13th lecture
advertisement
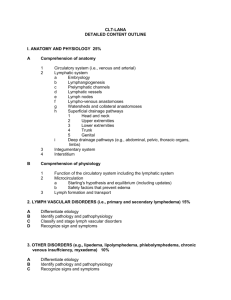
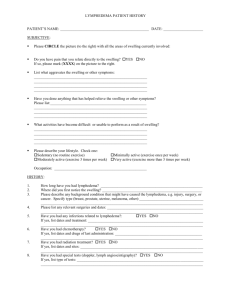
PERIPHERAL VASCULAR DISEASES DR. Mohamed Seyam PhD. PT. Assistant Professor Of Physical Therapy For Cardiovascular /Respiratory Disorder Lymphatic system( tissues and vessels) • The lymphatic system filters and collects lymph and large molecules in the interstitial space that come from the intravascular space. • unidirectional • Consists flow and no circulation. of • Lymph node, thymus, spleen and nodules • Lymph vessels • Right lymphatic duct and Thoracic duct • lymph Lymphedema • Lymphedema is an abnormal accumulation of high-protein concentrated fluid, usually in the arms and legs. • Lymphedema is described as an abnormal collection of protein, edema, fibrosis and chronic inflammation. Risk Factor (Secondary): Surgery • Any surgery that dissects or removes lymph nodes increases the risk of lymphedema by impairing the lymph flow. • Common cancers that may require surgical alterations of the lymph nodes include breast cancer, head and neck, prostate, testicular, bladder, or colon cancer. • Surgical disruption of • Vascular surgery lymphatic system • Risk Factor: Radiation Radiation therapy to the axillary or groin region around the lymph node can cause fibrosis and scarring of the tissue and therefore cause lymphedema to occur Types of Lymphedema 1- Pitting edema Short duration edema Finger indentation of the skin 2- Brawny edema Tissue feels hard upon palpation Indicates fibrotic changes 3- Weeping Fluid leaks, wound healing is impaired Occurs mostly in the lower extremities Stages of lymphedema Stage I • Considered reversible • There is lower than 3 cm difference between extremities. Stage II • Considered irreversible • There is 3 to 5 cm difference between extremities. Stage III • Tissues are hard and may have cartilage formation developing. • There is more than 5 cm difference between extremities. Signs and symptoms • Painless swelling of the arms or legs. • Swelling • Redness get worse during the day and better at night. and Warmth in the extremity. • A feeling of tightness and weakness in the affected extremity. • Bracelets, • Tends rings, or shoes may become tight. to occur distal to proximal • Increased pigmentation/superficial veins • Secondary cellulitis Measurement Methods Water displacement – “gold standard” 2. Circumference 3. Perometry 4. Bioelectrical impedance 1. Water Displacement (Volumetric measurement) “Gold standard” for volume measurement (edema size) 1- Water displacement – “gold standard Circumference Most commonly used method to assess limb volume Measurements taken at various points of arm or leg Time-consuming Requires considerable experience 2- Circumference Examination (Cont) - Girth measurements of the extremity (evaluating edema size). Limb measurements must be done at the set levels and ideally repeated by the same person. These measurements are taken in: 1. The upper limb at: (a) Axilla. (b) 8 cm proximal to olecranon. (c) 11 cm distal to olecranon. (d) Wrist. (e) Level with web of thumb Upper limb circumference. Examination (Cont) 2. (a) (b) (c) (d.) (e) The lower limb at: Groin 15 cm above base of patella. 15 cm below apex of patella. Ankle (malleoli). Middle of metatarsals. lower limb circumference. Perometry Imaging device Measures limb volume, circumference, contour, cross-sectional area Convenient Expensive 3- Perometry 4- Bioelectrical impedance Physical Therapy Components Of A Decongestive Lymphatic Therapy Program 1. Elevation 2. Manual lymphatic drainage 3. Compression bandaging and Garment 4. Exercise 5. Pneumatic Pumps 6. Electro modalities 7. Skin care 8. Daily living precautions 1- Elevation *Elevate the involved limb when using a sequential compression pump *Elevate limb when sleeping, resting, and during sedentary activities *Compressive bandages or garment should be worn during periods of elevation 1- Position Elevation of the feet for 10-15 minutes 3-4 times a day 2- Manual Lymphatic Drainage * Slow, very light, repetitive stroking and circular massage movements performed in a specific sequence, limb elevated whenever possible. * Proximal congestion in the trunk, groin, buttock, or axilla is cleared first. * Direction of massage is towards specific lymph nodes. * Usually involves distal to proximal stroking. 3- Compression bandaging and Garment. * Compression Garments. * Once a manageable size has been achieved from wrapping, a compression stocking may be worn to maintain the size and prevent increased swelling. * Bandages may be applied to increase tissue pressure and counteract the elastic insufficiency of the connective tissue. Compression Bandaging Bandages may be applied to increase tissue pressure and counteract the elastic insufficiency of the connective tissue. Thiadens, 2005 Used with permission from lymphacare.com Compressive Bandages 4- Exercise Exercise * Active range of motion, stretching, circulatory and low-intensity resistance exercise is incorporated with manual drainage techniques. * Exercises should be performed with compressive bandages or garment * Exercises are performed in a specific sequence, often with the limb elevated * Low-intensity cardiovascular/pulmonary endurance activities. * Deep breathing and relaxation. Exercises Elbow flexion Elbow extention 10 repetitions each Shoulder horizontal adduction Shoulder abduction Shoulder flexion 5- Sequential, Pneumatic Pumps 3- Compression pump (pneumatic pump unit) •Contraindications •Indications •Varicose veins •Thrombosis •Lymphedema •Kidney or cardiac diseases •Chronic venous insufficiency •Cancers Vasotrain 447 6- Electro modalities • Ultrasound : Pulsed , 0.1-0.3 W/cm2; for 5-8 minutes • Pulsed ultrasound at a lower intensity will produce mechanical and non thermal effects that will soften fibrotic tissues. • Ultrasound may be used for its fibrinolitic effects on lymphostatic fibrosis. 7- Good skin care • Keep the skin clean and dry • Apply moisturizer daily • Protect skin with sunscreen and insect repellant • Use care with razors • Wear gloves during activities • Avoid extreme temperatures Daily living precautions • No blood draws, finger pricks for blood sugar testing, IVs, blood pressures, or injections should be taken on the affected extremity. • Anything that may cause pressure needs to be avoided including: *Blood pressure cuffs *Tourniquets *Tight clothes (waist bands, bra straps, socks) • This constricts collateral circulation Precautions • Heat may cause vasodilatation, which causes more fluid to move from the blood vessels into the tissues. Avoid hot showers and saunas. • Cold may cause rebound swelling or chapped skin • Air travel more than 2 hours increases the risk of swelling because of continuous reduction of cabin pressure. • It is recommended to wear a compression stocking while flying. • Avoid carrying a purse, briefcase, or other heavy item with the affected extremity. • If the lower extremity is affected, avoid standing or sitting for long periods of time and do not cross legs.