Dr. Nabil Kronfol
advertisement
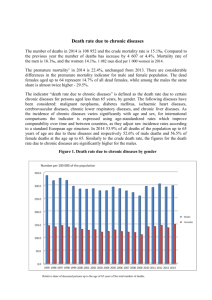
Integrating the care of NCD into PHC ECOSOC/UNESCWA/WHO Doha, May 10th 2009 Nabil M Kronfol MD, DrPH The Stake for NCD Control • The health problems caused by NCDs are today leading to premature death of more than 35 million people every year because of heart disease, stroke, cancer, chronic lung disease and other chronic health problems. • Out of 58 million deaths estimated to take place annually, more than 30% are caused by various forms of heart disease, about 16% by cancer and another 16% by other chronic diseases. Message One • Evidence from many countries, both industrialized and developing, show that countries that have a health system anchored on Primary care have better health outcomes, including morbidity and mortality indicators for NonCommunicable Diseases. Evidence from Canada • HCS based on PHC reduce health disparities, particularly for areas with the highest income inequality, including improved vision, more complete immunization, better blood pressure control, and better oral health. (Lynn Wilson) • Better access to general practice care offers reduced all-cause mortality and mortality caused by cardiovascular and pulmonary diseases • More continuity of care leads to better management of chronic disease • GPs offer better preventive care • A higher primary care physician supply leads to decreased incidence and mortality caused by colon cancer, and improved detection of breast cancer and cervical cancer • General practice offers fewer tests, high patient satisfaction, less medication use, with lower care related costs • Adequate resources for general practice care offers reduced emergency departments and hospital presentations with fewer and shorter hospitalizations The Evidence • Many other studies done within countries, both industrialized and developing, show that areas with better primary care have better health outcomes, including total mortality rates, heart disease mortality rates, and infant mortality, and earlier detection of cancers such as colorectal cancer, breast cancer, uterine/cervical cancer, and melanoma. The opposite is the case for higher specialist supply, which is associated with worse outcomes (Starfield). Lessons Learned From International Experience • NCDs are preventable through interventions against their risk factors • Strategies to reduce established risk factors should be combined with strategies to prevent the emergence of risk factors • To have an impact, interventions should be of appropriate intensity and sustained over extended periods of time • Success requires community participation, supportive policy decisions, legislation, and health care reforms • More health gains are achieved by influencing public policies in other sectors like trade, education, agriculture, food production, urban development and taxation than by changes in health policy alone. Message No Two • There is evidence that primary health care systems that support decentralization, community empowerment, an integrated referral system and universal coverage have achieved better outcomes for the promotion of health, the prevention of chronic illnesses, the screening for NCD and the care of patients afflicted with NCD. There is a need for health systems to evolve and adapt to address the risks of NCD. Decentralization • ‘Everybody’s Business’, (WHO 1998) suggested that lack of progress with PHC implementation, and poor outcomes, can often be attributed to a reluctance to decentralise authority to local levels, a failure to move resources between curative, promotive and preventative activities and a weak capacity in social epidemiology and health services research. A different paradigm for health systems • The burden of chronic diseases is high in low-income and middle-income countries and is predicted to increase with the ageing of populations, urbanisation, and globalisation of risk factors. • An integrated approach to the management of chronic diseases, irrespective of cause, is needed in primary health care. • Management of chronic diseases is fundamentally different from acute care, relying on assessment of risk factors, detection of early disease and identification of high risk status; • A combination of pharmacological and psychosocial interventions and long-term follow-up. • To meet the challenge of chronic diseases, primary health care will have to be strengthened substantially. Vertical programs versus PHC • Gish:“Alma-Ata affirmed health as a human right and sought to have interventions focus on the underlying social, economic and political causes of disease and illness as well as for comprehensive health care. • Mahler: ” Vertical programs do not do this. We were crushed by the IMF. The hammer that was used to crush us was the vertical intervention – ‘selective primary care’. • Cueto: “Vertical programs make it appear that we are “helping”, while in fact we are undermining political interventions that deal with the underlying causes of disease. • Even if vertical programs improve indicators widely, they do not fundamentally change power relationships or the underlying social structures that are the ultimate cause of diseases”. Effective interventions for NCD • Usual medical care often fails to meet the needs of chronically ill patients, even in managed, integrated delivery systems. The medical literature suggests strategies to improve outcomes in these patients. • Effective interventions tend to fall into one of five areas: the use of evidence-based, planned care Reorganization of practice systems and provider roles Improved patient self-management support Increased access to expertise; and Greater availability of clinical information. • The challenge is to organize these components into an integrated system of chronic illness care (Wagner et al). Cardiovascular Diseases • “This report paints a clear and strong argument that we need now to increase the attention we give to cardiovascular disease in low- and middle- income countries because of the health and economic impacts. • This argument becomes even stronger in light of the emerging demographic profile of the world, where every nation is facing a change in its age structure • The time to act to minimize the impact of chronic disease is now, both to protect today’s work-forces and to diminish the burden of costly disability in the future. (The Earth Institute Report) Message No Three • Controlling Non-Communicable diseases requires active participation from individuals, communities and Government. NCD intervention necessitates Legislation from several Ministries to create an environment that supports prevention and sustainable actions. Strong Government Commitment • NCDs are already the leading health problems and are on the rise • Market forces will further promote tobacco use, unhealthy diet. • NCD prevention cannot be considered an issue of personal choices and behavior. The Role of the Government is key and action by various sectors is mandatory • Cost-effective interventions exist and can be implemented at the PHC level. • Initial response should include establishment of a surveillance system and initiate policy changes as early as possible • Integrating interventions into PHC is effective but health systems needs to be strengthened • There is a need to develop a conducive environment which requires action by all sectors and requires legislation and regulation • This requires a strong role and responsibility for the government. Message No Four • Addressing NCD necessitates a performing health workforce that is well prepared and incentivized to respond to the needs of patients for care (including self care and home care) and for information and communication. Importance of Communications • Patients want better communication. Instead of receiving a physical examination or a prescription, patients would rather spend precious time with their doctors discussing their conditions and hearing about ways to stay healthy. • Three specific areas that patients want their doctors to emphasize: Communication, Partnership and Health Promotion • Patients wanted an open discussion of their feelings about treatments in order to reach cooperative decisions • Patients wanted to learn about ways in which they can improve their health or prevent future illness • Fewer patients wanted an examination and only a quarter of those surveyed wanted a prescription. Coordination of care • Coordination between care providers of different disciplines is essential to improve the quality of care, in particular for patients with chronic diseases (Haggerty et al) . • The way in which general practitioners (GP’s) and medical specialists interact has important implications for any healthcare system in which the GP plays the role of gatekeeper to specialist care (the Netherlands and the UK). However, in countries without a gatekeeper system, coordination of care is a concern as well (Shoen). • A large European study showed that patients in different countries value different aspects of healthcare (Groenwegen). ‘Being taken seriously’ is generally regarded as most important and ‘waiting time the least important. • “When evaluating the transition from primary to secondary care and vice versa, we need to have a thorough knowledge of the experiences and preferences of patients”. The cost of caring • The rise of chronic diseases has uncovered further problems: the burden of long-term care on health systems and budgets, the costs that drive households below the poverty line, and the need for prevention in a situation in which most risk factors lie outside the direct control of the health sector. In other words: fairness, efficiency, and multi-sectoral action. Catastrophic Impact • Cost studies are scarce, but in middle-income countries, the cost of illness not only represents much of the direct costs of medical care, but also has an impact on family disposable income. • Studies have reported that in low-resource settings, given incomplete health coverage and partial insurance, out-of-pocket expenses are high. Persons with chronic conditions often have to forego care because of their inability to pay. • This warrant attention from poverty-reduction programs. • Evidence shows that to have an impact on the burden of chronic diseases, action must occur at three levels: population-wide policies, community activities, and health services. The impact of NCD • Chronic diseases in 23 countries were responsible for 50% of the total disease burden in 2005. • If nothing is done to reduce the risk of chronic diseases, an estimated US$ 84 billion of economic production will be lost from heart disease, stroke, and diabetes alone in these 23 countries between 2006 and 2015. (Abegunde et al study) Summing up the evidence: The OECD Review • The strength of a country's primary care system was negatively associated with (a) all-cause mortality, (b) allcause premature mortality, and (c) cause-specific premature mortality from asthma and bronchitis, emphysema and pneumonia, cardiovascular disease, and heart disease. • This relationship was significant even while controlling for macro-level (GDP per capita, total physicians per one thousand population, percent of elderly) and micro-level (average number of ambulatory care visits, per capita income, alcohol and tobacco consumption) determinants of population health. • Conclusions: “Strong primary care system and practice characteristics such as geographic regulation, longitudinality, coordination, and community orientation were associated with improved population health”. The Doha Declaration Nov 2008 The Member States express their highest level of commitment to: • Strengthen the decentralization of the health system • Establish and/or scale up family practice models • Ensure integration of vertical programs into primary health care • Promote healthy lifestyles • Ensure community-oriented training programs for a health workforce with appropriate skills mix • Ensure good remuneration and clear career paths to encourage the health workforce into primary health care; • Expand the role of primary health care workers as community leaders • Strengthen partnership for primary health care between government, civil society, community leaders, academia and the private sector; • Monitor and evaluate health system performance through the development and use of national health information systems and national and regional health observatories • Promote policy and health systems research, community-based participatory research and knowledge translation for evidence-based policymaking. To sum up • ''If we didn't already have primary care medicine, we'd just have to invent it. It's the way we want to be cared for.'' (Allan Goroll)