neoplasia 2
advertisement

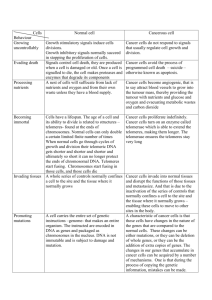
NEOPLASIA - II Dr. Saleem Shaikh Characteristics of Tumours Majority of the neoplasms are categorised clinically and morphologically into benign and malignant on basis of certain characteristics – 1. Rate of growth 2. Cancer phenotype and stem cells 3. Clinical and gross features 4. Microscopic features 5. Local invasion 6. Metastasis (distant spread) Local invasion Most benign tumors are encapsulated or circumscribed masses, they expand and push the surrounding normal tissues, without invading or infiltrating Malignant tumors also expand and push the surrounding tissues but they also spread by invasion, infiltration and destruction of surrounding tissues. They start to invade through the path of least resistance. Metastasis It is the spread of tumour from one site to the another, which is not anatomically connected to each other. Metastasis and invasiveness are the two most important features which distinguish benign and malignant tumors. Routes of metastasis: Lymphatic spread Hematogenous spread Spread along body cavities In general - Carcinomas spread by lymphatic route, the lymph nodes draining the tumour site will be invariably involved, this is known as regional lymph node metastasis. Some times the immediate lymph nodes may not get involved, instead the lymphnodes at a distant site my be involved this is known as “skip metastasis” Hematogenous spread or blood borne metastasis is a common route for sarcomas, but some carcinomas may also spread by this route. Hematogenous metastasis may be seen commonly in liver, lungs, kidney, brains and adernals. This supports the ‘seed-soil’ theory. These organs have good blood supply hence – good soil. Very rarely tumors may spread along body cavities. Grading & Staging of Cancer ‘Grading’ & ‘staging’ are two systems to predict tumour behaviour and guide therapy after a malignant tumour is detected. Grading is defined as the gross and microscopic degree of differentiation of the tumour. Staging is the extent of spread of the tumour within the patient. Grading is histological while staging is clinical Many systems of grading are seen, the most common and relevant is ‘Broders Grading’ - well differentiated, moderately well differentiated, poorly differentiated. Staging - TNM staging for squamous cell carcinoma T – tumour N – lymph node involvement M- metastasis Carcinogenesis Carcinogenesis (oncogenesis or tumorigenesis) means the mechanism of formation of tumors – pathogenesis of tumors. The agents which induce the tumor are known as carcinogens The carcinogens and carcinogenesis can be discussed under these headings: Molecular pathogenesis of cancer (genes and cancer) Chemical carcinogenesis Physical carcinogenesis Biological carcinogenesis Then genetic mutation in tumors may occur on its own or may be caused by chemical, physical or biological carcinogens. Molecular pathogenesis of cancer How a cell can transform into a cancer is complex and even till now 1. 2. 3. 4. all the various mechanisms have not been completely understood. In normal cell growth, there are 4 regulatory genes: Proto-oncogenes: these are growth promoting genes Anti-oncogenes: growth inhibiting or supressing genes Apoptosis regulatory genes: control programmed cell death DNA repair genes: repair minor DNA damage In cancer proto-oncogenes convert into oncogenes and promote cell proliferation. Inactivation of anti oncogenes, Abnormal apoptosis genes Failure of DNA repair genes P53 gene This an example of anti-oncogene or tumor suppressor gene. Located on short arm of Chromosome 17 In normal cells it is present in small amounts but accumulates after DNA damage Two major functions of P53 in normal cell cycle Blocks mitotic activity: if there is any damage to DNA, this gives the cell time to repair the DNA, before it is replicated into more number of cells. Promotes Apoptosis: if the DNA damage is greater and can not be repaired by inbuilt mechanisms, then this gene activates the factors of apoptosis P53 is also called as the protector of genome Chemical carcinogenesis The first etiologic factors for tumors to be discovered were chemicals. Basic mechanism of chemical carcinogenesis is by induction of mutation in proto-oncogenes and anti-oncogenes. Chemical carcinogenesis involves three steps 1. Initiation: may be a single dose or by multiple doses. May be Direct or Indirect. 2. Promotion: substances which do not cause any change in the cell but can enhance the damage in a cell. 3. Progression: cell has already converted into a tumor cell and only proliferates in this stage. An initiator may cause cancer without the presence of promoter but a promoter can never cause cancer it can only enhance the effects of initiator (oestrogen - harmone) Physical Carcinogenesis Physical agents can be grouped in two – Radiation Nonradiation Radiation carcinogenesis: Ultraviolet light and ionising radiation are the two main forms of radiation carcinogens. Ultraviolet light: the main source of UV light is the sunlight, UV rays usually penetrate only a few millimeters into the skin and hence there effect is limited to the epidermis of the skin. Exposure to UV light causes basal cell carcinoma, squamous cell carcinoma, melanoma. Mostly seen in fair skinned individuals. XERODERMA PIGMENTOSUM Physical Carcinogenesis Ionising radiation: these rays include x-rays, α- rays,β-rays and γ- rays. These rays penetrate more deep and hence cause many kinds of cancers, like leukaemia, skin, lung, uterus cancers, osteosarcomas etc. High incidence of tumors was seen in x- ray workers and radiotherapists. High incidence of osteosarcoma in girls working in watch factories. Japanese atom bomb survivors Non radiation carcinogenesis: by heat or in healing wounds etc. Biological Carcinogenesis (viral) Biological carcinogens are usually viruses, very rarely fungal, bacteria or parasites may be involved. Based on the nucleic acid content, oncogenic virus can be grouped into 2 groups DNA & RNA oncogenic viruses RNA viruses have more mutation potential than DNA viruses In general prolonged persistence of virus after infection, may cause mutation in the involved cell, DNA or RNA virus causes activation of growth promoting pathways and inhibition of growth suppressor genes in the infected cells. Such cells after multiplication produce cells which have increased growth potential.