Skeletal muscular disease- dystrophy
advertisement
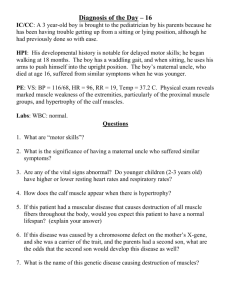
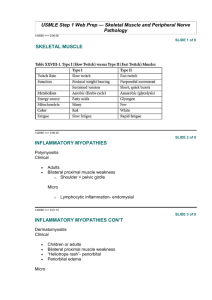
Skeletal muscle diseases a. The muscular dystrophies. • - Describe their pathogenesis. • - Describe their morphology. • - Discuss their clinical picture and management. b. The disease of neuromuscular junctions- MG • - Describe their pathogenesis. • - Discuss their morphology. • - Discuss the clinical picture and management. • Reference: Robbins Basic Pathology, 8th edition (pages 827 – 830). • Diseases of Muscles • What are the differences between the disease of Muscular Dystrophy and Myopathy? Are they related or totally separate diseases? • Myopathies: disorders with structural changes or functional impairment of the muscle “Weakness”. Not include U\L motor neuron lesion or MG. Include many types e.g.: MD. • Types:-Inflammatory, Congenital, Metabolic, Endocrine, Hereditary, Toxic\drug • Dystrophy: mean progressive loss of muscles(any types of muscles) ( 1-in 8,000 people) • Myopathy versus Neruogenic? • Myopathy= ( Bilateral & symmetrical), Neurogenic= (Asymmetric). A- The muscular dystrophies- Definition • Muscular dystrophy (MD) is a heterogeneous groups of familial inherited muscle disorders, each with unique phentotyic & genetic features lead to degeneration of skeletal muscle fibers. • MD recognized by progressive muscle weakness and muscle wasting. (generalized or localized). • Age: started in infancy or childhood, other appear later middle age • Affected sites: different Skeletal muscles groups, others may involve. • Limitation: • Difficulties with walking or Maintaining posture, Muscle spasms. Neurological, Behavioral, Cardiac, other Functional limitations. Who Discovered Muscular Dystrophy • Each diseases of (muscular dystrophy) was discovered by different person. > 43 types. • Muscular Dystrophy “MD” types: • common • 1- X-linked MD “Duchene MD” • 2- Becker Muscular dystrophy. • 3- Myotonic Dystrophy “ syndrome” • Less common - 4- Fascioscapulohumeral muscular dystrophy;-Autosomal dominant - 5- Oculopharyngeal muscular dystrophy;--autosomal dominant, - 6- Congenital muscular dystrophies;- autosomal recessive Duchene’s Muscular dystrophy (DMD) • Is most commonest and most fatal (x-linked recessive), non- inflammatory muscular myopathy in children-boys. • Etiology - caused by mutation in the dystrophin gene “X-linked inherited” (Deletion of DNA segment or single gene defect in short X- chromosome) deficiency of muscle protein dystrophin fragility • Prevalence: range 1- 3,000 to 1 – 3,500 boys. (all over the world) • Risk Because these are inherited disorders, risk include a family history of muscular dystrophy. • Clinical features; progressive-Proximal weakness • Presented at birth and become evident at 3 – 5 years-Boys • Gower’s maneuver- positive, lordosis, poor balance cont. • Joint contraction, scoliosis, decreased pulmonary function. (DMD, BMD) Pathogenesis • DYSTROPHIN- encode by DNA for anchor & interact all cells membrane protein support the whole membrane structure and connection between inside of the cell to outside. • DMD - Caused by mutation in the dystrophin gene “X-linked inherited” (Deletion of DNA segment or single gene defect in short X- chromosome) deficiency of muscle protein dystrophin or Production of bad dystrophin (with no function) Protein damage + membrane gaps increase+ calcium influx necrosis (Dystrophy) • Bekers Muscular Dystrophy- same like DMD but less severe and slow progression Duchene’s Muscular dystrophy (DMD) • Investigations; • Blood CK levels- raised, EMG- Reduced amplitude, • Muscle biopsy: Small groups of necrotic muscle fibers, regeneration, replaced by fat& fibrous stroma. • Abnormal Sacromere structure • Dystrophin protein deficiency demonstrated by special stain. • Molecular application for assessment of gene mutation • Management: • No treatment , Mainly supportive therapy ( Physiotherapy, physical therapy). • Steroid- prednisolone : significantly slow the disease progression. • https://www.youtube.com/watch?v=KA8W5UfE4ts MMD- Clinical features • MDM-Clinical features • • • • • Backer ‘s muscular dystrophy- BMS X-linked recessive inheritance Less severe form of dystrophy, Dystrophin protein is deficient. rd th Onset 5 – 15 years or even 3 or 5 decade. • Clinical features: • Muscle wasting resemble Duchene’s. • Proximal muscle weaknesses of lower extremities occur first. Cardiac muscle may be involved. • Investigation: results- similar like in Duchene’s • Management: No satisfactory treatment yet. Patients may survive till 5th decade. Morphology – DMD, BMS (1) Variation in fiber size (diameter)+ hypercontraction (2) Increased numbers of internalized nuclei (beyond the normal range of 3% to 5%). (3) Degeneration, necrosis (segemental& group) -phagocytosis . (4) Regeneration of muscle fibers. (5) Proliferation of endomysial connective tissue. • in advanced cases muscle fibers undergo degeneration and are replaced by fibrofatty tissue and collagen. • This feature distinguishes dystrophies from other myopathies, which also present with muscle weakness Internal central nuclei: Multiple NORMAL DYS-1 test Degeneration , regeneration, Inflammation replaced by fibrofatty tissue NEGATIVE DYS-1 test Myotonic dystrophy • • • • • • • • • Progressive disease in which the muscles and are slow relax after contraction- commonly dystrophy in adult. (Myotonia= is an inability to relax muscles at wil) Adolescence\adult onset -slow, children –congenital- rapid Etiology: is Autosomal dominant genetic disorder with triple repeat mutation. The correlation between disease severity , age at onset and approximate size of triple mutation. Investigation: Muscle biopsy-atrophy with internalized nuclei. EMG- show myotonia Molecular test • Management: No satisfactory treatment yet. • Phenytoin lead to delayed the relaxation. Myotonic dystrophies- Pathogenesis • Myotonia- inability to relax muscles. • Inherited as an autosomal dominant trait • Repeat expansion of trinucleotide CTG on chromosome 19 • This will affect the mRNA for the dystrophia myotonia protein kinase (DMPK) is an enzyme that in humans is encoded by the DMPK gene (CA channles, GTPase) Sustained involuntary contraction. • Sustained involuntary contraction of a group of muscles & stiffness, shrinkage, wasting (hands, legs, neck, face). Inherited as an autosomal dominant trait Affect DMPK Involuntary sustained muscle contraction and stiffness Clinical features: • Facial muscle weakness • Ptosis, frontal baldness, • Gyanecomastia • Neck muscles weakness • Distal limbs muscles weak • Diaphragm muscle weak • Respiratory failure. • Dysphagia • Cardiac muscle involvement “cardiomyopathy” • Mental retardation. • Proximal muscle are spared along the course. Morphology of MMS • • • • • Mytonic dystrophy- (MS) : 1) All features in No. (1-5) + 2) Presence of multiple internal nuclei 3) Ring fiber: formed by a bundle of peripheral myofibrils that are circumferentially oriented (PATH stain, EM). • 4) Relative selective atrophy. • 5) Degeneration and regeneration seen in severely affected muscles. Mytonic dystrophy Fiber size variation- Internal nuclei in some fibersPyknotic nuclear clumps Esterase Internal nuclei: Multiple NADH stain Pyknotic nuclear clumps the disease of neuromuscular junctions. Myasthenia Gravis - MG • MG- is a Chronic autoimmune neuromuscular muscle disease causedb.by immune-mediated loss of acetylcholine receptor, chr. Discuss the disease of neuromuscular junctions. by Varying degree of fluctuates weaknesses. (MG = grave Definition muscle weakness). • Affect area: Muscle neuro-transmitter • Prevalence: of about 30,000 in 100,000 persons. • Age: any age group, but commonly (F< 40 yrs , M> 60) of life. • Sex: Any gender, commonly affect female> male, older equally • Evidence based nearly all cases: decrease in the number of muscle acetylcholine receptors (AChRs), and circulating antibodies to the AChR are present in nearly all cases. • Risk- thymic abnormalities are common in these patients MG-PATHOGENESIS • Autoimmune basis: • Autoantibodies usually against the the nicotinic AChR lead to loss of functional AChRs at the neuromuscular junction by: • (1) Fixing complement - causing direct injury to the postsynaptic membrane. • (2) Increasing the internalization and degradation of the receptors. • (3) Inhibiting binding of acetylcholine. • HLA & environmental association. Outcomes: • A) Communication between nerves and muscles is disrupted (action potential affected) • B) Sensory as well as autonomic functions are not affected. • C) Electrophysiologic studies are notable for diminished. Neuromuscular junctions diseases- Morphology • 1- Muscle biopsy- (light microscopic): • a) Specimens are usually unrevealing. • b) In severe cases type 2 fiber atrophy due to disuse may be found. • 2- Electron microscopy: • a) The postsynaptic membrane is simplified, and there is loss of AChRs from the region of the synapse. • b) Immune complexes and the complement membrane attack complex (C5–C9) can be found along the postsynaptic membrane as well. • 3- Administration of anticholinesterase agents- Test • 4- Nerve conudcting studies • 5- CT- scan for thymus assessment • 6- Blood screening for auto-antibodies (anti-AChR or MuSK) Clinical features • 1- Voluntary muscle Weakness begins with the extraocular muscles; drooping eyelids (ptosis) and double vision (diplopia) facial expression, swallowing, arms , legs. • 2- Generalized weakness- the weakness fluctuates over days, hours, or even minutes. ( Aggravated- with exercised) • • 3- Intercurrent medical conditions can lead to exacerbations. • 4- Respiratory compromise (major cause of mortality) Management • 1- Avoid stress, exercise,+ Better ventilatory support. • 2- Anticholinesterase drugs. • 3- Steroid- prednisone+ Immunosuppressant=cyclosporin. • 4- Plasmapheresis + Immunoglobulin . • 5- Thymectomy wen thymic lesions are present.+ BM transplant. • No preventive measure can be adopted. • Prognosis- MG not affect life expectancy, can practicing daily activity even. • Myasthenia crisis- respiratory muscle weakness (ARF) SUMMARY OF MD Muscular Dystrophy- clinical features Type Onset Age (years) Clinical Features Other organ systems involved Duchenne Before 5 1.Progressive weakness of girdle muscles. 2.unable to walk after age 12 3.progressive kyphoscoliosis 4.Respiratory failure in 2dor 3d decade. Cardiomyopathy Mental impairment Becker early childhood to adult 1.Progressive weakness of girdle muscles 2. able to walk after age 15. 1.3. Respiratory failure may develop by 4th grade Cardiomyopathy 5-25yr Muscular dystrophy – clinical features Type Onset Age (years) Clinical Features Other organ systems involved Congenital At birth or within 1st few months .Hypotonia, contractures, delayed milestones Progression to respiratory failure in some; CNS and Eye abnormalities Facioscapulohumer al Before age 20 Slowly progressive weakness of face, shoulder girdle, and foot dorsiflexion Deafness Coat’s (eye) disease Oculopharyngeal 5th to 6th decade Slowly progressive weakness of extraocular, pharyngeal, and limb muscles ______ Myotonic ADULTONSET , 2nd decade, Congenital onset Slowly progressive weakness of face, shoulder girdle, and foot dorsiflexion inability to relax muscles Cardiac conduction defects Mental impairment Cataracts, hypersomnia Frontal baldness Gonadal atrophy