The Address in PowerPoint outline
advertisement

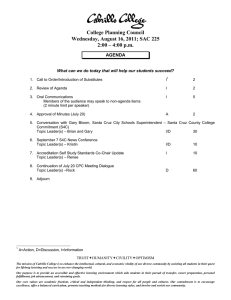
Increasing Access to Care for the Medically Underserved: Four County Models Annette Gardner, PhD, MPH Institute for Health Policy Studies University of California, San Francisco March 3, 2007 How many of us think of access: “Uh oh, your coverage doesn’t seem to include illness.” Access or getting the health care one needs Key barriers: linguistic, cultural, ethnic, geographic, economic, institutional Insurance matters uninsured delay seeking care There is no one solution consider a “holistic” approach California Counties Where the Action is At Bear significant responsibility (Section 17000) Willing and able to undertake coverage expansions, e.g., CHIs Vulnerable - sustainability is a key issue Presentation Objectives Describe barriers and opportunities to expanding access to care in 4 counties (Fresno, Humboldt, Santa Cruz and Solano) Increase understanding of access initiatives underway/proposed Describe strategies for financing, planning and implementing access initiatives, e.g., access coalitions Describe efforts to expand county capacity, e.g., IT, integrated services Study Approach Interviews with representatives from 4 counties comparable to Sonoma, including: County health agency official Access coalition director Provider representative Medi-Cal plan representative Gather information on: Access and policy issues Key stakeholders and their roles Access activities (type, funding) Models for planning, financing, implementing access activities IT Effort to integrate services, achieve costsavings Study Findings: Key Determinants Four different, four similar counties: (see handout) Rural/suburban Size (< 1M people) Programs for the medically indigent: 2 CMSP (Humboldt, Solano) and 2 MISP (Fresno, Santa Cruz) Range of uninsured, from 7% (Solano) to 18% (Fresno) Medi-Cal model: 2 COHS (Santa Cruz, Solano), 1 FFS (Humboldt) and Medi-Cal managed care (Fresno, 2-Plan) Health care delivery systems: county-run services (Solano and Santa Cruz) vs. noncounty services (Fresno and Humboldt) Barriers to Care: Access Issues Commonalities exist: Lack of insurance (and care) for low-income adults Lack of specialty care (mental health, dental care) Differences: Geographic barriers Target populations, i.e. farm workers, elderly Services, I.e. existence of county-run health care facilities, lack of hospital care Policy Issues That Impede Counties Lack of flexibility/control over existing programs, such as MediCal, CMSP/MISP, Medicare Rising medical costs Insuring the undocumented Low commitment to expanding coverage Low reimbursement for services County Access InitiativesObservations All counties are undertaking access initiatives, ranging from coverage expansions to service expansions There is some diversity within each type of initiative, e.g., activities to attract providers, coverage of different adult populations Children are addressed - adults are in the “proposed” stage IT systems/applications vary, piecemeal Efforts underway to integrate MH in primary care settings Financing Access Initiatives Multiple funding sources - public (federal, state and local) and private (foundations, United Way, providers) Tend to be piece-meal, project driven One study county, Sonoma, has sustainable funding (Tobacco Settlement funding) Vehicle for Change: Access Coalitions All 4 study counties have an organization to plan and undertake access initiatives: Vary in age/maturity Vary slightly in membership emphasize broad-based participation of leadership Recognized as lead agency in 3 of 4 counties Capacity - can staff/support county-wide access initiatives Wear multiple “hats” - convener, planning body, implementation Rely on grant funding Four Access Coalitions Coalition Launch Date Fresno Healthy Community’s Access Partners (HCAP) 2003 Community Health Alliance of Humboldt-Del Norte (CHA) 2000 Health Improvement Partnership of Santa Cruz County (HIP) 2003 Solano Coalition for Better Health 1988 Access Coalitions: Factors for Success High stakeholder commitment and involvement, particularly by top leadership - “culture of collaboration” Strong partnership with county Track record of accomplishments Agreement on coalition goals Established relationships among stakeholders Staff support to convene, coordinate, and facilitate stakeholders and capacity to plan and implement access initiatives The Future: County IT Capacity Uneven, piece-meal One commonality - adoption of One-e-App to streamline enrollment in public programs Some progress in developing centralized data systems (Humboldt, Santa Cruz) Varied adoption of TM, electronic exchange systems, such as HRE/HER The Future: Integrated Systems of Care Integration of behavioral health services in primary care settings (Prop 63) Other: Frequent Users project (Solano) IT in tandem with insurance coverage (Santa Cruz) TM mental health services in multiple settings (Humboldt) The Future: Cost-effective Systems of Care Limited activity - strategies emerging: Shared risk funding model among providers (Santa Cruz) Registries that have potential to morph into county-wide initiatives (Humboldt, Santa Cruz) Included as part of Coalition goals (Fresno) Leveraging of funding (Solano) Summary Counties can address intractable problems in innovative ways - have the means and the motivation Access coalitions may be critical in overcoming barriers, undertaking activities that individual organizations could not do otherwise Though counties vary, they can adopt similar approaches to reducing the barriers to health care Acknowledgements Funded by the California Program on Access to Care, University of California, Office of the President Contact Information Annette Gardner, PhD, MPH Institute for Health Policy Studies, University of California, San Francisco (415) 514-1543 Email: annette.gardner@ucsf.edu Panel: Four County Models County/coalition descriptions Realistic expectations - what can counties do? Opportunities? Strengthening stakeholder relationships-strategies? Advice for Sonoma County? Panel Participants Norma Forbes, Fresno Healthy Community’s Access Partners (HCAP) Allan Katz, Community Health Alliance of Humboldt-Del Norte, Inc. (CHA) Eleanor Littman, Health Improvement Partnership of Santa Cruz County (HIP) Patrick Hughes, Solano Coalition for Better Health