Dr: Salah Ahmed Endometriosis, Fibroids, PCOD
advertisement
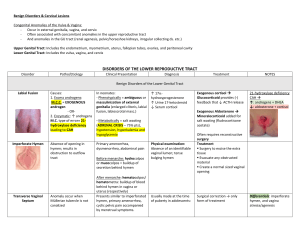
Endometriosis, Fibroids, PCOD Dr: Salah Ahmed Endometriosis - presence of endometrium (glands and stroma) outside the uterine cavity - occurs in as many as 10% of women in their reproductive years and in nearly half of women with infertility - sites: ovaries, pouch of Douglas, uterine ligaments, tubes, rectovaginal septum (common sites), peritoneal cavity, around umbilicus (less frequent) and lymph nodes, lungs, and even heart, skeletal muscle, or bone (uncommon) Pathogenesis: - Three theories: 1- Regurgitation theory: - currently the most accepted - suggests backflow of endometrium through the fallopian tubes during menstruation with subsequent implantation - disadvantage: this theory cannot explain lesions in the lymph nodes, skeletal muscle, or lungs. 2- Metaplastic theory: - suggests endometrial differentiation of coelomic epithelium - disadvantage: cannot explain the lesions in the lungs or lymph nodes 3- Vascular or lymphatic dissemination theory: - has been invoked to explain extrapelvic or intranodal implants Morphology: - the lesion contains functioning endometrium, which undergoes cyclic bleeding - grossly: -red-blue to yellow-brown nodules or implants - vary in size from microscopic to 1 to 2 cm in diameter - Often the lesions fuse to form larger masses - When the ovaries are involved, the lesions may form large, blood-filled cysts (chocolate cysts) - complicated by: 1- adhesions (bleeding, organization, fibrosis) which may lead to tubal obstruction and so to infertility 2- may undergo malignant change Clinical manifestations: - depend on the location of the lesions: 1- Extensive fibrosis of the oviducts and ovaries often produces discomfort in the lower abdominal quadrants 2- Pain on defecation reflects rectal wall involvement 3- dyspareunia (painful intercourse) reflects uterine serosa involvement 4- dysuria reflects involvement of the bladder serosa - In almost all cases, there is severe dysmenorrhea and pelvic pain as a result of intrapelvic bleeding and periuterine adhesions ADENOMYOSIS - the growth of the basal layer of the endometrium down into the myometrium - Nests of endometrial stroma, glands, or both, are found down in the myometrium between the muscle bundles microscopically - The uterine wall often becomes thickened and the uterus is enlarged as a result of the presence of endometrial tissue and a reactive hypertrophy of the myometrium - Because these glands derive from the stratum basalis of the endometrium, they do not undergo cyclical bleeding - marked adenomyosis may produce menorrhagia, dysmenorrhea, and pelvic pain before the onset of menstruation red-blue to yellow-brown nodules Endometrial glands and stroma within the myometrium Fibroids (Leiomyoma) - Benign tumors that arise from the smooth muscle cells in the myometrium -They are the most common benign tumor in females and are found in 30% to 50% of women during reproductive life - more frequent in blacks than in whites -Estrogens and possibly oral contraceptives stimulate their growth; conversely, they shrink postmenopausally Morphology: - firm, pale to gray, well-circumscribed lesions - may be single or multiple , small or large - location : - intramural (located within myometrium) - subserosal ( beneath the serosa ) - submucosal (close to endometrium) - may undergo cystic degeneration, calcification, red degeneration, necrosis, malignant change Clinical manifestations: - may be asymptomatic and be discovered only on routine pelvic or post mortem examination - The most frequent manifestation, when present, is menorrhagia, palpable mass - complication: 1- bleeding 2- reduced fertility 3- malignant change (very rare) Multiple fibroids (subserosal) Multiple fibroids (submucosal, intramural) interlacing smooth muscle fibers and spindle cells in swirling pattern POLYCYSTIC OVARIAN DISEASE (Stein-Leventhal syndrome ) - characterized by large ovaries with multiple cysts - Pathogenesis: 1- genetic factors (autosomal dominant ) 2-endocrine factors: high androgens, high LH/FSH ratio (peripheral conversion of androgens to estrone) - Morphology: large, gray-white ovaries with multiple subcortical cysts 0.5 to 1.5 cm in diameter - Clinical manifestations: - common in young women - hirsutism, acne (excess androgen) - menstrual disturbance (amenorrhea, oligomenorrhea) - anovulatory cycle (secondary to high LH\FSH ratio - infertility (anovulation) - obesity leading to increased insulin resistance and development of type 2 diabetes Subcortical cysts Hirsutism Thank you