CASE STUDIES OF PRACTICE: PHYSICS Title of Practice: Practice Placements
advertisement

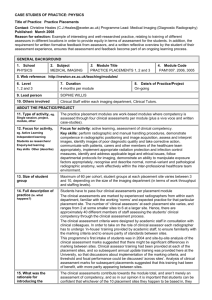
CASE STUDIES OF PRACTICE: PHYSICS Title of Practice: Practice Placements Contact: Christine Heales (C.J.Heales@exeter.ac.uk) Programme Lead: Medical Imaging (Diagnostic Radiography) Published: March 2008 Reason for selection: Example of interesting and well-researched practice, relating to training of different assessors in different locations in order to provide equity in terms of assessment for the students. In addition, the requirement for written formative feedback from assessors, and a written reflective overview by the student of their assessment experience, ensures that assessment and feedback become part of an ongoing learning process. GENERAL BACKGROUND 1. School PHYSICS 2. Subject MEDICAL IMAGING 3. Module Title PRACTICE PLACEMENTS 1, 2 and 3 4. Module Code PAM1007. 2006, 3005 5. Web reference: http://newton.ex.ac.uk/teaching/modules/ 6. Level 1, 2 and 3 7. Duration 4 months per module 8. Date/s of Practice/Project On-going 9. Lead person SOPHIE WILLIS 10. Others involved Clinical Staff within each imaging department, Clinical Tutors. ABOUT THE PRACTICE/PROJECT 11. Type of activity, eg. Single session, project, module, other 12. Focus for activity, eg. Active Learning Independent learning Students as researchers/ Enquiry-led learning Key skills Other (describe) The practice placement modules are work-based modules where competency is assessed through four clinical assessments per module (plus a viva voce and written case-studies). Focus for activity: active learning, assessment of clinical competency. Key skills: perform radiographic and manual handling procedures, demonstrate competence in radiographic positioning and image acquisition, assess and interpret images, identify images of poor diagnostic quality and take corrective action, communicate with patients, carers and other members of the healthcare team appropriately, implement appropriate radiation protection and infection control measures, identify and address applicable legal and ethical issues, follow departmental protocols for imaging, demonstrate an ability to manipulate exposure factors appropriately, recognise and describe normal, normal-variant and pathological radiographic anatomy, work effectively within the inter-professional healthcare team environment. 13. Size of student group Maximum of 60 per cohort, student groups at each placement site varies between 3 and 10, depending on the size of the imaging department (in terms of work throughput and staffing levels). 14. Full description of practice (ie. what Students have to pass four clinical assessments per placement module The clinical assessments are marked by experienced radiographers from within each department, familiar with the working ‘norms’ and expected practice for that particular placement site. The number of ‘clinical assessors’ at each placement site varies, and ranges from 2 at some smaller sites to 6 at a larger site. Hence, there are approximately 40 different members of staff assessing the students’ clinical competency through the clinical assessment process. The clinical assessment criteria were designed by academic staff in consultation with clinical colleagues. In order to take on the role of clinical assessor each radiographer has to undergo ‘in-house’ training provided by academic staff, to ensure familiarity with the marking criteria and to ensure parity of standards between sites. This programme’s first intake of students was in 2004 and site-by-site analysis of the clinical assessment marks suggested that there might be significant differences in marking between sites. Clinical assessor training had been provided at each of the placement sites, and so subsequent annual update training was provided here at the University, so that discussions about implementation of the marking criteria, and threshold and focal performance could be discussed ‘across sites’. Analysis of clinical assessment marks for subsequent placements suggested that this training had been of benefit, with more parity appearing between sites. happens?) 15. What was the rationale for introducing the The clinical assessments contribute towards the module total, and aren’t merely an assessment of competency, and so in our opinion it is important that students can be confident that whichever of the 10 placement sites they happen to be based in, they practice? will be assessed appropriately. 16. Resources/support required (technical The Clinical Placement Co-ordinator and the Programme Lead for the BSc (Hons) Medical Imaging (Diagnostic Radiography) programme provide 2 training days for the clinical assessors here at the University. The same training programme is provided at both sessions, so that clinical assessors need only attend one of the 2 per year. The reason for running the same session twice is that clinical departments can only release a limited number of staff from the clinical area on any given day. Hence this approach enables more staff from each department to be able to attend within the 12month period. assistance, specialised equipment etc) ASSESSMENT 17. Assessment Students have to pass four clinical assessments per placement module. Each clinical assessment contributes 10% towards the module total, but each clinical assessment must be passed at a threshold of 40% as well as obtaining 40% for the module overall in order for the credits to be awarded. Condonement is not permitted on this programme. 17c. Assessment criteria (web link if http://newton.ex.ac.uk/handbook/Rad-ClinAssmntL123MC.html http://newton.ex.ac.uk/handbook/forms/ClinAssmntL12.pdf NB: There are other clinical assessment forms for specific examinations undertaken in stages 2 and 3. - Students are expected to provide a verbal commentary throughout the clinical assessment to demonstrate their understanding of, and compliance with, safe competent practice. - Detailed marking of competences is accompanied by a requirement for formative feedback for the student relating to strengths and areas for future improvement (see p.9 of the Clinical Assessment form) - The student is also required to write reflective comments on their assessment (see p.10 of the same form): Did any of the assessor’s comments surprise you? Where you expecting any of these comments? How will you use these comments to develop your practical radiographic ability? What did you gain from this experience? What did you do well? What could you have done better? How will you future practice change as a result of this assessment? available) FEEDBACK 18a. Feedback Student comments Questions relating to the marking of the clinical assessments have recently been added to the students’ placement feedback forms as follows: Q: Feedback from each clinical assessment was sufficient for me to understand why I was awarded a particular mark Q: My clinical assessments were marked fairly i.e. by comparing my performance to the applicable marking criteria. For the two placements since these questions have been added, the majority of students have indicated that they agree or strongly agree with the above questions, suggesting that concerns previously indicated in the free-form student feedback comments about the parity of marking have been allayed. PAM1007 _Academic Year 2006-7_ Student Feedback.pdf 18b. Feedback – Staff comments OTHER MATTERS Informal feedback at the assessor days has suggested the value of facilitating crosssite discussion relating to the clinical assessment process. 19. Issues/difficulties encountered Cross-site training provides a burden on placement sites as they have to release staff from clinical duties in order to attend. However, our clinical sites have been hugely supportive and are continuing to facilitate staff attendance. Clinical Asse ssors Clinical Assessors Update Training - Update OctoberTraining 2006.doc - July 2006.doc There are also financial implications as we provide catering and also pay the travel expenses of clinical staff attending training here at the University. The clinical assessment process will always require continuous modification to reflect changing clinical practice, and so on-going training and support for clinical assessors is essential.