PD-1, SOCS-1, Tim-3 in HCV infection -WHY WE CARE?
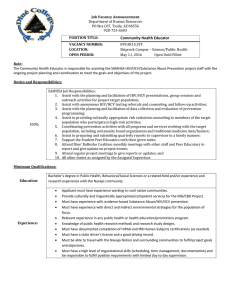
advertisement

PD-1, SOCS-1, Tim-3 in HCV infection -WHY WE CARE? Yao, Z. Q. M.D. Ph.D. Director, Hepatitis (HCV/HIV) Program, JHQ-VAMC Associate Professor, Division of Infectious Diseases Department of Internal Medicine, Quillen COM ETSU Disclosures • Grant funding from NIH NIAID, NIDDK, and ETSU/WFU • No other financial interests involved in this presentation In this Presentation We’ll talk: 1. Clinical features and immunodysregulations of HCV infection 2. Negative signaling molecules such as PD-1, SOCS-1, and Tim-3 in control of human innate to adaptive immune responses We expect to know: A) how HCV employ negative signaling molecules to establish chronic infection; B) why we care about this – its application in the HCV pathogenesis, treatment, and vaccine development Clinical features of HCV infection 15% 200 M WW PD-1, SOCS-1, Tim-3 4 M U.S. HIV Why the majority of infected individuals become chronic? Immunodysregulation in chronic HCV infection Impaired Monocyte maturation into DC Decreased IL-12 Viral Persistence T cell dysfunction and exhaustion mixed cryoglobulinemia B cell clonal expansion non-Hodgkins lymphoma B cell hyperactivation Th17 cell and Foxp3+ Treg cell expansions What is the underlying mechanism leading to these immunodysregulations? Mechanism leading to these immunodysregulations The primary site of HCV infection is within the liver, where hepatic sinusoids lack basal membrane with a very low velocity of blood flow PD-1 PD-1 Tim-3 Tim-3+ CD14+ M/MØ SOCS-1 100% 50% 0% 6h 12 h HCV+ Huh-7 So HCV-infected hepatocytes has ample opportunity to contact circulating or infiltrating immune cells 24 h 48 h HCV- Huh-7 What is PD-1 • • • • • Programmed Death-1, first identified on apoptotic cells Inducible expressed receptor on immune cells upon activation Provides a negative signaling to TCR positive signaling pathway A powerful negative feedback mechanism to balance the +/- signal Blocking PD-1 signaling will reverse T cell dysfunction PD-1 and T cell function / exhaustion Tim-3 : a molecule different from PD-1 A new negative molecule first identified on Th1, but not Th2, and now also found on other cell types: M/MФ, NK cells Suppressor of cytokine signaling (SOCS) – a family of negative inhibitors of cell signaling Cytokine Why we care about this? -Negative signaling molecules in HCV pathogenesis PD-1 & Tim-3 in Monocyte IL-12 regulation Immunodysregulation in chronic HCV infection Impaired Monocyte maturation into DC Decreased IL-12 Viral Persistence Monocyte IL-12 expression is significantly suppressed in chronic HCV infection Healthy HCV Gating strategy CD14 15.2% IL-12 50% 40% 30% 20% 10% 0% 60% PD-1+ CD14+ cells IL-12+ CD14+ cells 60% ** ____________________________ * _______________ ■ □ □ ▲ ■ □ □ □ ▲ □ ■ ▲ □ ▲ ■ ■ ■ □ □ ■ ▲ ▲ ■ □ ▲ ■■ ▲ ▲ ■ ■ □ ▲ ■ ▲ ▲ □ ▲ ▲ ■ ▲ ▲ ▲ ▲ □ ▲ □ ▲ ▲ ▲ □ ▲ ▲ ▲ HCV-Infected HCV-Resolved Healthy 50% 40% 30% 20% 10% 0% ** __________________________ * ____________ ▲ ▲ ▲ ▲ ▲▲ ▲ ▲▲ ▲▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ □ □□ □ □ □ □ □□ □ □ □□ □ HCV-Infected HCV-Resolved ■ ■ ■ ■■ ■ ■ ■ ■ ■ ■■ Healthy Ma et al. Immunology 2010; Zhang et al. J Immunol 2011 PD-1 is inversely associated with IL-12 production by monocytes B) A) Pearson Correlation = -0.464* PD-1 PD-1+ CD14+ cells LPS/R848 IL-12 50% 45% 40% 35% 30% 25% 20% 15% 10% 5% 0% 0% C) 40% IL-12 production D) 50% P = 0.003 CD14+ Cells P = 0.034 40% 30% 20% IL-12+ PD-1+ CD14+ Cells 50% 20% 10% 0 40% 30% 20% 10% 0 before IFN/RBV after IFN/RBV before IFN/RBV after IFN/RBV 60% Tim-3 is a negative molecule expressed on resting monocytes to control IL-12 expression un-stimulated 1.2% 45.8% iso TLR-stimulated 3.0% Tim-3 Tim-3 iso un-stimulated 2.7% 0.2% 55.3% 0.1% 0.4% 0.1% TLR-stimulated 1.8% 2.2% 38.9% IL-12 CD14 0.2% 0.3% 27.2% Positive cells (%) CD14 70 60 50 40 Tim-3 30 IL-12 20 10 IL-12 0 0h 6h 18h 24h 48h 72h Time of TLR stimulation Zhang et al. JLB 2011 Tim-3 functions as a break, and TLR as the driving force for IL-12 expression Tim-3/IL-12 expression in resting and activated monocytes in HCV patients A Healthy Subject Naïve Activated Isotype control HCV Patient Naïve Activated 38.3 2.8 4.1 4.4 54.6 3.4 8.7 27.0 27.3 45.5 47.6 22.3 18.8 13.5 74.4 Tim-3 7.4 CD14 0.2 40.9 33.9 67.7 0.4 54.0 15.3 28.5 0.1 22.7 2.5 31.8 0.2 29.6 1.0 CD14 71.3 IL-12 ** B *** C NS ** *** *** *** % of IL12+ CD14+ M/MØ % of Tim-3+ CD14+ M/MØ *** Naïve Activated Naïve Activated Healthy Subjects Naïve Activated Chronic HCV Patients Naïve Activated Zhang et al. PLoS One 2011 It’s not because of TLR expression, but due to defect of intracellular signaling A) Healthy Subjects 30 * 10 0 Healthy Subjects HCV patients 99.5% 99.7% 40 20 Healthy Subjects 40.7% TLR7+ CD14+ Cells 10.3% TLR4+ CD14+ Cells B) HCV patients 100 50 0 Healthy Subjects HCV patients HCV patients Healthy subject HCV-infected 21.6% D) IgG + HCV-resolved 23.7% 9.6% anti-Tim-3 + Core Phospho Stat1 Total Stat1 STAT-1+ CD14+ Cells C) 30 20 * 10 0 Healthy HCV-infected HCV-resolved HCV core TLR PD-1 Isotype gC1qR Count LPS R848 Control IgG + 11.7% 3.2% LPS R848+core+a-PDL-1 8.9% SOCS-1 IL-12 a-PDL-1 + Core SOCS-1 β-actin % IL-12+CD14+ cells M/MФ IL-12 production LPS R848+core+IgG 1.2% 14 12 ** 10 8 ** 6 4 2 0 LPS/R848 L/R core contl IgG L/R core anti-PDL-1 Silencing SOCS-1 inhibits PD-1 expression and improve IL-12 production A) 48 h after transfection Control siRNA SOCS-1 siRNA + + 72 h after transfection Control siRNA + SOCS-1 siRNA + Core SOCS-1 β-Actin B) Count Isotype 0.73% LPS R848 Core control siRNA 39.1% LPS R848 Core SOCS-1 siRNA 2.9% PD-1 C) Count Isotype 2.88% LPS R848 Core control siRNA 10.1% LPS R848 Core SOCS-1 siRNA 19.4% IL-12 Crosstalk between PD-1 and SOCS-1 to inhibit STAT-1/5 phosphorylations Control siRNA + + Control IgG - + + a-PDL-1 + pSTAT-1 Total STAT-1 Total STAT-1 Control IgG Anti-PDL-1 Anti-PDL-1 %STAT-1+CD14+ cells CD14 25 * 20 15 10 5 0 L/R core contl IgG Core pSTAT-1 STAT-5 Control IgG Core STAT-1 D) B) SOCS-1 siRNA L/R core anti-PDL-1 CD14 %STAT-5+CD14+ cells A) ** 80 70 60 50 40 30 20 10 0 L/R core contl IgG L/R core anti-PDL-1 Our Model LPS/R848 TLRs Signaling pathways for IL-12 expression (Jak/STAT) Gal-9 Tim-3 PD-L1 HCV core PD-1 gC1qR SOCS-1 Th1/Tc1 dysregulation Viral persistence Viral clearance Immunodysregulation in chronic HCV infection Impaired Monocyte maturation into DC Decreased IL-12 Viral Persistence T cell dysfunction / exhaustion B cell clonal expansion mixed cryoglobulinemia non-Hodgkins lymphoma B cell hyperactivation What is the underlying mechanism leading to these immunodysregulations? Why we care about this? -Negative signaling molecules in HCV pathogenesis HCV infection lead to a differential effect on T/B lymphocytes what is the underlying mechanism ? 45.3% HCV-NHL 10.4% 19.1% 96.2% IgM 5.8% IgG HCV-Tetramer CD69 19.4% TALL-1 Cell Immunology & Biology 2011 83.3% HCV-NHL 4.2% 72.3% 48.8% HS CD4 CD8 CD4 CD20 70.0% 53.5% Tetramer CD8 HCV CD20 6.9% PD-1 HCV-NHL PD-1 PD-1 47.3% 37.2% HS HCV-NHL 13.7% HS CD20 CD20 Differential regulation of T/B lymphocyte activation in patients with HCV-NHL T cells ____________ B cells ____________ HCV-NHL HS HCV-NHL HS T cells ____________ B cells ____________ HCV-NHL HS HCV-NHL HS SOCS-1 SOCS-1 hβ2M pSTAT1 Differential regulation of T / B lymphocyte signaling by HCV core protein T cells + - B cells + - Core SOCS-1 -Actin T cells + - B cells + - Core SOCS-1 -Actin Conclusion: HCV induces a differential regulation of PD-1/SOCS-1 expression, which translate into a differential regulation of T/B lymphocyte functions through Jak/STAT pathway Blocking PD-1 signaling restores T cell activation and proliferation Anti-PD-L1 Control Ab 29.8% 17.1% B) T cell Counts CD69 A) Anti-PD-L1 80% 10% 9% Control Ab 1% 46% 13% 36% 5% HS HCV-Tetramer CD4 21.3% 13.7% CD8 22% 36% 38% 4% 1% 9% 77% CFSE 13% HCV-NHL Why we care about this? -Negative signaling molecules in HCV pathogenesis Differential regulation of IL-12/IL-23 expressions by M/MФ leads to TH17 cell and Foxp3+ Treg development Differential regulation of IL-12/IL-23 expressions by M/MФ leads to TH17 cell development during HCV infection ** HS * IL-12 p35 HCV IL-23 p19 HS ** Pearson r=0.465 p<0.05 IL-17A HCV CD4 IL-23/IL-12 by CD14+ cells Hepatocyte Hepatocyte Hepatocyte TLR TLR monocyte Tim-3 STAT-3 STAT-1 IL-23 HCV IL-12 Tim-3 Foxp3+ Tregs TH17 Gal-9 Differential regulation of IL-12/IL-23 expressions by M/MФ leads to TH17 cell and Foxp3+ Treg development during HCV infection HS A) HCV ** 8.91 11.94 13.54 20.85 74.75 4.40 53.68 11.93 B) HS HCV *** 1.54 5.68 2.44 9.41 52.82 39.95 62.70 25.45 * A) B) HS * HCV HS HCV 25.86 15.78 20.06 7.42 15.94 4.89 14.53 7.26 28.50 29.85 45.08 27.44 62.47 16.7 59.18 19.03 NS ** NS Pearson Correlation = 0.75 Sig. (1-tailed)=0.0002; (2-tailed)=0.0004 Foxp3+ cells in CD4+CD25+ cells 14 12 10 8 6 4 2 0 0 CD4+ CD4+ CD25+ CD4+ CD25+ Foxp3+ CD4+ CD25+ Foxp3- 10 20 30 40 50 Tim-3+CD4+CD25+Foxp3+ cells 60 Differential regulation of IL-12/IL-23 expressions by monocytes/macrophages leads to TH17 cell and CD4+CD25+Foxp3+development during HCV infection HCV-infected hepatocytes produce Gal-9 and TGF-β IL-23/IL-12 IL-17 CD4+ T cell CD25+ FoxP3T eff TGF-β/IL-10 CD25+ FoxP3+ T reg Tim-3 is up-regulated more on Foxp3+ Tregs than on Teffs IL-2 proliferation apoptosis apoptosis proliferation Tim-3/Gal-9 interactions shift the balance of Tregs/Teffs by regulating T cell proliferation and apoptosis Teff Treg Treg α-Tim-3 Moorman JP et al J Immunol 2012 Tim-3 /Gal-9 Treg α-Tim-3 may correct the imbalance of Tregs/Teffs ratio induced by HCV Immunodysregulation during chronic HCV infection HCV-infected Hepatocytes Impaired CD14+ M/MΦ maturation into DC Accumulated TH17 & Foxp3+ Treg cells Increased PD-1, SOCS-1, Tim-3 Decreased IL-12 Increased IL-23 Increased IL-17 HCV chronic infection Increased IL-10 Increased TGF-β Autoimmune disorders Diminished CD4+/ CD8+ T cells Decreased IL-2 Decreased TNF-α Decreased IFN-γ Aberrant CD19+ B cell activation Increased IgG Increased IgM Why we care about this? -Negative signaling molecules in Vaccine response HBV vaccine response and HCV vaccine development Tim-3 on HBV vaccine failure in HCV-infected individuals HBV Vaccine response: 90% in Healthy Subjects; 50% in HCV-infected patients A) *** HBV-R ** Isotype % Tim-3/CD14+ cells HBV-NR % IL-23p19/CD14+ cells % IL-12p35/CD14+ cells B) * PD-1/SOCS-1 on HBV vaccine failure in HCV-infected individuals 12.1% vs 7.0%, P=0.002 18.00% 5.6% vs 4.5%, P>0.05 16.00% 14.00% CD69+ CD4+ T cells 12.00% 10.00% 8.00% 6.00% 4.00% 2.00% 100.00% 90.00% 80.00% 70.00% 60.00% 50.00% 40.00% 30.00% 20.00% 10.00% 0.00% 0.00% Pearson Corr. = - 0.374** Sig.(2-tailed) = 0.001 10.00% 20.00% PD-1+ 0.00% CD4+ 30.00% T cells HCV patients HCV patients HCV resolved Healthy HBV-NR (n=29) HBV-R (n=32) individuals(n=6) Subjects(n=10) HBsAg stimulation HBV-R HBV-NR a-CD3/28 stimulation HBV-R 0.4 HBV-NR SOCS-1 β-actin SOCS-1/actin PD-1 expression on CD4+ T cells 9.4% vs 4.9%, P=0.007 * 0.3 * 0.2 0.1 0 HBV-R HBV-NR HBsAg stimulation HBV-R HBV-NR a-CD3/28 stimulation 40.00% Control Ab 80 18.1% 29.9% HBsAg stimulation 31.6% 57.8% % CD69+ in CD4+ T cells A) a-PD-L1 Ab a-CD3/28 stimulation 70 60 IgG * a-PDL-1 50 * 40 30 20 10 0 Control Ab 0% 0.3% 7% 92% a-PD-L1 Ab 1.5% 8% 18% 73% HBsAg stimulation 100 80 60 IgG a-PDL-1 40 * 20 * 0 M1 100 0% 1.5% 19% 79% 1% 21% 58% 20% a-CD3/28 stimulation CFSE / a-CD3/28 B) CFSE / HBsAg HBsAg stimulation a-CD3/28 stimulation 80 60 M2 M3 M4 IgG * a-PDL-1 40 * 20 * 0 M1 M2 M3 M4 Why do we care - Listeria monocytogenes (Lm)-based DC-targeting HCV vaccine Development HCV vaccine development: HCV-quasispecies; HCV-delivery; HCV-models; HCV-exhaustion Listeria monocytogenes Lm vector HCV antigens Virulence determinants NS5B ∆actA/∆inlB Lm-infected DC Lm-NS5B CD14 Monocyte iDC induced by GM-CSF + IL-4 mDC induced by TNF-α + Poly I:C mDC infected by Lm-HCV vaccine HLA-ABC HLA-DR CD209 CD1a CD80 CD83 CD86 %Tim-3+ cells %IL-12 + cells Why do we care ? Improve Lm-based DC-targeting HCV vaccine by blocking Tim-3 signaling M/MФ BSA-FITC Uptake (ΔMFI) iDC mDC Un-infected HCV HCV+IgG HCV+a-Tim-3 Iso Gating strategy HCV-resolved CD3+CD8+ Tim-3 Lm-control IgG α-Tim-3 Lm-NS5B IgG α-Tim-3 CD3+CD8+ %HCV-Tet+/CD3+CD8+ HCV-Tetramer B) HCV-infected SSC HCV-Tetramer A) %Tim-3+/HCV-Tet+CD3+CD8+ Why do we care? Improve Lm-based DC-targeting HCV vaccine by blocking Tim-3 signaling Why do we care? Listeria monocytogenes (Lm)-based DC-targeting HCV vaccine B) Granzyme-B %GranzymeB+/HCV-Tet+CD3+CD8+ IFN-γ %IFN-r+/HCV-Tet+CD3+CD8+ A) Why do we care?- novel therapeutics MHC/peptide/B7 LPS TLR CD3 CD28 Gal-9 PD-L1 HCV Core Tim-3 PD-1 gC1qR STAT Monocyte IL-12 T cell activation α-gC1qR α-PD-1 SOCS α-HCV core α-Tim-3 Negative T cell regulators T cell dysfunction Improve HBV vaccine response in HCV/HIV-infected individuals viral clearance HCV persistence Improve HCV - DC therapeutic Vaccine Acknowledgements Dr. T. Niki: President of GalPharm, Japan; Dr. T.J. Liang, Chief Liver Dis, NIH NIDDK Dr. T Wakita, Director Virology Lab, NIH, Japan; Dr. D. Brockstedt, VP of Aduro BioTech, CA