Practical pathology of Adrenal, PTH
advertisement

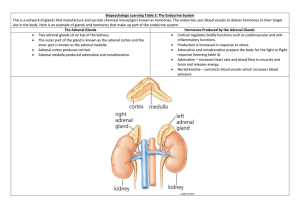
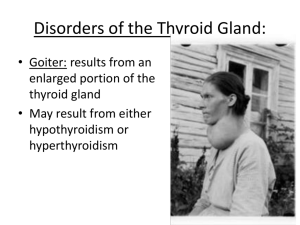
Practical 1 Adrenal and parathyroid glands Dr.Ashraf A.fatah Deya Normal Adrenal glands= weighs from 4 to 6 grams Head, body and tail . Adrenal Cortex Zona glomerulosa Zona fasciculata Zona reticularis 3 Practical 4:Pathology of Parathyroid &Adrenal Glands • By the end of this session, the student should: • Identify the various conditions of parathyroid and adrenal glands associated with morphological changes (microscopic and gross). • Robbins Basic pathology 9th edition pg - 734 738 Adrenal glands hyperfunction state 1. 2. 3. Adrenal cortical hyperplasia= Cushing Syndrome. Congenital Adrenogenital syndrome=(sex steroid hormones) Adrenal cortical adenoma\Associated with Hyperaldosteronism = (Conn’s syndrome). 4. Cushing syndrome= role of corticotropin level to rule out (Pituitary/Hypothalamic-Based Hyperplasia\adenoma, Paraneoplastic (Ectopic) Production (lung ca), primary cortical adenoma\hyperplasia). 5. Neuroblastoma (catecholamine precursors and their metabolites, e.g. metaphrine and pro-metaphrine). 6. Phaeochromocytoma (catecholamine precursors and their metabolites, e.g. VMA, metaphrine and pro-metaphrine) - A) Atrophied adrenal glands B) Normal adrenal glands C) Adrenal hyperplasia Case No- 1 • Q1 Write two clinical examples for the morphologic features shown in photo No (A) =atrophy? • A1= Adrenal atrophy • 1) Addison’s disease (10% ) OR 90% in TB • b) Long term corticosteroid therapy shuts off • A2= Adrenal hyperplasia • Q2 Write four clinical • a) Pituitary adenoma secreting examples for the ACTH (Pituitary -Cushing's morphologic features disease). shown in photo No (C) ? • b) Ectopic ACTH production• = hyperplasia (paraneoplasia- Cushing's syndrome). • Q3- describe the • c) Congenital Adrenogenital morphological appearance syndromes. of C? • D) Idiopathic hyperplasia Case No -2 • The parents of a girl notice that she has developed features that suggest puberty over the past 6 months. • On physical examination, she has few sex characteristics with Ambiguous genitalia. • Lab investigationincreased pituitary ACTH production, Markedly elevated Testosterone Answers- Case No -2 • Q1- what’s the most likely the diagnosis? • Congenital Adrenal Hyperplasia (Adrenogenital Syndrome) • Q2-What would be the adrenal status\ morphology in this patient? • Bilateral enlarged hyperplastic adrenals (upto 16 g) with cerebriform appearance • Q3- What is the etiology of this condition? • Autosomal recessive disorders characterized by enzymatic defects (5 enzymes) in cortisol synthesis e.g 21-hydroxylase • Q4-Write 4 other investigations, which are helpful in reaching the final diagnosis? • Q5- What’s the complications of this syndrome? Answer- case-2= Congenital Adrenal Hyperplasia adrenal hyperplasia. A4= 1- S. cortisol level (a.m\ . • Congenital Normal cortex p.m)(Decrease) 2- S. Aldosterone ( Decrease) 3- ACTH level ( Increase) 4- Increased levels of Progesterone , 17-OHprogesterone, and dehydroepiandrosterone (DHEA) Testosterone . 4-Abdominal ultrasound Looking for adrenals A5- Sexual development abnormalities, Hypertension, Adrenal insufficiency, Sodium imbalances. • replaced by clear-cell nodules Normal cortex replaced by clear-cell nodules “lipid depleted”. Differential diagnosis: 1- Adrenal cortical hyperplasia 2- Beckwith-Wiedemann syndrome: 13 Consequences of C-21 hydroxylase deficiency: Impairs the synthesis of both cortisol and aldosterone Summary of Adrenogenital Syndromes Laboratory 21-OHase Deficiency 11-OHase Deficiency 17-Ketosteroids ↑ ↑ 17-Hydroxyprogesterone ↑ ↑ 17-Hydroxycorticoids ↓ ↑ Mineralocorticoids ↓ ↑ 15 Case No- 3 • A 28-year-old, otherwise healthy man sees his physician because he has had headaches for the past 2 weeks. • Physical examination yields no remarkable findings except for a blood pressure of 170/110 mm Hg. Trousseau’s Sign while taking blood pressure. – Lab investigations revealed – Hypernatremia – Hypokalemia – ↑ plasma aldosterone level – Normal glucose level • An abdominal CT scan shows an enlarged right adrenal gland. • A right adrenalectomy is done; the figure shows the gross appearance of the specimen. Q1-what is the diagnosis? Q2- Describe the morphologic features? Q3- write single screening test of choice for diagnosis? Q4- write other causes of primary hyperalosteronism ? 18 Answer- Case No- 3 = primary hyperaldosteronism (Conn syndrome). • A3= The plasma • A2=a) The gross specimen aldosterone: Plasma renin Yellow-orange tumor nodule activity ratio > 30 is in the adrenal cortex, diagnostic. localized, nodular, solitary, circumscribed nature. • (function or non-functional)?? • A4= common: • 1- Unilateral Adrenal adenoma (2\3). • b) Histologic features : • 2- Bilateral adenoma (1\3) • The neoplastic cells are vacuolated \clear because of the presence of • Less common: intracytoplasmic lipid, with • Unilateral Adrenal carcinoma <1% mild nuclear pleomorphism. • Unilateral hyperplasia < 1% No Mitotic activity &necrosis. • Familail cases < 1% Case No- 4 • 40-year-old female sees her physician because she has had headache, weakness, and a 5-kg weight gain over the past 3 months. • On physical examination, her face is puffy. Her temperature is 36.9°C, pulse is 79/min, RR=15/min, BP= 160/75 mm Hg while lying down. • A radiograph of the spine shows a compressed fracture of T11. • MRI- pituitary g. was clear. • Laboratory findings (see table). • Q1- Discuss the Lab findings and what’s the value of doing dexamethasone test,? • Q2-what is the diagnosis? • Q3- describe the morphology of the excised gland? Test name concentration Reference value Glucose 7.1 mmol\L 3.6 – 5.5 Serum Na+ 150 mmol\L 135 - 145 Serum K+ 3.1mmol\L 3.5 - 5 Plasma Cortisol 414 nmol\L < 138 Dexamethasone suppression test Not suppressed in high dose Free 24 Urine cortisol-UFC 596 nmol\day 55 - 228 "moon facies," reddish face thin upper extremity truncal obesity purple abdominal striae 22 Adrenal gland adenoma from a patient with Cushing's syndrome C\S solid yellowish, circumscribe mimic fasciculata zone 23 Answer case No- 4 = Cushing syndrome • A1= The dexamethasone suppression test (1mg at 22:00- 6days) is used to localize the source of excess cortisol is employed in an attempt to induce suppression of the hypothalamic–pituitary–adrenal cortical axis (HPAC) • When Low-dose and High-dose dexamethasone trials secretion Interpretation • 1) Suppression occur in high dose= ACTH-secreting pituitary adenoma • 2) Failure of suppression in high dose= Cushing syndrome resulting from ectopic adrenocorticotrophic hormone (ACTH; corticotrophin) production, ectopic corticotrophin-releasing hormone (CRH) production, and cortisol secreting adrenal tumors. • 3) Borderline repeated + do further investigations. • A2= Cushing syndrome due to adrenal cortical adenoma • A3= Macroscopic:The cut surface of the adenoma is marbled yellow and brown, atrophied compressed cortix. • Microscopic: Cortisol-secreting adenoma showing cells with clear and dark cytoplasm and foci of myeloid metaplasia. various forms of Cushing syndrome Lab test Pituitary Cushing’s Adrenal Cushing’s Ectopic Cushing’s Serum cortisol Increased Increased Increased Low-dose DST Cortisol not suppressed Cortisol not suppressed Cortisol not suppressed Urine for free cortisol Increased Increased Increased Plasma ACTH Normal * to increased Low Markedly increased High dose DST Cortisol suppressed Cortisol not suppressed Cortisol not suppressed 26 5- Adrenal cortical carcinoma. The hemorrhagic and necrotic tumor compresses the upper pole of the kidney, Scattered atypical nuclei . Adrenal glands hypofunction state Hypofunction of adrenal cortex. Can be of two types: A. Acute adrenocortical insufficiency - causes include: 1.Abrupt withdrawal of corticosteroids . 2.Waterhouse-Friderichsen syndrome. B. Chronic adrenocortical insufficiency 1. Addison’s disease. 2. Chronic granulomatous adrenalitis. 3. Others (viral, bacterial, metastatic, etc..). Case No-6 • A 32-year-old woman with SLE has been treated with corticosteroid therapy for several years, because of recurrent lupus nephritis. • She undergoes an appendectomy for acute appendicitis. • On postoperative day 2, she becomes drowsy and develops severe nausea and vomiting. She then becomes hypotensive. • Laboratory studies were requested. Reference value 135-145 Tests Result Na + level 128 mmol\L K+ level 5.8mmol\L 3.5-5 CL- level 105mmol\ 95-105 L Glucose 60mg\Dl 65- 99 Creatinine 1.3 mg\dL 0.5-1.2 • Q1- What’s the diagnosis, and mention causes given in this scenario? • Q2- Identify the morphologic? • Q3- differential diagnoses? CO2 19 mol\L BLOOD CULTURE Negative 24-32 Primary adrenal insufficiency. A thinned cortex shows loss of normal zona fasciculata with clear cells. Answer case No 6= Primary adrenocortical insufficiency (Addison disease) • A1 = Primary adrenocortical insufficiency (acute addisonian crisis). • Causes: 1) Long term corticosteroid therapy shuts off. • 2) Stress of surgery • 3) Autoimmune condition, e.g. SLE • 4) Idiopathic • A2= Adrenal atrophy - Long-term corticosteroid therapy shuts off corticotropin stimulation to the adrenal glands, leading to adrenal atrophy • Residual cortical cells are hypertrophied and have compact eosinophilic cytoplasm and enlarged nuclei (ACTH stimulation effect). • Both gland Wt.= 3mg. • A3-Adrenal hemorrhage, tumor, metastatic, infections, amyloid Case 7- Adrenal- caseating granuloma of tuberculosisexample of chronic primary adrenal insufficiency= Addison's disease is much more often the cause for chronic adrenal 33 insufficiency. Case 7- Adrenal- caseating granuloma of tuberculosis- Case No- 8 • A 4-year-old, previously healthy child died suddenly after complaining of a fever, Marked Skin purpura, sore throat , for few days and suddenly collapsed. • At autopsy, her adrenal glands are enlarged, and there are extensive bilateral cortical hemorrhages. • Q1- What is most likely the diagnosis, describe the morphologic features? • Q2- Write two underling etiological factors? • Q3- mention the main complications of this condition? These adrenals are black-red from extensive hemorrhage in a patient with meningococcemia. A1-Waterhouse-Friderichsen syndrome A1-Microscopically: • Hemorrhages, with necrosis of both cortical and medullary tissue. • Little residual cortical architecture is discernible. A2= 1- Sepsis caused by meningococcal infection. 2- Anticoagulant drugs. 3- Viral infection= CMV. marked hemorrhagic necrosis with acute adrenal insufficiency. A3= Septicemia, DIC Endotoxic shock, Death. Parathyroid glands Disorders of Parathyroid glands 1. Hyperparathyroidis - Primary- Autonomous spontaneous overproduction • of PTH, elevated calcium level. - Secondary- PTH levels are raised, but serum calcium is not elevated. - Tertiary- Long-standing secondary hyperparathyroidism leads to autonomous hyperactive parathyroids e.g CRF. 2. Hypoparathyroidism 40 Case No- 9 TEST VALUE • A 40-year-old man visits 8.5- 10.5 SERUM 11.5 the physician because of CALCIUM mg\dL weakness and easy 30-110 ALP 317 U\L fatigability of 2 months' S. PTH 127pg\ml 14- 66 duration. • Physical examination yields no remarkable findings. • Laboratory studies What is the most likely cause which is near the top of the of these ? reference range. • A radionuclide bone scan Write the most common fails to show any areas of syndrome associate with condition? increased uptake. • Tc99 scan was requested CASE 9- Parathyroid adenoma Parathyroid Tc99 scan Parathyroid scan following intravenous administration of Tc99 (technetium-99msestamibi radionuclide scan) In addition to radiotracer uptake in both thyroid lobes, a small area of increased activity inferior to the left lobe of the 42 thyroid, consistent with a parathyroid adenoma. Primary Hyperparathyroidism- due to PTH adenoma PTH ADENOMA Brown tumor Fibrosis of BM, hemorrhage and a cluster of osteoclast giant cells Parathyroid Adenoma Primary Hyperparathyroidism • Primary • This entity was defined in part by Von Recklinghausen under the term osteitis fibrosa cystica generalisata. • Parathyroid adenoma 80% • Hyperplasia 10-15%. • Parathyroid ca <5% • Most likely syndrome: Multiple endocrine neoplasia (MEN) type 1. Case No- 10 • A 26-year-old woman with a history of end-stage renal disease (ESRD) and (CHF). she had been on vitamin D therapy-6\12, for suspected renal osteodystrophy. • Q1- What’s the most likely diagnosis, describe the morphology? • Q2- Mention other helpful diagnostic tests? TEST VALUE SERUM CALCIUM ALP 8.8mg\dL 8.5- 10.5 340U\L 30-110 S. PTH 110pg\ml 14- 66 Secondary hyperparathyroidism= Secondary Parathyroid hyperplasia,- as a consequence of chronic renal failure. 4 glands are involve - Not like a case of adenoma +\- Little or no adipose tissue. Note the pink oxyphil cells here. 48 Parathyroid Tc99 scan- indicated Case-11 • An infant is born at term to a 25-year-old woman. • On newborn physical examination, the infant is found to have an enlarged abdomen, but there are no other abnormal findings except for slightly elevated blood pressure. • An abdominal ultrasound scan shows a right retroperitoneal mass in the adrenal gland. The mass is resected surgically, and histologic sections reveal small blue cells tumour. • Lab investigation revealed elevated urinary metanephrine level. • __________________________________________ • Q1- Describe the morphologic features given in the photo attached? • Q2- What is the diagnosis? • Q3- what is the clinical significance of (metanephrine)? Answer Case No - • A1= Gross appearance: • Hemorrhagic, partially encapsulated tumor has displaced the opened left kidney and is impinging on the aorta and left renal artery. • Microscopic: This tumor is composed of primitive small ”blue” cells embedded in a finely fibrillar matrix with Homer-Wright rosettes • A2= Adrenal neuroblastoma • A3= Metanephrine– is indicative of this tumor, which is produce high levels of catecholamine precursors and their metabolites. Case No- 12 • A 35-year-old man with severe headaches and marked hypertension, undergoes surgical resection of a left suprarenal mass that appeared gray and tan centrally and yellowish on the cortex. • On microscopy, large pink cells are arranged in nests with capillaries between them. • Q1- What’s the most likely diagnosis, describe the morphology? • Q2- Describe the “rule of 10s .”? • Q3- Mention other helpful diagnostic tests? • Q4- Describe the association with pheochromocytoma and MEN 2A and 2B.? Answer case - Pheochromocytoma • The tumor is enclosed within an attenuated cortex and demonstrates areas of hemorrhage. • The comma-shaped residual adrenal is seen below. • Other helpful diagnostic tests: Urinary or serum catecholamines such • as vanillylmandelic acid (VMA). • ◆ Acute complications: Acute LVF , pulmonary edema, MI, ventricular fibrillation and • and CVA, CHF, and death Zell-Ballen pattern 55 Pheochromocytoma • 1- Nests of cells with abundant cytoplasm- derived from . Chromaffin cells “neural crest cells origin”. • 2- Granules containing catecholamine are not visible in this preparation. • 3- It is not uncommon to find bizarre cells even in pheochromocytomas that are biologically benign, and this criterion by itself should not be used to diagnose malignancy. • Electron micrograph- tumor contains membrane-bound secretory granules in which catecholamines are stored