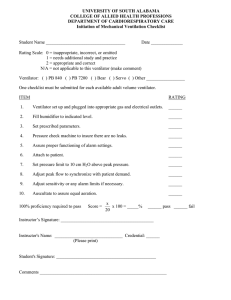
Respiratory Therapy 101 Understanding Oxygen Therapy in less than an Hour
advertisement
Respiratory Therapy 101 Understanding Oxygen Therapy in less than an Hour Oxygen Cannula • Can safely be used at flow rates of 1-6 LPM • Flow should not be turned above 6 LPM • Produces 24% to 44% oxygen to patient Oxygen Cannula Liter Flow % Oxygen 1 2 3 4 5 6 24% 28% 32% 36% 40% 44% Oxygen Humidifiers • Used with oxygen cannulas to prevent nasal drying • May not be used at flow rates less than 3LPM (need to bubble to be effective) • Check water level and change as needed Oxygen Humidifiers Reservoir Cannulas • Stores oxygen in a reservoir on exhalation so the patient has more oxygen available on inhalation • Capable of providing higher oxygen percentage at a lower flow rate Two styles of Reservoir Cannulas Simple Oxygen Mask • Flow rate should be from 5 to 10 LPM • Flow rate should NOT be Less than 5 LPM • Oxygen delivery is approximately 35% to 50% • Short term use only • No Humidity Simple Mask 100% Non-Rebreather Mask • Set oxygen flow to a setting that does not allow the reservoir bag to collapse with the patient’s inspiration (10 – 15 LPM) • If tight fitting to patient’s face, 100% oxygen can be given • Usual oxygen percentage is 60% to 80% • USED BY EMS Non-rebreather Masks High Flow Systems Air Entrainment Mask (Venturi) • Percent of oxygen delivered depends on the LPM flow, the size of the jet, and the size of the entrainment port • Delivers a precise oxygen percentage • Entrainment ports must be kept open • Most accurate way to deliver O2 • Ideal for CO2 retainers High Flow System Air Entrainment Mask High Flow System Air Entrainment Mask • The flow of 100% oxygen through the mask and draws in a controlled amount of room air (21 per cent oxygen). • Commonly available masks deliver 24, 28, 31, 35, or 40 per cent oxygen. At concentrations above 24 per cent, humidification may be required. (Color coded – depending on manufacturer) High Flow System Air Entrainment Mask Oxygen Blender • Controls precisely the percent of oxygen the patient is receiving • High flow meter is required for use Oxygen Blender How do I know if my Patient is Oxygen Deprived??? ? Clinical Respiratory Signs of Hypoxia MILD to MODERATE • Tachypnea • Dyspnea • Paleness SEVERE • Tachypnea • Dyspnea • Cyanosis Cardiovascular Signs of Hypoxia MILD to MODERATE • Tachycardia • Mild Hypertension • Peripheral Vasoconstriction SEVERE • Tachycardia, eventual bradycardia, arrhythmia • Hypertension and eventual hypotension Neurologic Signs of Hypoxia • • • • MILD to MODERATE Restlessness Disorientation Headaches Lassitude SEVERE • • • • • • • • • Somnolence Confusion Distressed appearance Blurred Vision Loss of Coordination Impaired judgment Slow reaction time Manic-Depressive activity Coma Monitoring Oxygen with an Oximeter • Monitors the adequacy of arterial oxyhemoglobin saturation • Usually maintained at values above 90% • Only provides valuable data when patient has normal hemoglobin • Light and nail polish can alter saturation readings ETCO2 Monitoring ETCO2 – measures ventilation, not saturation (end product of breathing is CO2) (See pamphlet) Used with post surgical patients on PCA pumps, Epidurals and Mechanically Vented patients Monitoring Oxygen with ABG’s • Pa02 reflects oxygenation levels • Normal Pa02 is 80-100mmHg (<60 mmHgneeds intervention). • Pa02 Values below 55 mmHg are Critical • Normal Pa02 values decrease with age • Hypoxemia – low PaO2 <80 ABG Review • pH = 7.35 to 7.45 <7.35 Acidic and > 7.45 Alkalotic • PaC02 = 35 to 45 • HC03 = 22-26 (28) • Cost of ABG ($800-$1500/draw) • Invasive Procedure • ROME = Respiratory – Opposite direction Metalbolic – Equal (same) direction What is CPAP??? • Continuous Positive Airway Pressure • Application of positive pressure to a patient’s airway throughout the respiratory cycle • Increases the patient’s FRC (functional residual capacity) • Improves oxygenation • Also, used to prevent airway collapse in treatment of obstructive sleep apnea What is BiPAP?? Non-Invasive Positive Pressure Ventilation (NIPPV) • Provides two levels of pressure to the patient • One pressure on the inspiration (IPAP) • One pressure on the expiration (EPAP) • May be used in patients with acute, short-term respiratory problems to avoid intubation and invasive mechanical ventilation • Improves the ability to remove CO2 and provide O2 Facial and Nasal Masks Non-Invasive Positive Pressure Ventilator Support FiO2 • Fractional concentrated of inspired oxygen delivered • Percentage of Oxygen delivered or participating in gas exchange in the alveoli (0.21 to 1.0) • Expressed in %. (0.35 is 35%). Oh my GOD!! My patient is on a ventilator! Drager Ventilator BASIC VENTIALTOR MODES 1. VOLUME CONTROLLED – – tidal volume (volume of air inhaled) 1. PRESSURE CONTROLLED – – PIP (positive inspiratory pressure) Basic Ventilator Parameters Breath Rate (f) • Number of times per minute that inspiration is initiated (controlled by ventilator, patient or combination of both). • Two things to know: »Ventilator Setting (rate) (f) »Patient Rate (BPM) • Rate (f) setting and Patient breathing rate are not the same thing Basic Ventilator Parameters Tidal Volume (vT) • Amount of gas delivered during an inspiration in ml or liters • Average adult tidal volume is 500-550 ml or .500 -.550 L • Setting in volume control modes • Not a setting but volume readings are measured in pressure control modes Basic Ventilator Parameters Peak Inspiratory Pressure (PIP) • Maximum pressure reached in the ventilator system during inspiration • Set parameter in pressure setting modes (Pressure Controlled Ventilation PCV) PEEP • Positive End Expiratory Pressure • Application of a constant, positive pressure such that at the end of exhalation, airway pressure does not return to zero • Improves oxygenation Basic Ventilator Parameters Breath Types • Mandatory – ventilator controls all parts of breathing • Spontaneous – patient controls all parts of breathing • Assisted Breaths – patient controls breathing rate, breaths are assisted with a set Vt (tidal volume) Basic Ventilator Parameters Common Modes of Ventilation • • • • • • CMV A/C VC SIMV SIMV + PS PSV CMV Mode (volume) most common type used is Assist Control (A/C) • • • • Continuous mandatory ventilation Continuous mechanical ventilation Every breath is mandatory or assisted Set minimum breath rate – CMV – patient does not determine breathing rate. – A/C – patient determines breathing rate. • Patient does not work • Delivery of a mandatory or assisted breath at a set rate SIMV Mode (volume , sometimes pressure) • A minimum number of breaths delivered with a tidal volume (assisted) is set on the ventilator. – Respiratory rate and tidal volumes are set • Patient may breath spontaneously between the number of set assisted breaths • Weaning mode (usually) • Set PEEP and sometimes pressure support is set Pressure Controlled Ventilation (pressure) • Delivers breaths at a preset pressure limit (equal to PIP). • When ventilator delivers a breath, it continues delivering the volume until the pre-set pressure limit is reached, then it stops delivering the breath. • Settings: Pressure limit (PIP) and I:E ratio but not the tidal volume (tidal volume will vary). • IMPORTANT NOTE: “unnatural feeling of breathing” – NEEDS SEDATION! • With control modes – increases mean airway and intrathoracic pressures rise, may decrease Cardiac Output, very important to monitor hemodynamics (BP, HR, CVP) Pressure Support Ventilation PSV (pressure) • Augments or assists spontaneous breathing efforts by delivering a high flow air to a selected pressure level early in inspiration and maintains that level throughout the inspiratory phase. • When PSV is used as a stand-alone mode the pressure support level is adjusted to achieve the targeted tidal volume and respiratory rate. (Vt and f are not set - patient determines own respiratory rate and tidal volume • Reduces the work of breathing for the patient by reducing the resistance of breathing through an ET tube and circuit tubing. • A lot of time this mode is combined with SIMV and CPAP mode. • At High pressures PSV can provide nearly total ventilator support. • Because level of pressure can be gradually decreased, endurance conditioning is enhanced in PSV modes. Great for weaning! CPAP Mode (pressure) • Not the same as CPAP by mask at home or is it???? • Supplies pressure throughout the respiratory cycle, helping to improve oxygenation in spontaneously breathing patients. • No setting on ventilator for rate or tidal volumes (patient determines own rate and their own tidal volume). • FiO2, PEEP, PS (pressure support) can be set. • Should not over sedate people on this mode. • Monitor breathing rate, apnea alarms!! • May be used on intubated or non-intubated patients via mask. Alarms • • • • • • • High inspiratory pressure or pressure limit Low inspiratory pressure Low exhaled tidal volume High or low minute volume Apnea High rate or frequency Low PEEP/CPAP High Inspiratory Pressure Alarm • • • • • • Coughing Secretions in the airway Biting on the ET tube Bronchospasm Patient Ventilator asynchrony Kinking of ventilator circuit Low Inspiratory Pressure • • • • Low exhaled volume Patient Disconnected Circuit Leaks Airway leaks When in Doubt Always Ask!! Your Respiratory Therapist Is Your Friend!!!!!!! They are here to help! And to keep your patients breathing forever!