Unit 4 Allergies and Immune Responses
advertisement

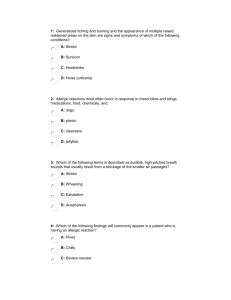
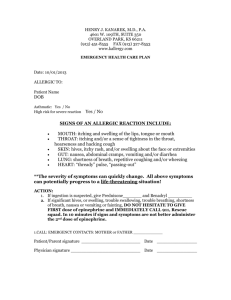
Unit 4 Allergies and Immune Responses • Every year, at least 1,000 Americans die of allergic reactions. When managing allergy-related emergencies, you must be aware of the possibility of acute airway obstruction and cardiovascular collapse and be prepared to treat these lifethreatening complications. • You must also be able to distinguish between the bodys usual response to a sting or bite and an allergic reaction, which may require epinephrine. • Your ability to recognize and manage the many signs and symptoms of allergic reactions may be the only thing standing between a patient's life and imminent death. • The immune system protects the human body from substances and organisms that are foreign to the body Without the immune system for protection, life as you know it would not exist. an allergic reaction, an exaggerated immune response to any • substance, is not caused directly by an outside stimulus, such as a bite or sting. Rather, it is a reaction by the body's immune system, which releases chemicals to combat the stimulus.. • Among these chemicals are histamines and leukotrienes, both of which contribute to an allergic reaction. An allergic reacrion may be mild and local, involving hives, itching, or tenderness, or it may be severe and systemic, resulting in shock and respiratory failure • Anaphylaxis is an extreme allergic reaction that is life threatening and involves multiple organ systems. In severe cases, anaphylaxis can rapidly result in death. • One of the most common signs of anaphylaxis is wheezing, a high-pitched, whistling breath sound that is typically heard on expiration, usually resulting from • broncho spasm,/bronchoconstriction and increased mucus production • Urticaria consists of small areas of generalized itching or burning that appear as multiple, small, raised areas on the skin • You may also note hypotension as a result of hypovolemic shock due to increased capillary permeability . The most common allergens, however, fall into the following five general categories: • 1- Insect bites and stings • When an insect bites you and injects the bite with its venom, the act is called envenomation. • The reaction may be local, causing swelling and itchiness in the surrounding tissue, or it may be systemic, involving the entire body. Such a total body reaction would be considered an anaphylactic reaction. • • 2-Medications. • injection of medications such as penicillin may cause an immediate (within 30 minutes) and severe allergic reaction . • However, reactions to oral medications, such as oral penicillin, may be slower in onset (more than 30 minutes) but equally severe. • 3-Plants. • individuals who inhale dusts, pollens, or other plant materials to which they are sensitive may experience a rapid and severe allergic reaction. • 4-Food. • Eating certain foods, such as shellfish or nuts, may result in a relatively slow (more than 30 minutes) reaction that still can be quite severe. The person may be unaware of the exposure or inciting agent. • 4-Chemicals. • Certain chemicals, makeup, soap, latex, and various other substances can cause severe allergic reactions. Primary Assessment • When a patient presents with an allergic reaction, you should perform a rapid scan of the patient to identify and treat any immediate or potential life threats. By paying careful attention to the patients ABCs, you will be able to maintain breathing and circulation until you are able to transport the patient to the emergency department. • form a General Impression • Allergic reactions may present as respiratory distress or as cardiovascular distress in the form of shock. • Patients experiencing a severe allergic reaction will often be very anxious and feel like they are going to die • Airway and Breathing • The most severe form of allergic reactions, anaphylaxis, can cause rapid swelling of the upper airway. You may have only a few minutes to assess the airway and provide lifesaving measures; however, not all allergic reactions are anaphylactic reactions • Work quickly to assess the patient to determine the severity of the symptoms. • Position the conscious patient in a tripod position leaning forward. This will help to facilitate air entry into the lungs and may help the patient to relax. • Quickly listen to the lungs on each side of the chest. If wheezing or a silent chest is heard, the lower airways are also closing, preventing oxygen from entering the circulatory system. • Do not hesitate to initiate high-flow oxygen therapy • You may have to assist with ventilations for a patient in severe respiratory distress with a severe allergic reaction. This can be done in a semi responsive or an unresponsive patient. • The positive-pressure ventilations you provid will force air through the swelling in the throat and into the lungs while you are waiting for more definitive treatment. In severe situations such as these, the definitive care needed is an injection of epinephrine. • Circulation • some patients in anaphylaxis may not present with severe respiratory symptoms but primarily with signs and symptoms of circulatory distress, such as hypotension. • Palpating a radial pulse will help you to identify how the circulatory system is responding to the reaction. • If the patient is unresponsive and without a pulse, begin basic life support measures or use an automatic external defibrillator if necessary • Assess for a rapid pulse rate; pale, cool, cyanotic or red, moist skin; and delayed capillary refill times that indicate hypo perfusion. • Your initial treatment for shock should include oxygen, positioning in a shock position, and maintaining normal body temperature. • The definitive treatment for anaphylactic shock is epinephrine • Transport Decision • Always provide prompt transport for any patient who may be having an allergic reaction. Take with you all medications and auto-injectors the patient has at the time. History taking • SAMPLE History If the patient is responsive, begin with obtaining the SAMPLE history and asking the following questions specific to an allergic reaction: Have any interventions already been completed? Do you have any prescribed, preloaded medications for allergic reactions? Secondary assessment • Physical Examinations The secondary assessment may help direct treatment. Perform evaluations of the respiratory system. Thoroughly assess breathing, including increased work of breathing, use of accessory muscles, head bobbing, tri- pod positioning, nostril flaring, and grunting. Carefully auscultate both the trachea and the chest. • Wheezing occurs because of narrowing of the air passages, which is mainly the result of contraction of muscles around the bronchioles in reaction to the allergen, and mobilization of mucus in an attempt to "push" out the allergen • Stridor, a harsh, high-pitched inspiratory sound, occurs when swelling in the upper airway (near the vocal cords and throat) closes off the airway and can eventuaily lead to total obstruction. • Carefully assess the skin for swelling, rash, hives, or signs of the source of the reaction: bite, sting, or con- tact marks. A rapidly spreading rash can be concerning because it may indicate a systemic reaction. Red, hot skin may also indicate a systemic reaction as the blood vessels lose their ability to constrict and blood moves to the extremities. • Vital Signs • Assess baseline vital signs, including pulse, respirations, blood pressure, skin, pupils, and oxygen saturation. Rapid, labored breathing indicates airway obstruction. Rapid respiratory and pulse rates may indicate respiratory distress or systemic shock. • Fast pulses and hypotension are ominous signs, indicating systemic vascular collapse and shock. Skin signs may be an unreliable indicator of hypo perfusion because of rashes and swelling. Emergency medical care for immunological emergency If the patient appears to be having a severe allergic (or anaphylactic) reaction, you should administer basic life support at once and provide prompt transport to the hospital, reassessing vital signs every 5 minutes if the patient's condition is unstable or every 15 minutes if the patient's condition is stable. Place the patient in a position of comfort. Consider the Trendelenburgs position for hypotensive patients and patients showing signs and symptoms of shock. In addition to providing oxygen, you should be prepared to maintain a patent airway or administer cardiopulmonary resuscitation If the allergic reaction was caused by a sting and the stinger is still present, attempt to scrape it away using a hard object, such as a credit card. Placing ice over the injury site has been thought to slow absorption of the toxin and diminish swelling, but ice packs placed directly on the skin may freeze the skin and cause more damage. in some areas, you may be allowed to administer epinephrine or assist the patient with epinephrine administration. Epinephrine • Epinephrine has various properties that cause the blood vessels to constrict, which reverses vasodilation and hypotension; this, in turn, elevates the diastolic pressure and improves coronary blood flow. • Other properties of epinephrine increase cardiac contractility and relieve brocho spasm in the lungs. Because epinephrine has immediate action, it can rapidly reverse the effects of anaphylaxis. • The indications for administering epinephrine include a severe allergic reaction and hypersensitivity to an exposed substance.