Pearls for Interns UCI Internal Medicine Residency
advertisement

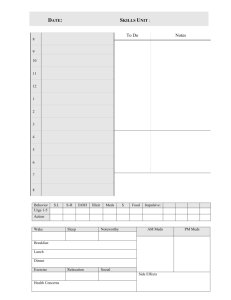
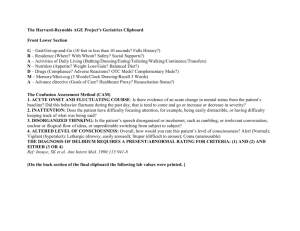
Pearls for Interns UCI Internal Medicine Residency Things to Do in AM As you drive in to work, think about pending issues from yesterday and potential discharges Pick up your sign-out from the overnight night float/team. Let senior know of anything urgent/major changes check vitals, I/O check labs, REPLETE LYTES AS YOU CHECK LABS so you don't forget check telemetry – think about D/C telemetry if no longer indicated See your patients. While seeing them, see how much of prn meds were used (i.e. pain meds, insulin sliding scale) etc. For ICU, determine doses of all pressors currently running. check if your patient has the following: 1) Foley. Does it need to be in? 2) Central line. Does it need to be in? 3) IV Fluids. Does the rate need adjustment? *** Are the fluids appropriate? Run through the list with senior resident for assessment/plan for your patients At UCI - have blue progress notes filled out at UCI (see next slide) Rounds – keep checklist of stuff to do on scut sheet, with checkboxes Progress Notes - UCI Check with your Attending on preference for billing (Attending charts entire note vs Attending writes Attestation statement for combined Resident/Attending note.) SOAP Format S: Includes Chief Complaint, HPI, and ROS Do NOT chart PE (except vitals) if the Attending does not want to write Attestation Chart static data (relevant medications, vitals, pertinent lab or radiology results, pulse ox, test results) A/P: Includes Dx or symptom, type or Stage, acuity or severity, & etiology if applicable (example: Chronic microcytic anemia due to menorrhagia; DM II, uncontrolled, etc.) Do NOT chart S: if the Attending does not want to write Attestation If charting, include as many of the 7 dimensions of chief complaint as appropriate and overnight events. If pt unable to give history, mention why (i.e. intubated/sedated). O: Includes Medications, PE, Lab or Radiology results, Pulse Ox, Telemetry, EKG, Dx test results Students (including sub-I’s) should only chart static data (see below) or write a separate blank Blue Note progress note (not the Hospitalist PN) and have Resident or Attending co-signature Do NOT chart A/P if the Attending does not want to write Attestation NEVER chart “FEN,” instead “dehydration” or “hypokalemia,” or “malnutrition.” Use a Dx. NEVER chart “PPx,” instead “risk for DVT due to cancer” or “risk for GI bleed due to steroid” All notes with Attending Attestation also require a Resident signature, printed name, date, and time After Rounds 1. 2. 3. 4. 5. 6. 7. Run the list with senior resident to confirm things to do Put in the most important orders from rounds first (i.e. antibiotics, imaging, time-critical IR procedures) Call consults: know your question is & what you want answered Work on discharges and sick patients first. For discharges, set up discharge meds/prescriptions for the patients, ensure patient has ride home, discuss dispo issues (i.e. transportation) with case management EARLY. Noon Conference Afternoon: continue work, F/U Consults. Run the list. Update signout. Can start on discharge summaries for future discharges. Do not enter anything in the DC summary which has not yet occurred (i.e., condition at discharge, discharge date, etc). Anticipate care path requirements for CHF, pneumonia and MI. i.e. for CHF pts, are they on all the correct medications? Sign-Outs Before sign-out: Highlight key parts of patient’s hospitalization and active issues Renew all orders that need renewal (IV fluids, restraints, Abx, etc.) Order AM labs if indicated Review sign-out with senior Resident or your Attending Anticipate what on-call Resident may get called about Try to avoid signing out things to do that aren’t absolutely necessary (i.e. will not change management overnight). Common things to sign out (to get an idea): - check H/H if pt bleeding - check lytes, I/O if pt being diuresed - checking cardiac enzymes/EKGs - F/U on critical imaging studies management Carefully sign out what to do with if-then scenarios, especially for sick/dying patients. Include things like OK for ICU transfer, DNR/DNI, calling consultants if this happens etc. - common overnight calls: pain control, fever Admissions First eyeball the patient and vitals to make sure they’re stable If patient appears unstable or has critical labs (especially ICU patients), address those first. Then quickly read through the patient’s chart (prior H&Ps and discharge summaries are key) before doing the full interview (this may make the interview more efficient). Don’t forget to get the name and number of pt’s PCP. Don’t forget Code Status HPI should be structured in three parts: 1) Introductory statement with patient’s age and pertinent presenting info relating to chief complaint 2) The HPI consisting of 7 dimensions of the chief complaint 3) List of what was done in ED For physical exam: - don’t forget rectal exam in any patient with GI bleed or anemia - don’t forget orthostatic vitals in patients with GI bleed, syncope etc For abnormal labs, look back to see what the pt’s baseline is Admissions Cont Print/make copy of EKG to keep with you After interviewing/examining the patient: - present the pt to your senior resident and formulate a plan. Make list of orders. - put in patient’s orders first, starting with the most critical Don’t forget AM labs. Review the routine (AM) labs; you probably don’t need to order most of them. - call consultants (check with your senior first) - after all of the above is done, THEN write the H&P When presenting new patients: have all the details, but make your presentation pertinent. H&P should be presented within 5-10 min. First present the H&P, then summarize 24 hr events and progress note from today (i.e. today’s subjective, vitals, labs, imaging). Discharges Anticipate discharge needs and speak with case managers ahead of time. Examples: - equipment: walkers, bedside commodes, etc - meds: IV abx, coumadin clinic, glucometers, Lovenox etc - follow-up appointments (done by case managers at UCI) - placement: SNF, board & care, hospice, referral to drug rehab transportation home Think of things holding pt in hospital: alimentation (nutrition), elimination (Foley, bowel obstruction), ambulation (independence), and oxygenation Convert IV meds to po; wean off oxygen if possible When discharge is planned, notify pt/family for transportation Reconcile patient’s medications and write new Rx Notify nurse of discharge Write D/C Instructions, Summary, enter d/c order At End of Day Don’t forget to ask yourself: 1) Did you place am lab orders? Do you really need those labs? 2) NPO past midnight for procedure in am? Did I adjust the diabetes meds and IV fluids when I made the patient NPO? 3) Held antiplatelet drugs or anticoagulants for future procedure? 4) Checked charts for recs from consultants, and entered those orders? 5) Restarted diet after patient has returned from procedure? Tips on medication orders: For all anti-hypertensive meds, always write hold parameters for the RNs. i.e. hold for systolic blood pressure <100. For beta blockers, include heart rate parameter i.e. HR <55 For septic/hypotensive patient, consider discontinuing all BP meds rather than relying on hold parameters For all topical meds, write what part of the body to apply it to, and in what amount (i.e. left arm thin film) For all prn meds, must specify the prn indication (i.e. prn constipation, nausea, anxiety etc) For prn narcotic pain meds, must specify severity of pain (i.e. prn severe pain). - consider using dilaudid in patients with impaired renal function (other narcotics have more renal excreted metabolites and therefore their narcotic effect may be more pronounced or linger) Tips on Meds cont For all meds, always ask yourself if the pt has any contraindications to it before you click the "submit" button. This is a good way to learn contraindications. Some common ones to watch for: heparin: bleeding/peptic ulcer, history of heparin induced thrombocytopenia. Consider holding before any procedures/surgery H2 blocker – thrombocytopenia Statin + plavix (statin may decrease plavix concentration; don’t change a stable dose unless cardiology approves) lovenox – renal failure ACE inhibitor – hyperkalemia with acute renal failure NSAIDs – risk of GI bleed, renal failure Acute liver injury – statin Coumadin – bleeding/peptic ulcer, risk of falls (elderly). Consider holding before any procedures/surgery Tips on Meds Cont A few meds to watch out for that have extensive renal clearance or can make AKI worse, so dose must be adjusted or stopped if the patient is admitted with AKI or develops it in the hospital: ACE inhibitors/ARBs – monitor for hyperkalemia atenolol lovenox ***insulin – watch out for this one!!! vancomycin NSAIDs aminoglycosides narcotic pain meds, except dilaudid and fentanyl Common Meds that Need Levels Checked Vancomycin Digoxin Aminoglycosides Valproic acid Carbamazepine FK506 (Tacrolimus) Tips on IV Maintenance Fluids: Be careful giving IV fluids to pts with: CHF, renal failure, ascites. Can cause pulmonary edema or increased ascites. Selecting what IV fluids to use: Dehydrated: Use NS for bolus or maintenance until euvolemic Metabolic acidosis or hyperchloremia: Use LR Maintenance or volume overload: Use ½ NS or D5W (preferred for CHF, renal failure, hepatic failure) Lack of nutrition source: add dextrose (D5 or D10 if volume overload) Dextrose should be added to IVF for diabetics who are NPO and treated with long-acting insulin, even if hyperglycemic. Calling Consults When calling a consultant, have the patient’s H&P and labs handy to answer any questions. Have a specific question in mind and ask it early on in the conversation. i.e. “We are requesting a GI consult on Mr. Doe to determine if he needs an inpatient colo with his degree of iron deficiency anemia. He is a 68 y/o man with…” Specify how urgent the consult request is. Calling consults cont Anticipate information that the consultant will require over the phone and make sure you have it ready. Common consults: GI bleed: vitals, rectal exam, hemoglobin, whether the patient is iron deficient, coags, last EGD/Colo + results, hx of liver disease/PUD, any anticoagulants ID consult: vitals/fever curve, WBC, results of all cultures, how many bottles positive (i.e. 1 of 2), any central lines, what antibiotics/when started AKI: baseline creatinine, prerenal risks (CHF, n/v/d), ins/outs, urinary obstruction, post-void residual, BPH, recent antibiotics (especially aminoglycosides), recent iodine contrast for CT scans GI Prophylaxis Overt GI bleed incidence 1.5-8.5% in all ICU patients, up to 15% with no ppx Up to Date, after review of the literature, suggests GI ppx for all ICU pts at high risk for bleeding, including patients with any of the following: Coagulopathy (platelets <50K, INR >1.5, or PTT >2 times control) - odds ratio 4.3 Mechanical ventilation for >48 hours - odds ratio 15.6 History of GI ulceration or bleeding within the past year Traumatic brain injury, traumatic spinal cord injury, or burn injury Two or more of the following: sepsis, ICU >1 week, occult GI bleeding for ≥6 days, or steroid therapy (> 250 mg hydrocortisone or the equivalent). H2 blocker vs PPI probably equal, some studies show oral PPI most cost effective Recommend to use PPI instead of H2 blocker if pt has thrombocytopenia Consider GI prophylaxis for patients on steroid therapy Remember to D/C prophylaxis when no longer indicated (not in ICU, off steroids, etc) DVT Prophylaxis Strong risk factors (odds ratio >10) - Fracture (hip or leg) - Hip or knee replacement - Major general surgery - Major trauma or spinal cord injury Moderate risk factors (odds ratio 2–9) - Arthroscopic knee surgery - Central venous lines - Malignancy or chemotherapy - Congestive heart or respiratory failure - HRT or OCPs - Paralytic stroke - Postpartum - Previous DVT - Thrombophilia Circulation. 2003;107:I-9 Weak risk factors (odds ratio <2) - Bed rest >3 days - Immobility due to sitting (e.g. prolonged car or air travel) - Age >40 - Laparoscopic surgery - Obesity - Antepartum - Varicose veins Use the Admission VTE order set in Quest (click to fully expand) to guide appropriate prophylaxis Miscellaneous Pearls HTN patient running chronically high --> don't drop BP too fast Usually hold oral anti-glycemics on admission and prior to surgery, especially metformin Obtain blood/urine cultures before giving antibiotics Patient admitted for any reason: if they have significant EtOH history, consider withdrawal risk and doing seizure/DT precautions or order CIWA protocol in Quest Patient admitted for any reason: if they have significant history of steroid use, be careful for adrenal insufficiency if stopping steroids after more than 3 week course, or if patient has increased need for steroids (i.e infection) Avoid beta blockers with no alpha blockade in a cocaine user. Use alpha blockers instead. Miscellaneous Pearls Cont Transfusion time for packed RBCs should be no faster than 2 hours per unit (unless acutely bleeding) as it increases risk of transfusion reaction Consider obtaining head CT prior to LP to assess for increased ICH Watch insulin dosing if patient is NPO risk hypoglycemia In ICU, be careful with using propofol continuously for >72 hours (risk of pancreatitis) Patients who have small bowel obstruction: remember to convert PO meds to IV when possible Every patient on narcotic pain meds should have bowel prophylaxis for constipation. Senna works well. Can order it as standing dose instead of prn and write “hold for diarrhea”