How to approach the patient in shock Payam Parvinchiha, MD
advertisement

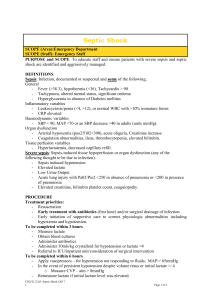
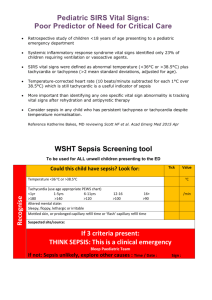
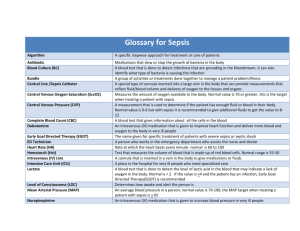
How to approach the patient in shock Payam Parvinchiha, MD Internal Medicine Chief Resident July 2014 Case 1, Part 1 It’s your first day on wards. You get a page “patient’s BP is 80/40.” •When are you going to see the patient? •What questions do you want to ask? •What are some orders to consider? Learning Objectives 1. Approach to the patient with shock Physiology Pathophysiology Physical exam 2. Recognize Shock 3. Differentiate b/w SIRS, Sepsis, & Septic Shock 4. Lactate levels and mortality in sepsis 5. Implement Early Goal Directed Therapy Blood Pressure Physiology • Mean arterial blood pressure – MAP = CO x SVR – MAP = 1/3 SBP + 2/3 DBP – MAP goal is to maintain perfusion of the vital organs – MAP goal is dependent on patient’s individual physiology • Cardiac Output – CO = HR x SV Physiologic Approach: MAP= CO x SVR – Low CO, High SVR • Cool extremities, slow capillary refill • Cardiogenic, Tamponade, Pulmonary Embolus, Tension pneumothorax, and Hypovolemic shock • Very late septic shock – High CO, Low SVR • Wide pulse pressure, warm extremities, normal capillary refill • Early septic shock, adrenal insufficiency, anaphylaxis, neurogenic, thyroid storm, AV fistulas Hypotension vs. Shock • Hypotension is an abnormal vital sign • Shock is a physiologic state defined by vital organ hypoperfusion • Not everyone with hypotension is in shock • Not everyone in shock is hypotensive • By evaluating and treating hypotension EARLY, you can prevent progression to shock Etiologies of Shock CATEGORY PHYSIOLOGY ETIOLOGIES Hypovolemic Decreased venous return Blood loss Fluid loss Cardiogenic Cardiac pump failure/Low CO Left/Right Ventricular failure Valvular dysfunction Arrhythmia Distributive Decreased SVR (Vasodilated) Anaphylactic (FFP) Adrenal insufficiency Neurogenic Obstructive Extra-cardiac obstruction to blood flow Tamponade Pulmonary Embolus Tension Pneumothorax Septic Sepsis Case 1: Part 1 It’s your first day on wards. You get a page “patient’s BP is 80/40.” •When are you going to see the patient? •What questions do you want to ask? •What are some orders to consider? When do you evaluate the hypotensive patient? Immediately I will be there in 1 minute Questions to ask yourself • Is patient symptomatic – delirium, dyspnea, chest pain, oliguria, bleeding, vomiting, diarrhea • Why is patient in hospital • Vitals: Temp, HR, RR, pulse ox, prior BP • Meds: Antibiotics/Blood pressure • Recent procedures – endoscopy, cardiac catheterization, IR procedures, surgery • How much IVF has been given and did they respond Orders to consider as you head over to see the patient • • • • • • • CBC, CMP Lactate, troponin Urinalysis, Urine Culture, Blood Cultures ABG/EKG/CXR Cortisol level/ACTH stim test IVF/Blood Transfusion Grab the bedside ultrasound Case 1, Part 2 Bedside, the patient is lethargic and unable to speak and there is no family at bedside What constellation of physical exam signs can help you narrow you differential diagnosis? Helpful physical exam findings • GEN: Delirium, confusion, lethargy, accessory muscle use • HEENT: Dry mucous membranes • CV: Jugular venous distension/flattening, murmurs, extra heart sounds, irregular tachycardia? • Lungs: Asymmetric hemi-thorax, rales or other abnormalities • Abdomen: Absent bowel sounds, distension, rebound – Palpate the back, groin, and thigh • Extremities: edema • Skin: Pallor, cyanosis, capillary refill, warm or cold Case 1, Part 3 • • • • • • • • • • • • Patient admitted earlier today for confusion Vitals: 39 C, HR 130, RR 22, BP 80/40, 98% RA, Confused Dry mucous membranes Symmetric, CTAB S1 S2 regular tachycardia Cool extremities Abd Soft, mildly distended, nontender, few bowel sounds CVA tenderness on Right UA: 200 WBC and few bacteria Urine output 10cc/hr WBC 25,000 Definitions of SIRS/Sepsis • Bacteremia: Positive Blood Cultures • SIRS: 2 or more – T <36 or >38 – HR >90 – RR >20 – WBC <4000 or >12000 or 10% bands • SEPSIS: SIRS that has proven or suspected microbial etiology • SEVERE SEPSIS: Sepsis induced tissue hypoperfusion with organ dysfunction • SEPTIC SHOCK: Sepsis with hypotension despite adequate fluid resuscitation or vasopressors needed to maintain SBP >90 or MAP >65 What defines severe sepsis vs sepsis? Tissue hypoperfusion • • • • • • • • Elevated lactate Urine output <30cc/kg – foley Acute kidney injury Elevated troponins Transaminitis Altered mental status, chest pain Ischemic bowel gangrene SIRS and SEPSIS Lactate and Mortality in Sepsis • Optimizing Oxygen delivery to the vital organs. • O2 delivery = CO x 1.34 x Hb x %O2 saturation • Serum Lactate: biochemical evidence of suboptimal tissue O2 delivery Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock Figure 3. Association between serum lactate level and 28-day mortality, stratified by the presence of shock. Serum lactate categorized as follows: low = 0-1.9 mmol/L, intermediate = 2-3.9 mmol/L high = 4 mmol/L. Critical Care Medicine. 37(5):1670-1677, May 2009. DOI: 10.1097/CCM.0b013e31819fcf68 © 2009 by the Society of Critical Care Medicine and Lippincott Williams & Wilkins. Published by Lippincott Williams & Wilkins, Inc. 2 Surviving Sepsis Campaign • 1. Goal-oriented hemodynamic resuscitation • 2. Cultures (Blood, Urine, CSF, etc) – Before antibiotics if does not delay antibiotic administration by more than 45 minutes • 3. Antimicrobial antibiotics in the first 1 hour of recognizing severe sepsis or septic shock • 4. Check lactate in first 3 hours • 5. Source control of infection Hemodynamic Resuscitation It’s all about optimizing Oxygen delivery to the tissue. MAP = CO x SVR CO = HR x SV O2 delivery = CO x 1.34 x Hb x %sat O2 Early Goal Directed Therapy • Early hemodynamic resuscitation in the first 6 hours based on CVP, MAP, ScvO2 (%), Hct • Randomized, controlled, single-center study • Urban center ED • 130 assigned to early goal directed therapy • 133 assigned to standard therapy – Achieving these targets resulted in a 15.9% absolute reduction in 28 day mortality Protocol for Early Goal-Directed Therapy. Rivers E et al. N Engl J Med 2001;345:1368-1377. Early “Hemodynamic” Goal Directed Therapy: The first 6 hours • Give first 2L IVF bolus over 10 minutes, then check CVP immediately (use pressure bags or rapid infuser) • check measures of vital organ perfusion: – lactate, blood pH, urine output, MAP • Repeat 1L bolus every 10 minutes until CVP 8-12 or vital organ perfusion is achieved Case 1, Part 4 • Patient receives 6L of IVF, CVP 12, and BP now 80/60, urine output 15cc/hr, lactate 5 • Patient meets criteria for septic shock Protocol for Early Goal-Directed Therapy. Rivers E et al. N Engl J Med 2001;345:1368-1377. Vasopressors Vasopressors First line: Norepinephrine (Levophed) Second line: Epinephrine Third line: Vasopressin (0.04 units/min fixed dose) Patient requires norepinephrine and epinephrine to maintain adequate vital organ perfusion Protocol for Early Goal-Directed Therapy O2 delivery = CO x 1.34 x Hb x %saturation O2 Inotropes First line: Dobutamine (max dose 20mcg/kg/min) -myocardial dysfunction -ongoing hypoperfusion despite adequate intravascular volume and MAP Corticosteroids in ICU • Why? – Cytokine release TNF alpha, IL-1, IL-2 via an unknown mechanisms induces adrenal insufficiency • When to start? – When adequate fluid hydration and vasopressors are not enough to restore hemodynamic stability – Cortisol level, ACTH stim test are not needed • Hydrocortisone 50mg IV q6 – Glucocorticoid + Mineralocorticoid effect Protocol for Early Goal-Directed Therapy. Rivers E et al. N Engl J Med 2001;345:1368-1377. Protocol for Early Goal-Directed Therapy UCI Severe Sepsis Order Set Case 1 Review • • • • • • • • • • • SIRS criteria 39 C, HR 130, RR 22, WBC 25K Source of infection identified UO 15cc/hr, lactate 5 2L IVF -> BP 80/60 How much IVF do you give and how? What do you do if MAP still inadequate for vital tissue perfusion? How do you assess adequate tissue perfusion? Which vasopressors? When do you transfuse PRBC? When do you start steroids and which one? What is the name of the order set if you don’t know what to do for sepsis? Case 1 Finale • Transferred out of ICU 2 days later • Patient survived • GOOD WORK! The key to success as an intern in the ICU: • Hypotension is a vital sign • Shock is a physiologic state defined by vital organ hypoperfusion • MAP goal is to maintain perfusion of the vital organs – MAP = CO x SVR – MAP = 1/3 SBP + 2/3 DBP • 5 categories of shock: Hypovolemic, Distributive, Cardiogenic, Obstructive, Septic • Identify shock early in patients on the wards and ICU • Know goal directed therapy! Etiologies of Shock CATEGORY PHYSIOLOGY ETIOLOGIES Hypovolemic Decreased venous return Blood loss Fluid loss Cardiogenic Cardiac pump failure/Low CO Left/Right Ventricular failure Valvular dysfunction Arrhythmia Distributive Decreased SVR (Vasodilated) Anaphylactic (FFP) Adrenal insufficiency Neurogenic Obstructive Extra-cardiac obstruction to blood flow Tamponade Pulmonary Embolus Tension Pneumothorax Septic Sepsis References • Early Goal Directed Therapy in the Treatment of Severe Sepsis and Septic Shock NEJM 345, 19. Nov 8, 2001 • Principles of Critical Care, 3rd edition. Chapter 21: Shock • Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. Critical Care Medicine. 37(5):1670-1677, May 2009. • Surviving Sepsis Campaign • Corticus trial: Corticosteroids in sepsis • Transfusion Requirements in Crticial Care evaluated mortality and Hb 7-9 From: Medical Management of Advanced Heart Failure JAMA. 2002;287(5):628-640. doi:10.1001/jama.287.5.628 Date of download: 7/20/2013 Copyright © 2012 American Medical Association. All rights reserved.