respiratory 4
advertisement

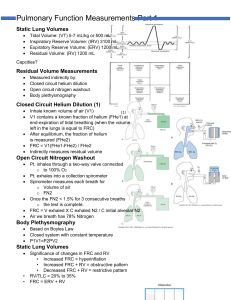
Respiratory Assessment DR. MOHAMED SEYAM PHD. PT. ASSISTANT PROFESSOR OF PHYSICAL THERAPY INVESTIGATION Arterial Blood Gas(ABG) The body produces acids daily: - 15,000 mmol CO2 and - 50 -100 mEq Nonvolatile acids (an acid produced from sources other than carbon dioxide). The lungs and kidney attempt to maintain balance by eliminating CO2 by secretion of H+ and HCO3 reabsorption. The Components: pH / PaCO2 / PaO2 / HCO3 Normal Arterial Values pH - 7.35 - 7.45 PaCO2 - 35-45 mmHg PaO2 - 80-100 mmHg HCO3 - 22-28 mEq/L Respiratory Acidosis pH, CO2 , Ventilation oCauses 1) CNS depression 2) Lung diseases like COPD/ARDS, Pneumothorax, 3) Diaphragmatic paralysis, Restrictive lung disease. 4) Musculoskeletal disorders(Myasthenia gravis, Guillain Barre syndrome) Respiratory Alkalosis pH, CO2, Ventilation Causes 1) Intra cerebral hemorrhage (Head injury) 2) Anxiety – decrease lung compliance 3) Cirrhosis of the liver 4) Sepsis 5) Pulmonary Embolism 6) Pneumonia 7) Asthma Metabolic Acidosis pH, HCO3 Causes 1. Lactic acidosis-is when lactic acid builds ups in the bloodstream faster than it can be removed. 2. Keto acidosis ( Associated with Diabetes) It occurs when the body cannot use sugar (glucose) as a fuel source because there is no insulin or not enough insulin. By products of fat breakdown, called ketones, build up in the body. 3. Renal failure 4. Chronic diarrhea Metabolic Alkalosis pH, HCO3 Causes 1) Vomiting 2) Diuretics 3) - Diuretics cause the kidneys to remove more sodium and water from the body 4) Hypokalemia - A drop in potassium level. 5) Renal Failure Pulmonary Function test Spirometry is a medical test that measures the volume of air an individual inhales or exhales as a function of time. Pulmonary function studies are commonly subdivided into the following 1. Lung volumes and capacities 2. Forced expiratory flow rate 3. Pulmonary diffusion capacity measurements USES OF PULMONARY FUNCTION TEST ◦ To evaluate respiratory symptoms To determine severity of impairment in patients with known respiratory disease ◦ To follow the course of disease in a patient, including the response to therapy To assess preoperative risk for predicting postoperative respiratory complications To screen for subclinical disease Technique Have patient seated comfortably Closed-circuit technique Place nose clip on Have patient breathe on mouthpiece Have patient take a deep breath as fast as possible Blow out as hard as they can until you tell them to stop Forced vital capacity (FVC) Total volume of air that can be exhaled forcefully from TLC The majority of FVC can be exhaled in <3 seconds in normal people, but often is much more prolonged in obstructive diseases. Measured in liters (L) Forced vital capacity (FVC): Interpretation of % predicted: 80-120% Normal 70-79% Mild reduction 50%-69% Moderate reduction <50% Severe reduction Forced expiratory volume in first second: (FEV1) Volume of air forcefully expired from full inflation (TLC) in the first second Measured in liters (L) Normal people can exhale more than 75-80% of their FVC in the first second; thus the FEV1/FVC can be utilized to characterize lung disease Interpretation of % predicted: > 75% Normal 60%-75% Mild obstruction 50-59% Moderate obstruction < 49% Severe obstruction FEV1/FVC ratio Thus compares the amount of air exhaled in 1 second with the total amount exhaled during an FVC maneuver. FEV 1/FVC ratio should be 80% or greater. FEV 1/FVC ratio is DECREASED in COPD FEV 1/FVC ratio is NORMAL or INCREASED in Restrictive lung disorders Flow volume Loop The flow volume loop is a graphical illustration maximum expiratory and inspiratory flowvolume curves • Useful to help characterize disease states (e.g. obstructive vs. restrictive) Obstructive Disorders -Characterized by a limitation of expiratory airflow Examples: asthma, COPD -Decreased: FEV1, FEF25-75, FEV1/FVC ratio (<0.8) -Increased or Normal: TLC Restrictive disorders -Characterized by diminished lung volume due to: • Change in alteration in lung parenchyma (interstitial lung disease) • Disease of pleura, chest wall (e.g. scoliosis), or neuromuscular apparatus (e.g. muscular dystrophy) FINDINGS -Decreased TLC, FVC -Normal or increased: FEV1/FVC ratio Measurements of the Residual Volume 1. Closed Circuit helium dilution test 2. Open circuit nitrogen test 3. Body Plethysmography Chest Radiographs (chxR) Chest radiographs provide a static view of the anatomy of the chest and they may be used to screen for abnormalities. Standard views: 1) Posterior anterior(PA): Patient in the standing position with the front of the chest facing the film cassette. 2) Anteroposterior(AP) OTHER VIEWS OF CHEST X RAY 3) lateral view : Taken at bedside 4)Decubitus view: To confirm the presence of an air-filled level in the lungs /pleural effusion. 5) Lordotic view: Visualize the apical or middle lobes. 6)Oblique: To detect pleural thickening, evaluate carina, see heart and great vessels.Position – standing diagonally Steps for assessment of chest x-ray Assess the technical quality Evaluate the location of all catheters, tubes and support devices. Assess cardio vascular system status Check for abnormal parenchymal opacities Evidence of barotrauma Look for pleural effusions Bones and soft tissues: Size, shape, symmetry of bony thorax, vertebral body faintly visible Determine whether patient is rotated to either side (distance from medial end of clavicle to spinous process) Width of intercostal space(↑space means ↑thoracic volume) Rounded, smooth sharply defined shadow of hemi diaphragms (Right side 1-2 cm higher than left) Diaphragm elevated- if less than 9 ribs visible above the level of domes. Diaphragm Depressed- if more than 10 ribs visible. Costophrenic angles: where hemi diaphragm meet the chest wall at the lateral aspect. Opacification of this angle – Pleural thickening/ Pleural effusion Cardio phrenic angle: Where hemi diaphragm meets the borders of the heart Bronchography : It is an x-ray of the bronchus involving the use of contrast. Evaluation of some congenital pulmonary anomalies. Bronchoscopy : Permits direct visualization of inaccessible areas of bronchial tree. It is indicated to assess for infection that cannot be evaluated from a sample or to assess for malignancy. Thank you