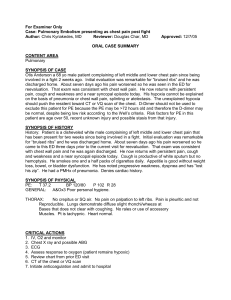
Patient with pleuritic chest pain
advertisement
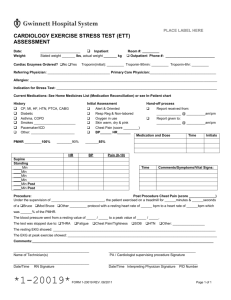
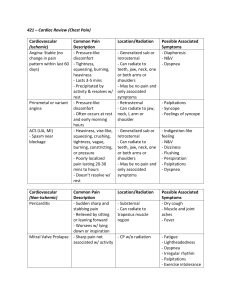
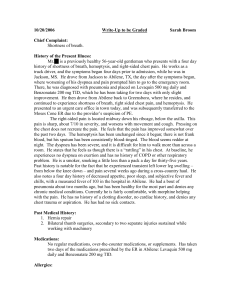
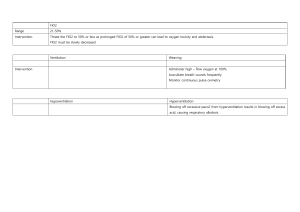
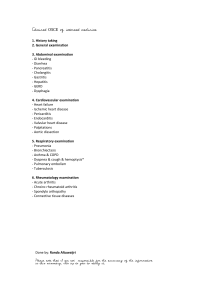
A Patient with Pleuritic Chest Pain and Dyspnea A 63-year-old woman is admitted to the hospital because of acute dyspnea and right sided chest pain. She has a long history of medical problems including hypertension, and insulin dependent DM and chronic kidney disease. She sustained an inferior-lateral wall transmural myocardial infarction 5 years ago with a residual left ventricular ejection fraction of 30%. Three years ago, she underwent a left mastectomy for breast carcinoma and completed 6 months of adjuvant chemotherapy because of tumor involvement in 3 axillary lymph nodes (hormone receptors were negative). She had been feeling relatively well lately until the day of admission when she noted the acute onset of dyspnea in the morning. This progressed throughout the day and was associated with pain in her right chest that increased upon inspiration, so she came to the Yale Emergency Department. She denied fever, cough, headache, abdominal pain, back pain, or light headedness. Her medications include insulin, Lasix, Lopressor, and an ACE-inhibitor. PE reveals a dyspneic obese woman. T 99.4, R 32, P 120, BP 130/84. SKIN - no rash or lesions. LN - none palpable. HEENT - conj pink; Fundi - background but no proliferative retinopathy; oropharynx benign. CHEST - clear; mastectomy scar healed. COR - RRR without murmurs or rub. ABD - obese, soft, nontender without hepatosplenomegaly. NEURO - normal. EXT – benign without edema or erythema. LABS Na 136, K 3.0, Cl 99, HCO3 24, Cr 1.7, glu 160 Hb 14.0, Hct 42.1, WBC 12.2 (normal differential), plts 375K UA: clear/1.016/2+ protein/2+ glucose/no ketones, cells or casts EKG: Stach 120/ Q waves in II, III, avF, V4-6; no change from recent EKG CXR: clear lungs, normal heart size ABG (room air) pH 7.52/pCO2 22/pO2 51 1. What would be your differential diagnosis of this patient’s presentation and what would be your leading concern? 2. What are the most common risk factors predisposing patients to pulmonary embolism? Which ones are most relevant to this patient? 3. What diagnostic tests would you perform to assess the possibility of pulmonary embolus? Describe the advantages and disadvantages of each. Rev 2-2011 4. The intern orders a ventilation-perfusion scan which is read as “high probability”. What acute therapy would you choose and what benefit does it provide to the patient? 5. What would be your approach to long term management? . Rev 2-2011