Community Acquired Pneumonia (CAP) Last revised January 2016 by Michelle Le
advertisement

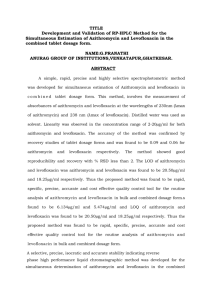
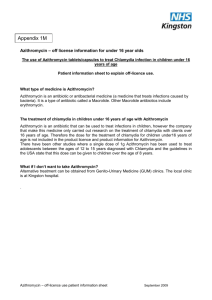
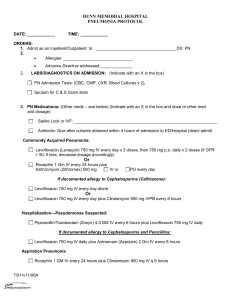
Community Acquired Pneumonia (CAP) Last revised January 2016 by Michelle Le Objectives • Diagnosis of CAP • Level of care assessment • Therapeutic recommendations Case Vignette A 68 y/o Vietnamese male presented to the ED with SOB and productive coughing for 2 days. Reports poor oral intake since onset due to nausea and intermittent vomitting. His wife had similar symptoms 1 week ago which improved with an unknown antibiotic. Patient is requesting to go home with antibiotic. He previously had tongue swelling and skin rash with use of augmentin. Reports good health otherwise so he has not seen his PCP for past 5 years. Denies chest pain, swelling of extremities, or diarrhea. His vital signs are T 38.5 C, P 76, BP 128/82, spO2 94%, RR 16. Patient is alert and oriented. Crackles were heard over left lower lung field. Labs showed WBC 14, BUN 20 mg/dL. Chest X-ray had a consolidation in left lower lobe. Case Vignette What is the best way to further manage this patient? A. Send home with oral azithromycin B. Send home with oral levofloxacin C. Admit to medicine floor with iv levofloxacin D. Admit to medicine floor with iv ceftriaxone and po azithromycin E. Admit to ICU with iv ceftriaxone and iv azithromycin Don’t worry... We will revisit this case at the END of our mini-lecture! Definitions – Pneumonia (PNA) • Community acquired PNA (CAP) – Infection of lung parenchyma in pt who is not hospitalized or living in a long-term care facility for ≥2 weeks • Hospital-acquired PNA (HAP) – Occurs ≥48 hours after admission; not intubating on admission • Healthcare-associated PNA (HCAP) – Non-hospitalized pt with extensive healthcare contact and ≥1 criteria from below: • • • • IV therapy, wound care, or IV chemotherapy within the prior 30 days Residence in a nursing home or other long-term care facility Hospitalization in acute care hospital for ≥2 days within the prior 90 days Attendance at a hemodialysis clinic within the prior 30 days • Ventilator-associated PNA (VAP) – Arises >48-72 hours after endotracheal intubation Severity of PNA • Severity-of-illness scores can help guide whether a pt needs hospital admission and should always be supplemented with clinical judgement • CURB-65 criteria – – – – – – Confusion Urea >19 mg/dL Respiratory rate ≥30 Blood pressure (SBP <90 or DBP ≤60) ≥65 year old ≥2 criteria then needs hospital admission and ≥3 criteria may need ICU level of care • Can also use Pneumonia Severity Index (PSI) instead of CURB-65 CAP Pathogens CAP Treatment - Outpatient • No comorbidities or recent antibiotics use 1st line: azithromycin (Z-Pak) 2nd line: doxycycline • Have comorbitidies or antibiotic use in last 3 months Preferred: moxifloxacin OR levofloxacin Alternative: augmentin + azithromycin CAP Treatment - Inpatient • Non-ICU moxifloxacin OR levofloxacin azithromycin + [unasyn OR zosyn OR ceftriaxone OR meropenem] • ICU Preferred: azithromycin + [unasyn OR zosyn OR ceftriaxone OR meropenem] Alternative: moxifloxacin OR levofloxacin • If has PCN allergy aztreonam + [moxifloxacin OR levofloxacin] Case Vignette A 68 y/o Vietnamese male presented to the ED with SOB and productive coughing for 2 days. Reports poor oral intake since onset due to nausea and intermittent vomitting. His wife had similar symptoms 1 week ago which improved with an unknown antibiotic. Patient is requesting to go home with antibiotic. He previously had tongue swelling and skin rash with use of augmentin. Reports good health otherwise so he has not seen his PCP for past 5 years. Denies chest pain, swelling of extremities, or diarrhea. His vital signs are T 38.5 C, P 76, BP 128/82, spO2 94%, RR 16. Patient is alert and oriented. Crackles were heard over left lower lung field. Labs showed WBC 14, BUN 20 mg/dL. Chest X-ray had a consolidation in left lower lobe. Case Vignette What is the best way to further manage this patient? A. Send home with oral azithromycin B. Send home with oral levofloxacin C. Admit to medicine floor with iv levofloxacin D. Admit to medicine floor with iv ceftriaxone and po azithromycin E. Admit to ICU with iv ceftriaxone and iv azithromycin Case Vignette What is the best way to further manage this patient? A. Send home with oral azithromycin B. Send home with oral levofloxacin C. Admit to medicine floor with iv levofloxacin D. Admit to medicine floor with iv ceftriaxone and po azithromycin E. Admit to ICU with iv ceftriaxone and iv azithromycin Summary • CAP: infection of lung parenchyma in pt who is not hospitalized or living in a long-term care facility for ≥2 weeks • CURB-65 and Pneumonia Severity Index (PSI) are severity-ofillness scores which help guide level of care in conjuction with clinical judgement • Appropriate antibiotic regimen will provide coverage for both Strept pneumoniae and atypical pathogens References • Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 2007; 44 Suppl 2:S27. • American Thoracic Society, Infectious Diseases Society of America. Guidelines for the management of adults with hospitalacquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 2005; 171:388. • Schuetz P, Christ-Crain M, Thomann R, et al. Effect of procalcitonin-based guidelines vs standard guidelines on antibiotic use in lower respiratory tract infections: the ProHOSP randomized controlled trial. JAMA 2009; 302:1059.