or high power, sketch seminiferous tubules. In your sketch, draw and clearly label one or two tubules with: the lumen, interstitial space, interstitial cell (aka Leydig cell), spermatogonia (the stem cells), primary or secondary spermatocytes (cells midway through meiosis), spermatids (immature sperm, products of meiosis), sustentacular cells (aka, Sertoli cells). A. What hormones do sustentacular cells secrete? B. What do interstitial cells secrete? The Female Reproductive System Figure 28–13 Organs of the Female Reproductive System • • • • • Ovaries Uterine tubes Uterus Vagina External genitalia Oogenesis Figure 28–15 Oogenesis • Begins before birth, pauses • Continues at puberty • Does not actually complete until fertilization! • Ceases at menopause • Ovarian Cycle Includes monthly oogenesis between puberty and menopause Oogenesis Oogenesis • Oogonia = females reproductive stem cells – complete mitotic divisions before birth (not thought to happen at all after birth, but…) • Between third and seventh months: – primary oocytes begin meiosis but stop at prophase of meiosis I • At birth, a baby girl’s ovaries have about 2 million primordial follicles each containing a primary oocyte arrested in prophase I of meisosis • At puberty rising FSH triggers start of ovarian cycle Oogenesis • Each month thereafter some primary oocytes are stimulated to develop further by FSH • One per month will complete meiosis I and become a secondary oocyte just prior to ovulation • Ovary releases secondary oocyte (not mature ovum) that is suspended in metaphase of meiosis II • Meiosis II is only completed upon fertilization The Ovarian Cycle Figure 28–16 (1 of 2) The Ovarian Cycle Figure 28–16 (2 of 2) Before Ovarian Cycle • Ovarian Follicles specialized structures in cortex of ovaries where oocyte growth and meiosis I occur • Primary Oocytes Are located in outer part of ovarian cortex: – near tunica albuginea – in clusters called egg nests • Primordial Follicle: each primary oocyte in an egg nest is surrounded by follicle cells The Ovarian Cycle • Formation of primary follicles – follicle cells become granulosa cells – Thecal Cells surround follicle, work with granulosa cells to produce estrogens • Formation of secondary follicles – Follicular fluid accumulates between inner and outer layers of follicle • Formation of tertiary follicle – Antrum (cavity surrounded by granulosa cells) enlarges and fills with follicular fluid – Just before ovulation, oocyte becomes secondary oocyte and floats free in the anrtum The Ovarian Cycle – Luteal Phase • After ovulation, formation of corpus luteum: – produces steroid hormone progesterone which prepares uterine lining for pregnancy • If fertilization does not occur corpus luteum degenerates about 12 days after ovulation fills with scar tissue to become corpus albicans Ovaries Slide- “Ovary immature” • On low power, take a look around. On medium power, take a closer look at the numerous primordial follicles. Slide- “Ovary-Graafian follicle” • Draw and clearly label the ovary. Indicate the different follicles. Find and sketch a secondary or tertiary follicle (Graafian follicle). Label: the primary oocyte, antrum, granulosa cells, theca cells. (Note: when viewing follicles, realize that the oocyte may not be in the plane of view). Slide- “Ovary - Corpus luteum” • Draw and clearly label an ovary containing a corpus luteum (and/or corpus albicans). Indicate the corpus luteum in your sketch. A. What important hormone is secreted by the corpus luteum? B. What important function does this hormone have in terms of the menstrual cycle? The Uterus Figure 28–18a Uterine Wall • Has a thick, outer, muscular myometrium • Has a thin, inner, glandular endometrium (mucosa) • Uterine Glands open onto endometrial surface, extend deep into lamina propria 2 Divisions of Endometrium • Functional zone: layer closest to uterine cavity – Contains most of uterine glands – Contributes most of endometrial thickness – Undergoes dramatic changes in thickness and structure during menstrual cycle • Basilar zone: adjacent to myometrium – Attaches endometrium to myometrium – Contains terminal branches of tubular endometrial glands The Uterine Wall Figure 28–19 Uterus • If slide is available, draw and clearly label the uterus. Label: myometrium, endometrium and uterine cavity. Within the endometrium, indicate the basilar zone and functional zone. Label endometrial glands. Endometrium in Uterine Cycle Figure 28–20 The Mammary Glands Figure 28–23a Mammary Glands Figure 28–23b, c Mammary Gland Ducts • Leave lobules, Converge to form single lactiferous duct in each lobe • Forms expanded chamber (lactiferous sinus) • 15–20 lactiferous sinuses open to each nipple (Why?) Active Mammary Gland • Consists of multiple glandular tubes ending in secretory alveoli • Does not complete development unless pregnancy occurs • Near complete at about 6 months gestation, but milk is usually not let down in any great amounts until delivery (Why?) Mammary glands • Look at both inactive and active mammary gland tissue. Draw and clearly label active tissue: secretory alveoli, and lactiferous ducts. A. What is in the ducts? B. How do the two tissues look different? Slides • Seminiferous Tubules • Ovaries: – Ovary immature – Ovary- Graafian follicle – Ovary - Corpus luteum • Uterus • Mammary glands – Active – Inactive