OBJECTIVES
advertisement

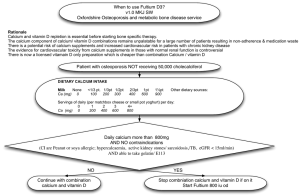
OBJECTIVES Identify the origin,target organs & physiologic effects of parathyroid hormone(including effects on vitamin D metabolism) Describe the regulation of parathyroid hormone secretion & the role of the calcium-sensing receptor. Describe the cell of origin,the target organs,the physiological effects & the regulation of release of calcitonin. Illustrate & discuss the physiological response to hypocalcemia & hypercalcemia. Correlate this knowledge to clinical conditions related to hypo & hypersecretion of parathyroid hormones. CALCIUM METABOLISM - Dietary sources& requirement Dietary sources of calcium: milk, milk products,meat, fish, vegetables, beans, Daily requirements: Adults: 800 mg TO 1 gm. Pregnancy & lactation:1500mg Children: 800-1200mg CALCIUM METABOLISM A total of 1-2 kg of calcium is in the body, 98% of it in the skeleton. Some is bound to proteins, another fraction is bound to anions, usually citrate and phosphate, and the rest is free or ionized calcium. Clinically, the most significant is the ionized fraction. Plasma level 9 – 11 mg %,of this 4mg% non diffusible 6mg%diffusible With plasm proteins (not useful ) 1mg% 5mg% with bocarb Free ionised & phosp This free ionised form (50%of tot.is imp. For Phyiological functios. Calcium is present: 1. Extra cellularly- which can not diffuse into cell as-a). Cell membrane is impermeable to ca. b).Presence of Ca ATPase pump,c).Ca-Na exchange system. 2. Intra cellularly: a. large fraction is stored as in ER. b. Small fraction- free calcium- which brings activity in cells Intra cellular cal. Binding proteins: 1. calmodulin. 2. Calbindin. 3. Troponin. Bone calcium 99% of total calcium is in bones. A fraction of bone calcium can be exchangeable with plasma calcium. It is of 2 types: Readily exchangeable(smallfraction) and Slowly exchageable ( bigger fraction). The exchangeable bone calcium is under the influence of PTH, 1,25 DHCC. Calcium- Functions Required for formation of bones& teeth. muscle contraction Nerve excitation, membrane excitation NM & Synaptic transmission. Glandular secretion Blood coagulation intracellular messenger systems cardiac repolarization. Milk formation. Entry & exit of calcium Amount ingested = excreted in stool+ urine CALCIUM PHYSIOLOGY: BLOOD CALCIUM CALCIUM FLUX INTO AND OUT OF BLOOD “IN” FACTORS: INTESTINAL ABSORPTION, BONE RESORPTION Renal reabsorption “OUT” FACTORS: RENAL EXCRETION, BONE FORMATION (Ca INCORPATION INTO BONE) CALCIUM PHYSIOLOGY: BLOOD CALCIUM BLOOD CALCIUM IS TIGHTLY REGULATED PRINCIPLE ORGAN SYSTEMS GUT, BONE, KIDNEYS HORMONES PARATHYROID HORMONE (PTH), 1,25 DHCC(VITAMIN D) & Calcitonin INTEGRATED PHYSIOLOGY OF ORGAN SYSTEMS AND HORMONES MAINTAIN BLOOD CALCIUM Hormones of calcium metabolism PARATHYROID HORMONE (PTH), 1,25 DHCC(VITAMIN D) Calcitonin Parathyroid glands Were discovered in 1880 by Sandstorm of Sweden Parathyroid Hormone Produced by Parathyroid Chief cells Secreted in response to low iCa++ Stimulates renal conversion of 25-(OH)D3 to 1,25-(OH)2D which increases intestinal Ca++ absorption Directly stimulates renal Ca++ absorption and PO43- excretion Stimulates osteoclastic resorption of bone PARATHYROID HORMONE (PTH) PHYSIOLOGY PTH FUNCTIONS TO PRESERVE NORMAL BLOOD CALCIUM (AND PHOSPHATE) PTH STIMULATES BONE RESORPTION AND, THUS, INCREASES BLOOD CALCIUM PTH STIMULATES RENAL TUBULAR REABSORPTION OF CALCIUM, AND THUS, INCREASES BLOOD CALCIUM PTH STIMULATES RENAL 1a-HYDROXYLATION OF 25(OH)VITAMIN D, THUS INDIRECTLY STIMULATING INTESTINAL ABSORPTION OF CALCIUM PTH PHYSIOLOGY PTH SECRETION IS INCREASED IN RESPONSE TO FALLING CALCIUM LEVEL, TO HELP KEEP CALCIUM NORMAL BY THE ABOVE MECHANISMS RISING CALCIUM FEEDS BACK TO THE PARATHYROIDS TO SUPPRESS PTH SECRETION IN A CLASSIC ENDOCRINE FEEDBACK LOOP THIS LOOP IS MUCH LIKE OTHER ENDOCRINE FEEDBACK LOOPS YOU’RE FAMILIAR WITH SUCH AS GLUCOSE AND INSULIN, THYROID HORMONE AND TSH, ETC. CALCIUM, PTH, AND VITAMIN D FEEDBACK LOOPS BONE RESORPTION URINARY LOSS SUPPRESS PTH 1,25(OH)2 D PRODUCTION RISING BLOOD Ca NORMAL BLOOD Ca FALLING BLOOD Ca BONE RESORPTION URINARY LOSS 1,25(OH)2 D PRODUCTION STIMULATE PTH CALCIUM FEEDBACK TO REGULATE PTH SECRETION CALCIUM-SENSING RECEPTOR IN THE PARATHYROIDS 7-TRANSMEMBRANE SPANNING PROTEIN RECEPTOR THAT BINDS CALCIUM EXTRACELLULARLY, AND IS COUPLED TO SIGNALLING PATHWAYS VIA G-PROTEINS THE Ca-SENSING RECEPTOR IS ALSO PRESENT IN THE KIDNEYS, AND A VARIETY OF OTHER TISSUES MECHANISM OF CALCIUM FEEDBACK TO REGULATION OF PTH SECRETION IS MEDIATED VIA THE Ca-SENSING RECEPTOR INCREASING AMBIENT CALCIUM IS SENSED BY RECEPTOR AND SUPPRESSES PTH SECRETION FALLING AMBIENT CALCIUM IS SENSED BY RECEPTOR AND STIMULATES PTH SECRETION CALCIUM SENSING RECEPTOR: CLINICOPATHOLOGIC CORRELATES INACTIVATING MUTATIONS RIGHT-SHIFT THE SETPOINT FOR PTH SECRETION, SO THAT IT TAKES HIGHER CALCIUM TO SUPPRESS PTH SECRETION IN THE HETEROZYGOUS STATE, IT TAKES HIGHER AMBIENT CALCIUM TO SUPPRESS PTH SECRETION. PATIENTS WITH THIS MUTATION HAVE HYPERCALCEMIA, AND RELATIVELY LOW URINE CALCIUM LOSSES. THIS IS REFERRED TO AS FAMILIAL BENIGN HYPOCALCIURIC HYPERCALCEMIA (FBHH). IT IS A CONDITION FREE OF THE PROBLEMS USUALLY ASSOCIATED WITH HYPERCALCEMIA. IN THE HOMOZYGOUS STATE, IT IS LETHAL IN INFANCY AS A RESULT OF VERY SEVERE HYPERCALCEMIA. PTH RECEPTOR PTH RECEPTORS ARE TRANSMEMBRANE PROTEIN RECEPTORS FOUND IN A VARIETY OF TISSUES (BONE, KIDNEY, OTHERS). PTH RECEPTORS ARE COUPLED TO SECOND MESSENGER SYSTEMS VIA STIMULATORY G PROEINS (Gs). BINDING PTH TO THE RECEPTOR CAUSES GDP TO DISSOCIATE FROM Gs AND GTP TO BIND. THE SIGNAL IS THEN TRANSMITTED TO A VARIETY OF SECOND MESSENGER SYSTEMS, RESULTING IN PRODUCTION OF CYCLIC AMP (cAMP), INOSITOL TRIPHOSPHATE, DIACYLGLYCEROL, AND OTHERS. THE PTH RECEPTOR ALSO BINDS THE PARATHYROID HORMONE RELATED PROTEIN (PTHrP) WITH EQUAL AFFINITY TO PTH. FOR THIS REASON, THE RECEPTOR IS USUALLY REFERRED TO AS THE PTH/PTHrP RECEPTOR. PTH RECEPTOR: CLINICOPATHOLOGIC CORRELATES THERE IS A FAMILY OF DISEASES KNOWN AS PSEUDOHYPOPARATHYROIDISM. CLINICAL MANIFESTATIONS INCLUDE HYPOCALCEMIA THUS MIMICKING HYPOPARATHYROIDISM. HOWEVER, AFFECTED INDIVIDUALS ARE RESISTANT TO PTH, NOT DEFICIENT IN PTH. PTH LEVELS ARE ELEVATED IN THESE PATIENTS. THE MOLECULAR DEFECTS IN PSEUDOHYPOPARATHYROIDISM ARE NOT ALL CHARACTERIZED, ALTHOUGH IN SOME CASES ARE WELL CHARACTERIZED. A CLASSIC EXAMPLE IS A MUTATION IN ONE OF THE SUBUNITS OF Gs, SO THAT SIGNAL TRANSDUCTION UPON PTH BINDING THE RECEPTOR IS NOT TRANSMITTED TO THE SECOND MESSENGER PATHWAYS CONSIDER IN RELATION TO DISEASES OF INSULIN RESISTANCE, VITAMIN D RESISTANCE, THYROID HORMONE RESISTANCE, ETC. CALCIUM HOMEOSTASIS DIETARY CALCIUM THE ONLY “IN” BONE DIETARY HABITS, SUPPLEMENTS ORGAN, ENDOCRINE BLOOD CALCIUM INTESTINAL ABSORPTION ORGAN PHYSIOLOGY KIDNEYS ENDOCRINE PHYSIOLOGY ORGAN PHYS. ENDOCRINE PHYS. URINE THE PRINCIPLE “OUT” VITAMIN D PHYSIOLOGY VITAMIN D IS A HORMONE BY CLASSIC CRITERIA: MADE IN ONE PLACE (OR SEQUENTIALLY SEVERAL PLACES!), AND ACTING IN OTHER PLACES. THIS DISTINGUISHES IT FROM OTHER “CLASSIC” VITAMINS, SUCH AS VITAMIN C, B VITAMINS, ETC., WHICH ACT AS COFACTORS IN BIOCHEMICAL REACTIONS. Vitamin D Sources Metabolism Food – Vitamin D2 UV light mediated cholesterol metabolism – D3 D2 and D3 are converted to 25(OH)-D by the liver 25(OH)-D is converted to 1,25(OH)2-D by the Kidney Function Stimulation of Osteoblasts Increases GI absorption of dietary Ca++ VITAMIN D SYNTHESIS THE PRECURSOR FOR VITAMIN D SYNTHESIS IS A STEROL IN THE CHOLESTEROL BIOSYNTHETIC PATHWAY, 7-DEHYDROCHOLESTEROL. IN THE SKIN, ULTRAVIOLET LIGHT TRANSFORMS 7-DEHYDROCHOLESTEROL TO VITAMIN D3 ROLE OF SUNLIGHT IN VITAMIN D ADEQUACY VITAMIN D SYNTHESIS VITAMIN D3 CIRCULATES TO THE LIVER, WHERE THE ENZYME 25-HYDROXYLASE HYDROXYLATES IT TO 25HYDROXY VITAMIN D (25(OH)VITAMIN D) 25-HYDROXYLASE FUNCTIONS CONSTITUTIVELY WITHOUT INPUT FROM BLOOD CALCIUM STATUS OR PTH 25(OH)VITAMIN D IS THE BEST SCREENING TEST FOR VITAMIN D ADEQUACY VITAMIN D SYNSTHESIS 25(OH)VITAMIN D CIRCULATES TO THE KIDNEYS, WHERE THE ENZYME RENAL 1a-HYDROXYLASE HYDROXYLATES IT TO 1,25(OH)2 VITAMIN D THIS IS THE ACTIVE METABOLITE OF VITAMIN D. 1,25(OH)2 VITAMIN D MEDIATES THE PHYSIOLOGIC ROLES OF VITAMIN D. RENAL 1a-HYDROXYLASE IS REGULATED BY PTH WHICH STIMULATES ITS ACTIVITY. PTH IS THE PRINCIPLE PHYSIOLOGIC REGULATOR, ALTHOUGH CALCIUM CAN AFFECT THE ACTIVITY. VITAMIN D SYNTHESIS SKIN LIVER 7-DEHYDROCHOLESTEROL h VITAMIN D3 VITAMIN D3 KIDNEY 25(OH)VITAMIN D 25-HYDROXYLASE 25(OH)VITAMIN D 1a-HYDROXYLASE 1,25(OH)2 VITAMIN D (ACTIVE METABOLITE) TISSUE-SPECIFIC VITAMIN D RESPONSES VITAMIN D THE BODY CAN SUPPLY ITS OWN VITAMIN D VIA THE SYNTHETIC PATHWAYS SHOWN ABOVE. ALTERNATIVELY, VITAMIN D MAY BE SUPPLIED BY VITAMIN D - ENRICHED FOODS. THE CLASSIC EXAMPLES ARE MILK AND MULTIPLE VITAMINS. VITAMIN D MECHANISM OF ACTION: VITAMIN D RECEPTOR BIOLOGICAL EVOLUTION IS VERY CONSERVATIVE. VITAMIN D SHARES MANY SIMILARITIES WITH STEROID HORMONES. IT IS NOT SURPRISING, THEREFORE, THAT THE VITAMIN D RECEPTOR SHARES AN EVOLUTIONARY RELATIONSHIP WITH RECEPTORS FOR STEROID HORMONES, THYROID HORMONE, RETINOIDS, AND MANY ORPHAN RECEPTORS (WITH NO KNOWN LIGAND). Bind with intrcellular receptors – Gene expression in target cells VITAMIN D REPCEPTOR: TRANSCRIPTIONAL REGULATION THE SUPERGENE FAMILY OF NUCLEAR RECEPTORS THAT INCLUDES THE VITAMIN D RECEPTOR ALSO INCLUDES RECEPTORS FOR CORTISOL, ESTROGEN, TESTOSTERONE, THYROID HORMONE, ALDOSTERONE, RETINOIC ACID, AND OTHERS. MANY RECEPTORS IN THIS FAMILY HAVE NO KNOWN LIGAND, AND MAY FUNCTION VIA ALTERATIONS IN PHOSPHORYLATION STATE, AND/OR ??. VITAMIN D MECHANISM OF ACTION VIT D / VDR RNA POL 5’ UNTRANSLATED REGION VITAMIN D RESPONSIVE GENE TRANSCRIPTION START SITE IN THE NUCLEUS ACTIONS OF 1,25 DHCC GUT To help calcium absorption. STIMULATE TRANSEPITHELIAL TRANSPORT OF CALCIUM AND PHOSPHATE IN THE SMALL INTESTINE (PRINCIPALLY DUODENUM). Induce synthesis of calcium binding proteins,calbinding,&calcium dependantATPase. BONE STIMULATE TERMINAL DIFFERENTIATION OF OSTEOCLASTS STIMULATE OSTEOBLASTS TO STIMULATE OSTEOCLASTS TO MOBILIZE CALCIUM = BONE RESORPTION KIDNEYS: INCREASE RENAL REABSORPTION OF CALCIUM&PHOSPAHTES PARATHYROID INHIBIT TRANSCRIPTION OF THE PTH GENE (FEEDBACK REGULATION) Calcitonin Produced by Parafollicular C cells of Thyroid in response to increased iCa++ Actions Inhibit osteoclastic resorption of bone Increase renal Ca++ and PO43- excretion Non-essential hormone. Patients with total thyroidectomy maintain normal Ca++ concentrations Useful in monitoring treatment of Medullary Thyroid cancer Used in treatment of Pagets’, Osteoporosis ORGAN PHYSIOLOGY AND CALCIUM METABOLISM THERE ARE THREE PRICIPLE TISSUES THAT FUNCTION PROMINENTLY IN CALCIUM HOMEOSTATIS. DISORDERS OF THESE TISSUES, OR OF THE CALCIOTROPIC FACTORS THAT AFFECT THEIR FUNCTION MAY RESULT IN DISORDERS OF CALCIUM METABOLISM INTESTINES KIDNEYS BONE ORGAN PHYSIOLOGY AND CALCIUM METABOLISM IT HELPS TO THINK IN TERMS OF THE “IN” AND “OUT” FACTORS WE DISCUSSED AT THE BEGINNING OF THIS SECTION. THEREFORE, THE ORGAN INFLUENCES OF INTESTINAL ABSORPTION, BONE RESORPTION AND FORMATION, AND RENAL EXCRETION CONTRIBUTE TO MAINTAINANCE OF NORMAL BLOOD CALCIUM. INCORPORATE YOUR UNDERSTANDING OF THE ABOVE HORMONES, AND NORMAL CALCIUM METABOLISM ASSUMES THE LOGIC CHARACTERISIC OF THE STUDY OF ENDOCRINOLOGY. DISORDERS IN ORGAN PHYSIOLOGY AND/OR HORMONE FUNCTION MAY RESULT IN DISEASE. GI PHYSIOLOGY NORMAL INTESTINAL FUNCTION AND NORMAL RESPONSE TO VITAMIN D ARE REQUIRED FOR NORMAL CALCIUM ABSORPTION. GI DYSFUNCTION: SHORT BOWEL, MALABSORPTION SYNDROMES, INFLAMMATORY BOWEL SYNDROMES AVAILABILITY AND FUNCTION OF VITAMIN D (DIETARY AND/OR ENDOGENOUS) DIETARY CALCIUM INTAKE DIETARY PHOSPHATE INHIBITS Ca ABSORPTION RENAL PHYSIOLOGY RENAL FUNCTION RESPONSE TO PTH 1,25(OH)2D PRODUCTION TUBULAR RESPONSE (Ca REABSORPTION) NORMAL FUNCTION IN 1,25(OH)2D SYNTHESIS 1,25(OH)2D SUPPLEMENTATION IN RENAL INSUFFICIENCY/FAILURE NORMAL TUBULAR PHYSIOLOGY GENETIC RENAL CALCIUM LEAK HYPERCALCIURIA, WITH SECONDARY HYPERPARATHYROIDISM BONE PHYSIOLOGY BONE IS A RESERVOIR OF CALCIUM, CALCIUM EN MASSE BEING REQUIRED TO MAKE AND MAINTAIN THE SKELETON. TO BE AN EFFECTIVE RESERVOIR FOR THE MAINTAINANCE OF NORMAL BLOOD CALCIUM, CALCIUM MUST BE ABLE TO BE INCORPORATED INTO, AND LIBERATED FROM, BONE ON SHORT NOTICE. BONE PHYSIOLOGY, cont. BONE TURNOVER: A COUPLED PROCESS OF BONE FORMATION AND BONE RESORPTION (BREAK DOWN) TAKES PLACE THROUGHOUT LIFE SHIFT TOWARD FORMATION OR RESORPTION REMOVES Ca FROM BLOOD OR PUTS Ca INTO BLOOD, RESPECTIVELY, AND CORRESPOND-INGLY AFFECTS BONE MASS. BONE PHYSIOLOGY, cont.: BONE TURNOVER SKELETAL MASS IN THE HUMAN REACHES A PEAK AT ABOUT AGE 30 PRIOR TO THAT, AS SKELETAL MASS IS INCREASING, BONE FORMATION EXCEEDS BONE RESORPTION. AT PEAK BONE MASS, THE TWO PROCESSES ARE EXACTLY MATCHED AFTER THE AGE OF PEAK BONE MASS, SKELETAL MASS IS LOST FOR THE REST OF LIFE BONE PHYSIOLOGY, cont. BONE FORMATION IS MEDIATED BY OSTEOBLASTS BONE RESORPTION IS MEDIATED BY OSTEOCLASTS PNEMONIC: OSTEOBLASTS BUILD; OSTEOCLASTS, WELL, THEY DON’T MEASUREMENT OF BONE TURNOVER THE COUPLED PROCESS OF BONE TURNOVER CAN BE MEASURED BY: MARKERS OF OSTEOBLAST METABOLISM SERUM BONE-SPECIFIC ALKALINE PHOSPHATASE SERUM OSTEOCALCIN MARKERS OF OSTEOCLAST METABOLISM URINE PRODUCTS OF BONE COLLAGEN BREAKDOWN HYDROXYPROLINE N-TELOPEPTIDES PYRIDINIUM CROSSLINKS BONE PHYSIOLOGY, cont. HORMONAL CHAIN OF COMMAND: NOTE THAT OSTEOCLASTS RESORB BONE, AND THAT 1,25(OH)2D AND PTH STIMULATE BONE RESORPTION. HOWEVER, OSTEOCLASTS HAVE RECEPTORS FOR NEITHER PTH NOR 1,25(OH)2D PTH AND 1,25(OH)2D RECEPTORS ARE EXPRESSED ON OSTEOBLASTS. THE OSTEOBLASTS, IN RESPONSE TO THESE HORMONES, SEND A PARACRINE SIGNAL TO OSTEOCLASTS TO TERMINALLY DIFFERENTIATE (VIT. D INFLUENCE) AND RESORB BONE (PTH INFLUENCE). BONE PHYSIOLOGY, cont. WHEN THE COUPLED PROCESS OF BONE TURNOVER (FORMATION AND RESORPTION) IS SHIFTED IN FAVOR OF RESORPTION, THERE IS RELATIVE OR NET BONE LOSS. THIS OCCURS IN A VARIETY OF CONDITIONS: age menopause in women or hypogonadism in men glucocorticoid therapy hyperparathyroidism (primary of secondary) defects in organ physiology (GI, RENAL, BONE) others (medications, genes, comorbid conditions, etc.) BONE PHYSIOLOGY, cont. IN A BROAD SENSE, FRACTURE RISK IS INVERSELY PROPORTIONAL TO BONE MASS accelerated bone loss increases fracture risk menopause chronic and/or high dose glucocorticoid therapy others failure to reach normal peak bone mass means lower bone mass per age later in life, and therefore increases fracture risk soda pop doesn’t provide calcium or vitamin D!! BONE MASS AS A FUNCTION OF AGE; PERTURBATIONS PEAK BONE MASS NORMAL FAILURE TO REACH PEAK ACCELERATED LOSS BONE MASS THEORETICAL FRACTURE THRESHOLD AGE APPLIED ASPECTS Hypoparathyroidism& Hypocalcemia,Tetany. Rickets Osteomalacia Osteoporosis Hyperparathyroidism. Hypocalcemia Decreased PTH Resistance to PTH Genetic disorders Bisphosphonates Vitamin D abnormalities Surgery Hypomagnesemia Idiopathic Vitamin D deficiency Rickets (VDR or Renal hyroxylase abnormalities) Binding of Calcium Hyperphosphate states (Crush injury, Tumor lysis, etc.) Blood Transfusion (Citrate) Hypoparathyroidism Truehypoparathyroidism:1. Post operative during thyroidectomy 2. Idiopathic. Here Decreased secretion of PTH. Pseudohypoparathyroidism: PTH secretion is normal but non responsiveness of PTH receptors of target tissues. Hypoparathyroidism leads to Hypocalcemia Hypocalcemia Causes: Hypoparathyroidism , Alkalosis. Decreased plasma calcium <4-8mg% and ionised calcium<3mg%. This leads to clinical condition = TETANY TETANY: 1. Latent tetany: (Sub clinical) –Assessed by – Trausseau’s sign & Chvostek’s sign. 2. Manifest Tetany:Carpal & pedal(rare)spasm,Laryngeal stridorasphyxia,Visceral features-bronchospasm,etc HYPOCALCEMIA: SIGNS AND SYMPTOMS NEUROMUSCULAR: CNS: IRRITABILITY, SEIZURES, PERSONALITY CHANGE, INVOLUNTARY MUSCLE CONTRACTION (TETANY), 7TH CRANIAL NERVE EXCITABILITY (CHVOSTEK’S SIGN), NUMBNESS AND TINGLING IN FACE, HANDS, AND FEET, TROUSSEAU’S SIGN IMPAIRED COGNITION CARDIOVASCULAR: QT PROLONGATION ON ECG, IN THE EXTREME, ELECTROMECHANICAL DISSOCIATION MAY OCCUR HYPOCALCEMIA: SIGNS AND SYMPTOMS AS WAS NOTED ABOVE FOR HYPERCALCEMIA, THERE IS NO FIXED LEVEL OF BLOOD CALCIUM AT WHICH SIGNS AND/OR SYMPTOMS DEVELOP. THIS VARIES FROM PATIENT TO PATIENT, AND MAY BE INFLUENCED BY COMORBID CONDITIONS. CAUSES OF HYPOCALCEMIA HYPOPARATHYROIDISM HYPOVITAMINOSIS D POSTSURGICAL (MOST COMMON) AUTOIMMUNE PSEUDOHYPOPARATHYROIDISM (PTH RESISTANCE) IDIOPATHIC DIETARY DEFICIENCY RICKETS, OSTEOMALACIA ORGAN DYSFUNCTION GI MALABSORPTION, RENAL LOSS ENDOCRINE RESPONSE TO NON-HYPOPARATHYROID HYPOCALCEMIA SECONDARY HYPERPARATHYROIDISM (2o HPT) HYPOCALCEMIA: HYPOPARATHYROIDISM POSTSURGICAL MOST COMMON CAUSE OF HYPOPARATHYROIDISM AUTOIMMUNE MAY CLUSTER WITH OTHER AUTOIMMUNE ENDOCRINE DISEASES, INCLUDING IDDM, AUTOIMMUNE THYROID DISEASE, ADDISON’S, ETC. THIS IS RATHER UNCOMMON. HYPOPARATHYROIDISM: TREATMENT GOAL: MAINTAIN ADEQUATE BLOOD CALCIUM WITHOUT CAUSING SIDE EFFECTS PTH IS NOT AVAILABLE CLINICALLY FOR REPLACEMENT THERAPY TREATMENT CENTERS ON THE USE OF VITAMIN D AND CALCIUM SUPPLEMENTATION VITAMIN D AND CALCIUM CAN MAINTAIN BLOOD CALCIUM VIA ENHANCED GI ABSORPTION ABSENCE OF PTH ALLOWS UNRESTRICTED URINARY LOSS HYPOPARATHYROIDISM: TREATMENT SUMMARY VITAMIN D AND CALCIUM SUPPLEMENTS TO MAINTAIN BLOOD CALCIUM AT LOW END OF NORMAL PREVENT SYMPTOMS OF HYPOCALCEMIA MINIMIZE URINARY CALCIUM LOSSES USUALLY USE PRESCRIPTION STRENGTH VITAMIN D HYPOCALCEMIA: HYPOVITAMINOSIS D THIS CATEGORY INCLUDES A NUMBER OF CONDITIONS RELATED TO VITAMIN D AVAILABILITY, METABOLISM, OR FUNCTION INADEQUATE DIETARY SUPPLY INADEQUATE EXPOSURE TO SUNLIGHT DEFECTS IN VITAMIN D SYNTHESIS DEFECTS IN VITAMIN D RECEPTOR DEFECTIVE VITAMIN D FUNCTION CLINICAL SYNDROMES BROADLY CATEGORIZED AS RICKETS AND OSTEOMALACIA. DIMINISHED GI ABSORPTION OF Ca TENDENCY TOWARD HYPOCALCEMIA SECONDARY HYPERPARATHYROIDISM NON-PARATHYROID HYPOCALCEMIA: SECONDARY HYPERPARATHYROIDISM IN HYPOVITAMINOSIS D (RICKETS AND OSTEOMALACIA), LOW LEVELS OF, OR DEFECTIVE FUNCTION OF, VITAMIN D CAUSE TENDENCY TOWARD HYPOCALCEMIA. THE PARATHYROIDS RESPOND APPROPRIATELY BY INCREASING PTH SECRETION TO MAINTAIN NORMAL BLOOD CALCIUM. THIS IS REFERRED TO AS SECONDARY HYPERPARATHYROIDISM: ELEVATED PTH IN RESPONSE TO (SECONDARY TO) SOME NON-PARATHYROID PROBLEM RICKETS In children. Mineralization of organic bone bone matrix is defective. Causes & types: 1. Vit.D deficiency rickets-a. Nutritionalb. Deficient synthesis due to lack of exposure to sun light(uv rays). 2. VitD resistant rickets: non forming of 1,25DHCC OR no response to it( receptor level) Features of Rickets Bony defects:Craniotabes(areas in membranous skull yeilding to pressure), Widening of wrists, Chest deformities, Rickety rosary( beading of costochondral junctions), Bowing of legs/knock knee, Kyphosis. General: delayed mile stones. Biochemical:Decreased plasma cal, CaXPO4<60( normal 60),decreased 1,25DHCC Tetany : if sever hypocalcemia Rickets RICKETS AND OSTEOMALACIA(malacia=softening) DISEASES OF DEFECTIVE BONE MINERALIZATION THESE DISEASES ARE PATHOPHYSIOLOGICALLY RELATED, AND DIFFER MAINLY IN THE AGE AT WHICH THEY BECOME MANIFEST RICKETS IS A DISEASE OF CHILDHOOD OSTEOMALACIA IS A DISEASE OF ADULTHOOD WIDE RANGING CATEGORY OF DISEASE DISORDERS OF VITAMIN D PHOSPHATE DEFICIENCY CHRONIC RENAL FAILURE (ALSO RENAL OSTEODYSTROPHY) PRIMARY DISORDERS OF BONE METABOLISM RICKETS AND OSTEOMALACIA: CLINICAL MANIFESTATIONS RICKETS MAY RESULT IN CHARACTERISTIC BONY DEFORMITIES IN CHILDREN RICKETS USUALLY IS ASSOCIATED WITH SHORT STATURE OSTEOMALACIA IN ADULTS GENERALLY DOES NOT CAUSE BONY DEFORMITIES OSTEOMALACIA (ONSET IN ADULTHOOD) DOES NOT CAUSE SHORT STATURE PATIENTS MAY SUFFER BONE PAIN (NOT SEEN IN OSTEOPOROSIS UNLESS THERE IS A FRACTURE) FRACTURE RISK IS INCREASED RICKETS AND OSTEOMALACIA: CAUSES NUTRITIONAL DEFICIENCY OF VITAMIN D AND/OR INADEQUATE SUNLIGHT EXPOSURE: EASILY TREATED WITH DIETARY SUPPLEMENTATION FORTIFIED MILK - PROVIDES VITAMIN D AND CALCIUM MULTIPLE VITAMIN - PROVIDES VITAMIN D ONLY EITHER WAY, MUST ASSURE ADEQUATE CALCIUM WITH THE VITAMIN D DEFECTIVE RENAL 1a-HYDROXYLATION OF 25(OH) VIT. D AUTOSOMAL RECESSIVE CHARACTERIZED BY HYPOCALCEMIA, HYPOPHOSPHATEMIA, SECONDARY HYPERPARATHYROIDISM, LOW 1,25(OH)2D, AND INCREASED ALKALINE PHOSPHATASE TREATMENT IS BY GIVING 1,25(OH)2D AND CALCIUM RICKETS AND OSTEOMALACIA: CAUSES, cont. TISSUE RESISTANCE TO 1,25(OH)2D AUTOSOMAL RECESSIVE, OR ACQUIRED DEFECT IN NUCLEAR RECEPTOR FOR VITAMIN D DEFECTIVE SYNTHESIS OF RECEPTOR DEFECTIVE AFFINITY OF RECEPTOR FOR 1,25(OH)2D DEFECTIVE ABILITY OF 1,25(OH)2D/VITAMIN D RECEPTOR COMPLEX TO INTERACT WITH DNA OR ACTIVATE TRANSCRIPTIONAL MACHINERY PROPERLY TREATMENT IS WITH 1,25(OH)2D AND CALCIUM RESPONSE TO THERAPY IS VARIABLE GIVEN DIVERSITY OF MOLECULAR DEFECTS (ABOVE) RICKETS AND OSTEOMALACIA: CAUSES, cont. ANITCONVULSANT-INDUCED OSTEOMALACIA: PATIENTS TREATED CHRONICALLY WITH DIPHENYLHYDANTOIN (PHENYTOIN, DILANTIN©) OR PHENOBARBITAL FOR SEIZURE DISORDERS ARE AT RISK FOR ANTICONVULSANT-INDUCED OSTEOMALACIA THESE DRUGS ALTER AND ACCELERATE HEPATIC METABOLISM OF VITAMIN D, AND THIS IS THOUGHT TO PLAY A MAJOR ROLE IN THIS DISORDER ASSURANCE OF ADEQUATE VITAMIN D INTAKE IS ENCOURAGED IN THESE PATIENTS NEWER ANTICONVULSANTS, SUCH AS VALPROIC ACID, CARBAMAZEPINE, GABAPENTIN, ETC. HAVE NOT BEEN IMPLICATED AS OF YET Osteoporosis Primary = Senile osteoporosis and more commonly post menopausal. Secondary: due to excess of glucocorticoids, hyperparathyroidism etc. Mainly loss of bone matrix i.e loss of collgin fibers with some loss of calcium salt. Osteoporosis Symptoms of Osteoporosis There are no symptoms in the early stages of the disease. Symptoms occurring late in the disease include: Joint pain and tenderness Swelling Warmth over the affected joint HYPERCALCEMIA HYPERCALCEMIA IS THE STATE OF BLOOD CALCIUM CONCENTRATION ABOVE THE NORMAL RANGE RELATE TO ORGAN PHYSIOLOGY AND ENDOCRINE PHYSIOLOGY DISCUSSED ABOVE: “IN” AND “OUT” FACTORS GI, RENAL, BONE PTH, VITAMIN D TO MUCH CALCIUM ENTERING BLOOD AND/OR TOO LITTLE LEAVING BLOOD Hypercalcemia Hyperparathyroidism Malignancy Overproduction of 1,25 (OH)2D Drug-Induced Humoral Hypercalcemia PTHrP (Lung Cancer) Osteoclastic activity (Myeloma, Lymphoma) Granulomatous Diseases Primary, Secondary, Tertiary MEN Syndromes Thiazides Lithium Milk-Alkali Vitamin A, D Renal failure Hypercalcemia Signs & Symptoms Medical Treatment Bones (Osteitis fibrosa cystica, osteoporosis, rickets) Stones (Renal stones) Groans (Constipation, peptic ulcer) Moans (Lethargy, depression, confusion) SERM’s (Evista) Bisphosphonates (Pamidronate) Calcitonin (for severe cases) Saline diuresis Glucocorticoids (for malignant/granulomatous diseases) Avoid thiazide diuretics Surgical Treatment Single vs. Double adenoma – simple excision Multiple Gland hyperplasia – total parathyroid with autotransplant vs. 3½ gland excision Primary Hyperparathyroidism Diagnosis Signs & Symptoms Elevated serum calcium Elevated PTH Etiology Solitary Adenoma (80-85%) Double Adenomas (2-4%) Muliple Gland Hyperplasia (10-30%) Parathyroid Carcinoma (0.5%) MEN syndromes (10% of MGH have MEN 1) Multiple Endocrine Neoplasia MEN 1 MEN 2a Pituitary adenoma Pancreatic endocrine tumor Parathyroid neoplasia (90%) Medullary thyroid cancer (100%) Pheochromocytoma (50%) Parathyroid neoplasia (10-40%) MEN 2b Medullary thyroid cancer (100%) Pheochromocytoma (50%) Neuromas (100%) Parathyroidectomy 1990 NIH Guidelines Serum Ca++ > 12 mg/dl Hypercalciuria > 400 mg/day Classic symptoms Nephrolithiasis Osteitis fibrosa cystica Neuromuscular disease Cortical bone loss with DEXA Z score < -2 Reduced creatinine clearance Age < 50 Other considerations Vertebral osteopenia Vitamin D deficency Perimenopause Preoperative Localization Thallium / Pertechnetate Technetium 99m Sestamibi Based on subtraction of Tc 99 which concentrates only in thyroid from background Thallium which is absorbed by thyroid and parathyroid Moderate sensitivity and specificity Thyroid pathology reduces effectiveness Absorbed by thyroid and abnormal parathyroid Early washout from thyroid leaves residual parathyroid signals in later images Higher sensitivity and specificity Single Photon Emission Computed Tomography Creates a three dimensional representation to allow for ectopic localization Not commonly used HYPERCALCEMIA: SIGNS AND SYMPTOMS SIGNS AND SYMPTOMS DEPEND ON THE DEGREE OF HYPERCALCEMIA AND COMORBID CONDITIONS THERE IS NO ABSOLUTE VALUE OF BLOOD CALCIUM AT WHICH SYMPTOMS DEVELOP. LEVEL OF BLOOD CALCIUM AT WHICH SYMPTOMS DEVELOP VARY FROM PATIENT TO PATIENT. HYPERCALCEMIA: SIGNS AND SYMPTOMS CNS: altered MS, including lethargy, depression, decreased alertness, confusion, obtundation, and coma GI: anorexia, constipation, nausea, and vomiting RENAL: diuresis, impaired concentrating ability, dehydration. Hypercalciuria is a risk for kidney stones. SKELETAL: most causes of hypercalcemia are associated with increased bone resorption, and thus, fracture risk CARDIOVASCULAR: cause/exacerbate HTN, shortened QT interval CAUSES OF HYPERCALCEMIA HORMONAL NON-HORMONAL PRIMARY HYPERPARATHYROIDISM HYPERVITAMINOSIS D PARANEOPLASTIC (e.g., PTHrP, cytokines) RENAL FAILURE MILK-ALKALI SYNDROME DRUGS THIAZIDES, LITHIUM, OTHERS PRIMARY HYPERPARATHYROIDISM PRIMARY HYPERPARATHYROIDISM (1o HPT) is the most common cause of hypercalcemia in the healthy outpatient setting RESULTS FROM AN ADENOMA, MULTIPLE ADENOMAS, OR HYPERPLASIA OF THE PARATHYROIDS. MALIGNANCY IS FORTUNATELY VERY RARE. THE DEFECT LIES WITH THE PARATHYROID TISSUE. COMPARE SECONDARY HYPERPARA-THYROIDISM (2o HPT), BELOW PRIMARY HYPERPARATHYROIDISM 1o HPT is characterized by hypercalcemia PTH above the normal range hypercalciuria increased risk of fractures increased risk of kidney stones seldom causes extreme hypercalcemia unless confounded by renal failure, dehydration, etc. QESTIONS 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. How much calcium we have in our body? Name the dietary sources of calcium. What is daily dietary requirements? In which forms calcium is present in our body? Mention the functions of calcium. Name 3 organs related to cal.metabolism Name 3 hormones related to it. Name other hormones influencing metabolism Site of synthesis& mechanism of action of PTH Actions of PTH QESTIONS 11. Describe formation of 1,25DHCC 12. Which factors regulate synthesis of it. 13. Mechanism of action of 1,25DHCC 14. Actions of 1,25DHCC. 15. Describe the hormonal regulation of blood calcium. 16. Describe TETANY. 17. Describe RICKTES. 18. Describe OSTEOMALACIA. 19. Describe OSTEOPOROSIS.