Quality of care Israel De Alba, MD MPH Clinical Professor Health Sciences
advertisement

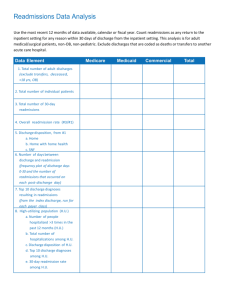
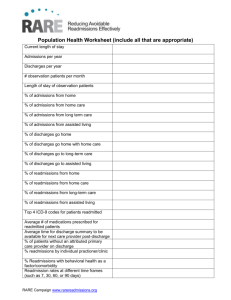
Quality of care Israel De Alba, MD MPH Clinical Professor Health Sciences University of California, Irvine Content Introduction: quality of care today Core measures HCAPS Patient Satisfaction Survey Hospital Readmission Reduction Program Universal Protocol (Time out) The new face of health care Emphasis on efficient, lean care Change in payment structure Emphasis on disease rather than on health Disease makes money; health doesn’t The standard fee-for-service system that encourages doctors and other caregivers to give lots of tests, individual treatments and to prescribe drugs, instead of keeping patients well Oversight: Governtment agencies Insurance companies Quality agencies Patients Quality of care (Institute of Medicine) Safe – avoiding injuries to patients from the care that is supposed to help them. Effective – providing services based on scientific knowledge to all who could benefit and refraining from providing services to those not likely to benefit (avoiding underuse and overuse). Patient-centered – providing care that is respectful of and responsive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions. Timely – reducing waits and sometimes harmful delays for both those who receive and those who give care. Efficient – avoiding waste, in particular waste of equipment, supplies, ideas, and energy. Equitable – providing care that does not vary in quality because of personal characteristics, such as gender, ethnicity, geographic location, and socioeconomic status. Center for Medicaid and Medicare Services HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) survey is the first national, standardized, publicly reported survey of patients' perspectives of hospital care. Contains 18 core questions communication with nurses and doctors responsiveness of hospital staff the cleanliness and quietness of the hospital environment pain management communication about medicines discharge information overall rating of hospital would they recommend the hospital Patient satisfaction Core Measures: Joint Commission Heart failure MI timely care MI effective care Pneumonia markers DVT prevention Hospital acquired infections Hospital readmission reduction Decreasing Hospital Readmissions Beginning in fiscal year (FY)2013, hospitals with higher than expected readmission rates will experience a decrease in payment for all Medicare discharges Reduce payment to hospital by 1% in FY 2013 and 2% in 2014 and 3% beyond Expected to save $7.1 billion over 10 years Performance data will initially be based on 30 day readmissions for MI, HF and pneumonia Additional conditions added in 2015 (COPD, CABG, PCA) Avoidable Readmissions Evidence suggests many rehospitalization may be preventable No one knows what proportion of readmissions are truly “avoidable”? Large interstate and inter-hospital variation Many readmissions are outside the control of the hospital or health system Many readmissions are appropriate and the goal is not to avoid all readmissions Some interventions have demonstrated the ability to decrease readmissions Readmission rates The patient perspective Patients did not necessarily see hospital readmissions as a problem Many patients felt they were discharged too soon. Many did not understand their discharge instructions. Care instructions were too general. Patients and caregivers wished they had been more assertive. New diagnoses posed special challenges. Primary care physicians were missing from the picture. Some had only limited or no support once home. Some were not ready to change behaviors A few had chronic health conditions for years but were not educated about their illnesses. The physician perspective The issue is on their radar. Readmissions are complicated. There are financial pressures to discharge as soon as possible. The quality and training of the providers can make a difference. Some hospitals are improving the discharge process and in-hospital experience to reduce readmissions. Some hospitals try to avoid readmissions by referring patients to their own outpatient clinics for follow-up care. Project RED Discharge Checklist Eleven mutually reinforcing components: 1. Medication reconciliation 2. Reconcile discharge plan with national guidelines 3. Follow-up appointments 4. Outstanding tests 5. Post-discharge services 6. Written discharge plan 7. What to do if problem arises 8. Patient education 9. Assess patient understanding 10. Discharge summary sent to PCP 11. Telephone reinforcement What is Universal Protocol? The Joint Commission Board of Commissioners originally approved the Universal Protocol for Preventing Wrong Site, Wrong Procedure and Wrong Person Surgery Process that involves 3 steps Pre-procedure verification Site marking Time out Universal Protocol Three steps to patient safety 1. Pre-procedure verification 2. Site marking 3. Time Out 1. Pre-procedure verification • The first SAFETY CHECK • Is a process of information gathering and confirmation, including verification of: • Correct patient, correct procedure, correct site • Documentation (H&P/interval note, consent form, other assessments) • Supplies: blood products, implants, devices, and/or special equipment for the procedure • Other: labeled diagnostic and radiology test results • Assures that missing information or discrepancies are addressed before starting the procedure 2. Site Marking • Required prior to procedures involving incisions or percutaneous puncture or insertion • Mark the site before the procedure is performed and involve the patient in the site marking process, if possible • The site does not need to be marked for bilateral structures Department Name | Month X, 201X 3. Time-Out • Final SAFETY CHECK before starting the procedure • Activities are suspended so that ALL team members time out. • can fully engage in the The focus is on ACTIVE confirmation of the patient, site, and procedure • For bedside or ambulatory practice procedures, the physician performing the intervention or other trained member of the procedural team may lead the time-out. • The procedure is NOT started until all questions or concerns are resolved. Time-Out The time-out must address: Correct patient identity Accurate procedure consent form or physician order Correct side/site marked Agreement on procedure to be done The time-out should also address, where applicable: Correct patient position Relevant images/results displayed The need to administer antibiotics or fluids for irrigation Safety precautions based on patient history or medication use. QUEST Documentation 31 Department Name | Month X, 201X 32 Department Name | Month X, 201X Summary and conclusions Quality of care: why it matters to you New paradigm These changes will affect how we practice medicine