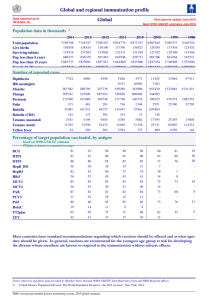
Tetanus
advertisement

TETANUS Assist Prof Microbiology College of Medicine, Majmaah University LEARNING OBJECTIVES 1. Explain etiology, pathogenesis and mechanism of transmission 2. Discuss the mechanism of action of tetanus toxin 3. Discuss the role of immunization in primary and secondary prevention of tetanus TETANUS-ETIOLOGY • Tetanus is caused by Clostridium tetani • Gram positive anaerobic bacillus • One of two genera that form spores • Two forms: vegetative form and spore form • Vegetative form: actively secretes toxin and cause disease • Spore form: Dormant and metabolically inert, important in disease transmission TETANUS-ETIOLOGY • Spores present in soil, dust, manure, dirty metallic objects e.g. nails, sharp rusted metallic objects, wood pieces, etc. • Spores excreted in feces of horse, sheep, chicken and other animals • Soil mixed with feces-spores remain in soil for long time • Non communicable disease VIDEO TETANUS INTRODUCTION TETANUS-TRANSMISSION • Non invasive disease • C. tetani remains localized to devitalized tissue • Spores (& not Vegetative form) are important in disease transmission • Spores enter body through cuts, lacerations, deep wounds, puncture wound etc. • Neonatal tetanuscontaminated equipments to cut umbilical cord • African nation-ritual of putting animal dung on umbilical stump TETANUS-TRANSMISSION • The spore can get into the body through broken skin -injuries from contaminated objects. • Breaks in skin more likely to get infected • • • • • Wounds contaminated with dirt, feces, spit (saliva) Puncture wounds- nail, needle, thorn Burns Crush injuries Injuries with dead tissue • Rare ways of transmission • Clean superficial wounds, surgical procedures, insect/ animal bites, compound fractures, I/V drug users TETANUS-PATHOGENESIS • Incubation Period- 3-21 days(1day-several months) • Average IP 10 days • Spores carried deep inside wound • Anaerobic atmosphere: dead tissue, deep in tissue, foreign body, co-infection with aerobic organisms • Spores germinate into vegetative form TETANUS-PATHOGENESIS • Vegetative form remain localized to wound • Secrete toxin Tetanospasmin • Active fragment binds to pre-synaptic motor neurons • Retrograde axonal transport- to spinal cord and brain stem • Toxin diffuses to inhibitory cells-Glycinergic and GABAergic neurons • Toxin degrades Synaptobrevin-docking protein of pre-synaptic vesicles TETANUS-PATHOGENESIS • Release of inhibitory neurotransmitters Glycine & GABA is blocked • Uninhibited spastic contraction of muscles • Hyper-reflexia, spastic paralysis of muscles • Lock jaw, trismus, neck stiffness, difficulty swallowing • Opisthotonus VIDEO NEUROTRANSMISSION TETANUS-PATHOGENESIS COMPLICATIONS • Laryngospasm • Fractures • Hospital-acquired infections • Pulmonary embolism • Aspiration pneumonia • Breathing difficulty, possibly leading to death (10-20% of cases are fatal especially very young and old) VIDEO NEONATAL TETANUS TETANUS PREVENTION PRIMARY PREVENTION A. PREGNANT LADIES – Tdap between 27 & 36 weeks B. NEWBORNS – DTaP -2,3,4 months C. PRE-SCHOOL (3-5 years) – DTaP booster D. ADULTS(13-18 years) – Single Td booster E. ADULTS >19 Years not received Tdap & F. PERSON >65 Years-should get Tdap TETANUS PREVENTION SECONDARY PREVENTION IMMUNIZATION STATUS FULLY IMMUNIZED NOT IMMUNIZED OR INCOMPLETE Minor wound No immunization Active immunization with tetanus toxoid Tetanus prone wound Tetanus Immunoglobulins (TIG) single dose Tetanus toxoid & TIG TETANUS TREATMENT 1. Wound debridement 2. Antimicrobial therapy: Metronidazole preferred over Penicillin G 3. Penicillin G -structurally similar to GABA and competitively antagonizes this neurotransmitter 4. Management of clinical tetanus: Human tetanus immunolobulin (TIG) 5. General supportive management e.g. airway management, physiotherapy etc. 6. Spasmolytics MCQ Tetanus 1. 2. 3. 4. 5. Is caused by Clostridium botulinum Causative organism secretes toxin tetanolysin Has an average incubation period of 3 days Is not a contagious disease Vegetative form is important in disease transmission MCQ A 21-years-young boy met RTA and sustained multiple deep penetrating wounds on body. He has never been vaccinated for any disease in his life. Regarding secondary prevention of tetanus for this man, which of the following vaccination protocol should be followed? 1. 2. 3. 4. Tetanus toxoid only Tetanus toxoid and TIG TIG only Neither Tetanus toxoid nor TIG MCQ A 39-years-old lady is brought to ER with clinical diagnosis of tetanus after a penetrating wound sole 15 days back. Regarding management of tetanus, what should be line of action? 1. Inquire about her immunization status of tetanus 2. Give tetanus toxoid irrespective of her immune status 3. Give her TIG as a management protocol 4. Reassure the relative as she does not need any immunization at present MCQ What causes the major symptoms of tetanus? 1. 2. 3. 4. 5. Multiplication of the organisms at the site of infection Production of botulin toxin Super-infection due to antibiotic therapy Bacteria multiplying in the bloodstream Production of tetanospasmin