Parasitology 7th lecture
advertisement
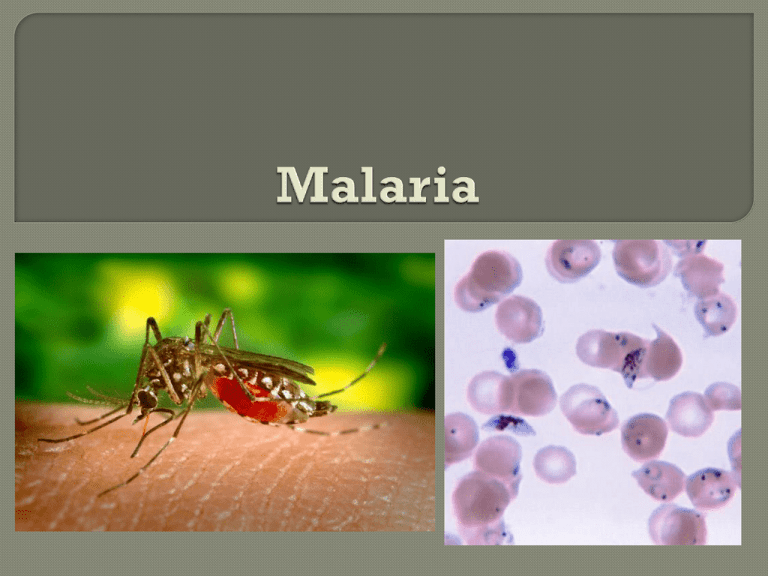
Malaria is a vector-borne infectious disease caused by protozoan parasites. It is widespread in tropical and subtropical regions, including parts of the Americas, Asia, and Africa. Each year, there are approximately 350–500 million cases of malaria, killing between one and three million people, the majority of whom are young children in Sub-Saharan Africa. Ninety percent of malaria-related deaths occur in Sub-Saharan Africa. Malaria is one of the most common infectious diseases and an enormous public health problem. The disease is caused by protozoan parasites of the genus Plasmodium. 4 species of the plasmodium parasite can infect humans; the most serious forms of the disease are caused by Plasmodium falciparum. Malaria caused by Plasmodium vivax, Plasmodium ovale and Plasmodium malariae causes milder disease in humans that is not generally fatal. People get malaria by being bitten by an infective female Anopheles mosquito. Only Anopheles mosquitoes can transmit malaria, and they must have been infected through a previous blood meal taken on an infected person. Malaria is transmitted primarily by the bite of infected anopheline mosquitoes. It can also be transmitted by inoculation of infected blood. Anophelines feed at night and their breeding sites are primarily in rural areas. The greatest risk of malaria is therefore from dusk to dawn in rural areas. In many malaria-endemic areas, there is little or no risk in urban areas. In the late 1950s and early 1960s, it was thought that malaria could be eradicated through the widespread use of insecticides such as DDT and by treatment of cases with chloroquine. Eradication is no longer thought possible, however, because of the development of drug resistance by both the mosquito and the parasite, and because of deteriorating social and economic conditions in many malaria-endemic countries. These changes have resulted in a dramatic increase in the incidence of malaria in many parts of the world, and an increase in malaria-related mortality in some of these areas. The classic symptom of malaria is cyclical occurrence of sudden coldness followed by fever and sweating lasting four to six hours, occurring every two days. It causes widespread anemia and also direct brain damage. Severe malaria is almost exclusively caused by P. falciparum infection and usually arises 6–14 days after infection. Consequences of severe malaria include coma and death if untreated. Splenomegaly (enlarged spleen), severe headache, hepatomegaly (enlarged liver), hypoglycemia, and hemoglobinuria with renal failure may occur. Severe malaria can progress extremely rapidly and cause death within hours or days. Special Condition: Pregnant women are at higher risk of developing severe and fatal malaria. Hyperparasitemia, hypoglycemia and pulmonary edema are more common in pregnant women with P falciparum infections. Pregnant women should be treated promptly with appropriate doses of antimalarials. The parasite's primary hosts and transmission vectors are female mosquitoes of the Anopheles genus. Young mosquitoes first ingest the malaria parasite by feeding on an infected human Anopheles carrier mosquitoes and carry the infected Plasmodium sporozoites in their salivary glands. Only female mosquitoes feed on blood, thus males do not transmit the disease. The females of the Anopheles genus of mosquito prefer to feed at night. They usually start searching for a meal at dusk, and will continue throughout the night until taking a meal. Malaria parasites can also be transmitted by blood transfusions, although this is rare. The malaria parasite life cycle involves two hosts. During a blood meal, a malaria infected female Anopheles mosquito inoculates sporozoites into the human host (1). Sporozoites infect liver cells (2) and mature into schizonts (3), which rupture and release merozoites (4). After this initial replication in the liver (exo-erythrocytic schizogony [A]), the parasites undergo asexual multiplication in the erythrocytes (erythrocytic schizogony [B]). Merozoites infect red blood cells (5). The ring stage trophozoites mature into schizonts, which rupture releasing merozoites (6). Some parasites differentiate into sexual erythrocytic stages (gametocytes) (7). Blood stage parasites are responsible for the clinical manifestations of the disease. The gametocytes, male (microgametocytes) and female (macrogametocytes), are ingested by an Anopheles mosquito during a blood meal (8). The parasites‘ multiplication in the mosquito is known as the sporogonic cycle [C]. While in the mosquito's stomach, the microgametes penetrate the macrogametes generating zygotes (9). The zygotes in turn become motile and elongated (ookinetes) (10) which invade the midgut wall of the mosquito where they develop into oocysts (11). The oocysts grow, rupture, and release sporozoites (12), which make their way to the mosquito's salivary glands. Inoculation of the sporozoites into a new human host perpetuates the malaria life cycle (1). Since Charles Laveran first visualised the malaria parasite in blood in 1880, the mainstay of malaria diagnosis has been the microscopic examination of blood. Areas that cannot afford even simple laboratory diagnostic tests often use only a history of subjective fever as the indication to treat for malaria. The most economic, preferred, and reliable diagnosis of malaria is microscopic examination of blood films because each of the four major parasite species has distinguishing characteristics. Two sorts of blood film are traditionally used: Thin films are similar to usual blood films and allow species identification because the parasite's appearance is best preserved in this preparation. Thick films allow the microscopist to screen a larger volume of blood and are about eleven times more sensitive than the thin film, so picking up low levels of infection is easier on the thick film, but the appearance of the parasite is much more distorted and therefore distinguishing between the different species can be much more difficult. Diagnosis of species can be difficult because the early trophozoites ("ring form") of all four species look identical and it is never possible to diagnose species on the basis of a single ring form; species identification is always based on several trophozoites Rapid tests: In areas where microscopy is not available, or where laboratory staff are not experienced at malaria diagnosis, there are antigen detection tests that require only a drop of blood. Immunochromatographic tests (also called: Malaria Rapid Diagnostic Tests, Antigen-Capture Assay or "Dipsticks") have been developed, distributed and fieldtested. These tests use finger-stick or venous blood, the completed test takes a total of 15–20 minutes, and a laboratory is not needed. Methods used to prevent the spread of disease, or to protect individuals in areas where malaria is endemic, include: prophylactic drugs, mosquito eradication, and the prevention of mosquito bites. The continued existence of malaria in an area requires a combination of high human population density, high mosquito population density, and high rates of transmission from humans to mosquitoes and from mosquitoes to humans. If any of these is lowered sufficiently, the parasite will sooner or later disappear from that area, as happened in North America, Europe and much of Middle East. There is currently no vaccine that will prevent malaria, but this is an active field of research. Atovaquone-proguanil, trade name Malarone (Therapy and prophylaxis) Quinine (Therapy only) Chloroquine (Therapy and prophylaxis; usefulness now reduced due to resistance) Mefloquine, trade name Lariam (Therapy and prophylaxis)


