SuperficialBack.doc
advertisement

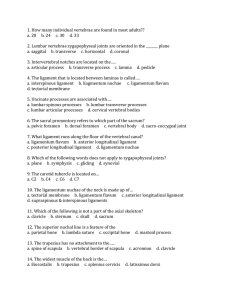
Superficial & Deep Back Tabulae sceleti et musculorum corporis humani. Albinus, Bernhard Seigfried (1697-1770). When you ask a student who has taken a course in human gross anatomy what their favorite part of the body was to dissect, the answer is never the superficial and deep back. While the back may not have the glamour of the head or the uncanny quality of the digestive organs, the function of the back is interesting if you think about it. Let me illustrate. On those friday evenings you spend at your favorite bar looking for that special someone there is a deep evolutionary drive that is at work here weeding out the inappropriate candidates for procreation. Now you may be thinking, “I’m just looking for some fun, who said anything about making babies?” I did. In the following example, tell me which of the following individuals is going to appear more attractive to you. First, a person who sits or stands upright at the bar with their shoulders squared, but still appearing relaxed. Second, a person who is either standing, but leaning on the bar or sitting somewhat slumped on the barstool with their shoulders rounded. Of course you picked the first person after reflecting on the scenario. The muscles found on the superficial and deep back are the ones working to achieve this affect. Well these muscles and a persons self esteem. I would also suggest that the surface of the back has a sexual allure to it as well. As evidence for this statement, consider the one of the many awards shows next time they are on television and count the number of backless gowns worn by the actresses / female singers. These ladies are not wearing gowns like this because it is hot outside. The back also functions as a large palate for the tattoo artist allowing space for a detailed horimono design. Finally, no discussion about the back would be complete without mention of the vertebral column. The vertebral column is interesting to any person who has suffered a herniated disc or knows a person with scoliosis. Chiropractors naturally love spinal anatomy, if not why choose that profession? Inside of the vertebral column you will find the spinal cord and emerging through the intervertebral foramen, individual spinal nerves. Palpation Features: The external occipital protuberance (inion) is in the center of the superior nuchal line and that is the superior attachment of the trapezius muscle. The vertebra prominens (C7 spinous process) is not only palpable, but sometimes visible on a person when viewed from a lateral perspective. The acromion of the scapula is the bony landmark found lateral to the clavicle and is sometimes visible where the trapezius meets the deltoid at the superior aspect of the shoulder. If you follow the acromion in a posterior direction, it continues as the spine of scapula. The inferior angle of scapula is occasionally obscured by the upper border of the latissimus dorsi, but when you find it, it should be in the same horizontal line as the 7th thoracic vertebrae and in the same vertical line as the angle of the ribs. The iliac crests are inferior points of attachment for the latissimus dorsi and are often obscured by the fat of the region commonly called “The muffin top”. If you locate the most superior edge of the left and right iliac crest and imagine a horizontal line running between the two points then that line normally will pass through the space between the 3rd and 4th lumbar vertebrae. The clinical relevance of this is that this is the location a needle is typically inserted to collect cerebrospinal fluid (spinal tap). Note: Keep in mind that even though we don’t dissect the vertebral column you will be responsible for these bones and the ligaments that secure them to one another. The Back: Anatomical borders of “the back” are from the inferior portion of the neck to the buttocks in the vertical plane, and from the angle of the ribs on the left to the angle of the ribs on the right. “The back” is not to be confused with the definition of the back in the Sir Mix-a-lot song “Baby Got Back”, which is clearly a reference to the buttocks. Even a person who is not an anatomist knows this. Neurovascular bundles: What you are seeing here are the branches of dorsal rami along with an artery and a vein. They can be found at regular intervals (superior to inferior) emerging through trapezius and latissimus dorsi just lateral to the vertebral column. If you see branches closer to the midaxillary line, what you are seeing are lateral cutaneous branches of intercostals nerves. And as you may already know, intercostal nerves are branches of ventral rami. Most of the neurovascular bundles are cut when the superficial fascia is reflected, so I add this feature for the occasional times these bundles escape the swipe of the scalpel. Trapezius: One of the superficial back muscles that you may hear being described in a clinical setting in three parts, upper fibers, middle fibers and lower fibers. Although it looks like one muscle when you look at the entire back, keep in mind that the left and right sides have independent innervation, so it is possible to come across a patient with only one side functioning. How might this happen you ask? Lets say we have a patient with cancer that spread into the lymph nodes of the cervical region. If a good but overworked surgeon accidentally cuts the spinal accessory nerve while removing one of these lymph nodes that would be one cause of such a presentation. Figure 1: Left side spinal accessory nerve lesion Spinal Accessory Nerve (CN XI): In this dissection you can find this nerve on the deep surface of trapezius. It emerges from an opening in the inferior portion of the skull called the jugular foramen. It is the motor nerve to this muscle as well as to the sternocleidomastoid, a muscle of the neck. Transverse Cervical Artery: The source of this artery is the thyrocervical trunk. The transverse cervical artery has two parts, the superficial branch (which we see on the deep surface of trapezius) and a deep branch that is also called the dorsal scapular artery. Note that occasionally trapezius receives some of its blood supply from a branch of the suprascapular artery. If such a branch exists in your cadaver it will be cut when you reflect trapezius. Occipital Artery: The source of this artery is the external carotid artery. Like the transverse cervical artery, we can’t see it’s source in this dissection, but should you be wondering where it is coming from, now you know. This artery will be emerging from the area of the mastoid process then ascending the posterior cranium deep to the splenius capitis and superficial to the semispinalis capitis, and piercing trapezius just lateral to the greater occipital nerve. The connective tissue in this area tends to be rather dense and most students will cut the artery along with the greater occipital nerve. So, if you find that you can expose these structures with a minimal amount of damage you should feel pretty good about yourself for today. (You will only be exposing the most superior portion of this artery today, don’t remove musculature inferior to the superior nuchal line except trapezius) Greater Occipital Nerve: Find this nerve piercing the trapezius muscle approximately 3 cm inferolateral to the inion. Recall from lecture the difference between a ventral ramus and dorsal ramus of a spinal nerve. The greater occipital nerve is part of the dorsal ramus of spinal nerve C2. Just as with the occipital artery, please don’t try to dig this nerve out from deep to the muscle today. Hmmm, was it the roots or the rami that allows you to determine the function of a group of neurons? Latissimus Dorsi: While the origin of this muscle should be clearly observable in this dissection, its insertion may not be as obvious at this point. Once you can appreciate the path this muscle follows, its actions on the upper extremity become obvious. So, take note of how the superior portion of this muscle intervenes between the thorax and the arm on its way to the floor of the intertubercular sulcus of the humerus. In today’s dissection you may find that latissimus interdigitates with the external oblique and possibly serratus anterior so be mindful of this when reflecting the muscle. The innervation of the latissimus dorsi is the thoracodorsal nerve. Thoracodorsal nerve: This nerve comes from the posterior cord of the brachial plexus, specifically spinal levels C6-C8. That last sentence may not mean much to you now, but it will in a few weeks. It can be identified as it emerges from the area of the axilla and enters the deep surface of latissimus dorsi. You will see more proximal portions of this nerve when you do the pectoral/axilla dissection. Thoracodorsal artery: This artery is the primary blood supply for latissimus dorsi as you may have guessed. This artery one of the terminal branches of the subscapular artery. What I mean by “terminal branch” is that the subscapular artery bifurcates, meaning instead of giving off any more branches it simply splits into two arteries, like reaching a fork in the road. The other terminal branch (circumflex scapular artery) is discussed in the scapulo-deltoid dissection. Rhomboid Minor & Major: You find these muscles deep to the trapezius securing the scapula to the vertebral column. Note that rhomboid minor attaches at the root of the scapular spine while rhomboid major attaches more inferiorly on the vertebral border of the scapula. Use this information to differentiate one from the other. Both muscles are innervated by the dorsal scapular nerve (C4,C5) which may be seen in this dissection if you are careful not to hack it apart. The dorsal scapular nerve can be found close to the medial border of the scapula traveling from the deep surface of levator scapulae to rhomboid minor then to rhomboid major. The dorsal scapular nerve should lie in close proximity to the artery of the same name. Levator Scapulae: After the rhomboids have been cut from their vertebral attachments, pull the scapula laterally and note how levator scapulae splits into four slips as it approaches its superior attachments. The superior attachments I speak of are the posterior tubercles of the transverse processes of cervical vertebrae 1 – 4. Serratus Posterior Superior & Inferior: These muscles will be tricky to dissect out for two reasons. (1) They are thin flat muscles (2) their fiber orientation matches the muscles superficial to them. Have fun with that. The serratus posterior superior lies deep to the rhomboids while the serratus posterior inferior lies deep to latissimus dorsi. Both are innervated by intercostals nerves. Recall that intercostals nerves are NOT dorsal primary rami. These two serratus muscles are considered to be the intermediate layer of back muscles and you should not include the serratus anterior muscle in this group. Thoracolumbar Fascia: This tissue separates the intrinsic (true) back muscles from the extrinsic back muscles. What you see here is the superficial portion. The deep portion gives attachment to the transversus abdominus and the internal obliques, which will be discussed in the anterior abdominal wall dissection. Cut the superficial portion close to the vertebral column in the lumbar region and reflect it laterally when you want to begin exposing the true (deep) back muscles. Erector Spinae: These muscles can be divided into three columns from lateral to medial they are iliocostalis, longissimus, and spinalis. The columns can be separated and differentiated by running the fingertips between them. Multifidus Muscles: These muscles help to stabilize the spine and are part of the transversospinalis group. Note the “up and in” orientation of the muscle fibers making them contralateral rotators when contracting unilaterally. Multifidus gets its name from the Latin terms multus, many + findere, to split, which gives us divided into many sections. An appropriate name for a muscle that travels up the entire vertebral column (Sacrum to C2) with the longest fibers spanning only 4 vertebrae. You will have to move the erector spinae muscles laterally to view the multifidus. Anterior Longitudinal Ligament: Attaches superiorly at the basilar part of the occipital bone and extends inferiorly, superficial to the vertebral bodies, to the anterior portion of the upper sacrum. This ligament is most adherent to the intervertebral discs, hyaline cartilage and vertebral end plates. It is more loosly attached (by comparison) to the vertebral bodies themselves. Posterior Longitudinal Ligament: Found on the posterior surface of the vertebral bodies C2 (superiorly) to the sacrum (inferiorly). Between C2 and the occipital bone this ligament blends with the cranial dura to form the tectorial membrane. This ligament is broad and more uniform in width through the cervical and thoracic regions while in the lumbar spine it narrows as it crosses the vertebral bodies and widens as it crosses the IV discs. This makes sense as this allows the ligament to help prevent posterior herniation of the nucleus pulposis, which would compress the spinal cord or cauda equina. Apical ligament: Spans the distance between the superior aspect of the dens and the anterior aspect of the foramen magnum. This is separate / distinct from both anterior and posterior longitudinal ligaments. Alar Ligaments: This pair of ligaments attach to the postero-lateral aspects of the dens to the medial sides of the occipital condyles. (One on the left and one on the right, just so that we are clear). Functionally, they are thought to limit the amount of rotation between the atlas and the axis. Then why don’t they attach to the atlas you may be thinking? Well, the atlas and the cranium rotate more as a single unit on the dens than as two separate parts. Anterior and posterior atlanto-occipital membranes: While the anterior atlanto-occipital membrane somewhat blends with the anterior longitudinal ligament, the posterior atlanto-occipital membrane does not blend with the posterior longitudinal ligament. The posterior atlanto-occipital membrane will be removed to expose the vertebral artery in dissection 2, suboccipital region. Some Clinical Curiosities… Rhomboid of Michaelis: This anatomical region on females can be used to get a rough estimate of the dimensions of the birth canal. Named for gynecologist G.A. Michaelis, the boundaries for this landmark are the left and right PSIS, the spinous process of L4 vertebrae, and the upper part of the natal cleft. In a normal female, the vertical and horizontal dimensions of this rhomboid are roughly equal. While I can find several references for this landmark, its obstetric utility is virtually non-existent in the literature. The Rhomboid of Michaelis will not be on the exam, I include it because sometimes the history of medicine can be interesting. (Fig. 4.2) Triangle of Auscultation: Found between the medial border of the scapula, upper border of latissimus dorsi, and the inferior/lateral border of trapezius. This puts you superficial to the sixth intercostals space. In this triangle there is a minimal amount of superficial tissue and therefore an ideal place to position a stethoscope to listen to the lungs. It is common to hear this in most clinical settings. On a fit individual, you should be able to find this landmark with some ease. In a more sedentary person you just have to ballpark the area. To increase the size of the sixth intercostal space, have the patient flex forward with both arms folded across the chest. Lumbar Triangle (of Petit): Inferiorly bordered by the iliac crest, medially by the latissimus dorsi and laterally by the external abdominal oblique. While it is a rare occurrence, this may be the site of a hernia (lumbar hernia). Jefferson (Burst) Fracture: Classically described as a fracture of 4 parts of the atlas resulting from a compression force delivered through the axial skeleton by way of the head. Example, diving head first into the shallow end of a swimming pool. If you look at the coronal section of the craniovertebral and atlantoaxial joints you can see how a compression force delivered through the head would effectively drive the two lateral masses of the atlas in opposite directions. This of course a result of the orientation of the facet (zygopophyseal) joints. One of the real dangers here is a rupture of the transverse ligament that secures the dens to the atlas. If this ligament is ruptured there is a possibility of compressing the spinal cord within the vertebral canal. (illustration below) A B C A: inferior portion of occipital bone B: atlas (C1) C: axis (C2) Figure 2: MRI Jefferson Burst Fracture