ICU Case of the Block
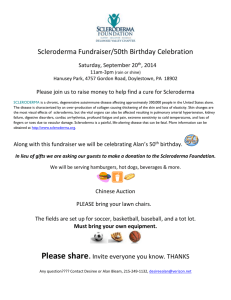
advertisement
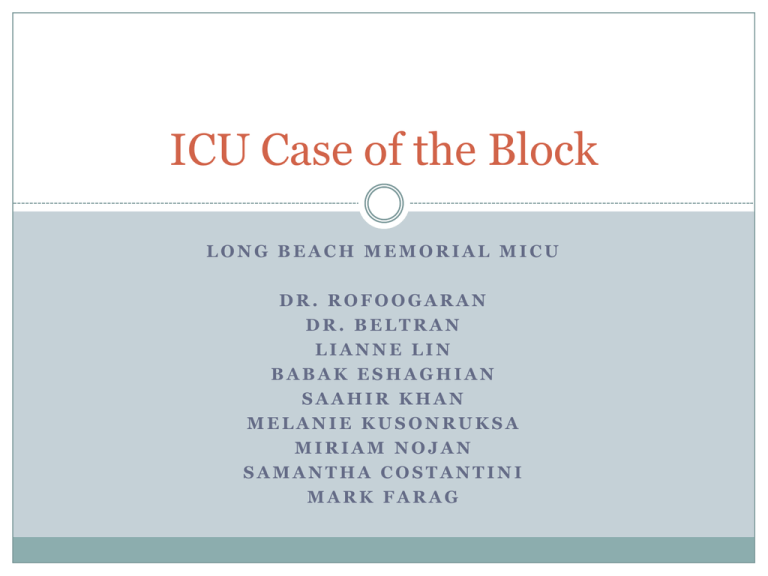
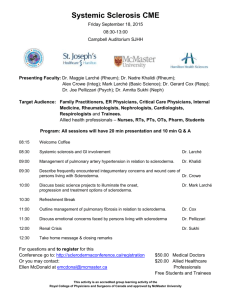
ICU Case of the Block LONG BEACH MEMORIAL MICU DR. ROFOOGARAN DR. BELTRAN LIANNE LIN BABAK ESHAGHIAN SAAHIR KHAN MELANIE KUSONRUKSA MIRIAM NOJAN SAMANTHA COSTANTINI MARK FARAG Prior Admission 33 year old male admitted 6mo ago for shortness of breath, productive cough x 3 days, night sweats, and subjective fever, also notable for 40 lb weight loss in past 4 months, attributed to depression due to losing custody of child. CXR: Suspicious for multifocal pneumonia CT Chest: Suggestive of atypical/multifocal pneumonia, possible interstitial pattern Treatment: Ceftriaxone and Azithromycin -> Levaquin, Remeron added by psychiatry for severe depression Negative workup for TB, HIV, Hepatitis Discharged to home in stable condition HPI 32yo M, PMH of major depressive disorder and 80-lb weight loss over 8 months attributed to depression Presents with chest pain, dyspnea on exertion Admitted to ICU for hypotension, dyspnea and elevated troponin. Intermittent chest pain since 3-4 days ago, lower left chest, relieved by rest. Shortness of breath since 3-4 days ago with activity, relieved by rest, associated with bilateral lower leg swelling and 2pillow orthopnea. Denies any trauma, denies recent substance use other than marijuana, denies meth and cocaine other than one episode 10yrs ago, states last alcohol use 4 months ago, denies personal or family history of cardiac disease, denies fever/chills, headache, abdominal pain. Physical Exam GEN: Anxious on BIPAP, labored breathing without BIPAP, no acute distress HEENT: normocephalic, atraumatic, perrl, eomi, oropharynx clear, moist mucous membranes NECK: supple, no jvd CV: tachycardic with regular rhythm, + S4, 1/6 systolic murmur in LRSB, no rubs or gallops LUNGS: bibasilar crackles L>R, otherwise clear ABD: normoactive bs, soft, nt/nd, no HSM, no masses, no CVAT EXT: warm, well-perfused, peripheral pulses 1+ difficult to palpate due to thick skin, no cyanosis or edema SKIN: No rashes, ulcers, or lesions noted NEURO: alert and oriented x3, CNII-XII intact, 5/5 motor strength and sensation to light touch grossly intact throughout, nonfocal Labwork Pertinent labs: CBC: WBC 13.1, Hgb 12.7, Plat 334 CMP: BUN 23, Cr 0.67, ALT 166, AST 152, otherwise wnl BNP: 952 Trop: 3.00, CK 119 ABG: 7.55, 28, 178, 25 Lactate: 1.9 Utox: +Cannabinoids Imaging: CXR Imaging: CT Chest ECHO SUMMARY: 1. Left ventricular ejection fraction \R\ <20 %. 2. Severely decreased left ventricular systolic function. 3. Moderate to severe mitral valve regurgitation. 4. Grade II (pseudonormal) left ventricular diastolic dysfunction. 5. Hypokinetic right ventricular function. 6. Dilated right ventricle. 7. Dilated left atrium. 8. Dilated right atrium. 9. Moderately reduced right ventricular systolic function. 10. Small pericardial effusion. 11. Estimated pulmonary artery pressure 35 mmHg EKG Hospital Course 8/21: Hospital Day #1 Pt continues to have increased WOB, but does not tolerate BIPAP well and refuses intubation Central line placed for blood pressure support, pt declines arterial line Consults: Cardiology: On physical exam, noticed upper chest wall thickening, skin thickening on bilateral hands, unable to form fists; Recs: unlikely ACS, await echo, hold heparin and follow rheum consult Rheumatology: Findings as seen above +nail pitting, pt reported difficulty swallowing liquids and solids, always feels like he is choking; Recs: IVIG for systemic sclerosis picture, Cytoxan once PNA clears, full rheumatologic workup Hospital Course 8/22: Hospital Day #2 Trop trending down, 1.92 ESR 24, CRP 2.7 Pt subjectively feeling better after first dose of IVIG Increasing levophed requirement to maintain BP Consults: Cardiology: Top of cardiac differential is either Scleroderma effects and/or acute myocarditis, IVIG would help with both Rheumatology: Continue IVIG, f/u rheum labs, recommend barium swallow, bronchoscopy and BAL to rule out infection Hospital Course 8/23: Hospital Day #3 Acutely short of breath on BIPAP, RR 30-40s Emergent intubation and A-line insertion, patient markedly hypotensive Asystole on cardiac monitoring @ 10:30, code blue called Coded for 30 minutes in PEA arrest, ROSC, pulses not palpable but seen on doppler Bicarb drip + bicarb amps + pressors Family informed, at bedside, patient full code Hospital Course 8/23: Continued Code Blue Labs: Cr: .63 -> 1.16 AG: 9 -> 26 ALT: 135 -> 701 AST: 113 -> 1051 Lactic Acid: 1.9 -> 18.7 CPK: 1025 Myoglobin: 2871 Hospital Course 8/23-8/24: Hospital Day #4 Continued to require increasing doses of pressors, family at bedside. Family decided to make patient DNR/DNI, pt went into asystole and declared dead. Post-mortem labs: ANA +, Anti-Scl70, dsDNA, anti-Smith, anti-CCP, RF, C3, C4, Ro, La (-) Diagnosis?? Scleroderma Disorders Peak onset between 30-50, women Skin involvement nearly universal from excess collagen Severity and extent is variable Classifications Limited cutaneous systemic sclerosis (lcSSc) restricted to hands, distal forearm > face and neck prominent vascular manifestations (CREST) Diffuse cutaneous systemic sclerosis (dcSSc) trunk, upper arms and shoulders involvement significant fibrotic internal organ damage Systemic sclerosis sine scleroderma Environmentally induced scleroderma Overlap syndromes Pre-scleroderma Clinical Manifestations SCLERODACTYLY plus multiorgan involvement: Rheumatology Image bank "On-line Archives of Rheumatology" © , 1996-2006 http://www.rheumatologynetwork.com/articles/limited-joint-mobility-diabetesmellitus-clinical-implications#sthash.A8P1MsuN.dpuf Clinical Manifestations SCLERODACTYLY plus multi-organ involvement: RAYNAUD phenomenon HEARTBURN, dysphagia and esophageal dysmotility Dyspnea on exertion (ILD from NSIP) Pulmonary hypertension Myocardial fibrosis, pericarditis and effusion, arrhythmias, CAD, dilated > restrictive heart failure Acute hypertension and renal insufficiency (renal crisis) Malabsorptive diarrhea Characteristic mucocutaneous telangiectasia on the face Digital infarctions and digital tip pitting scars Arthralgias, arthritis, myalgias, tendon friction rub Erectile dysfunction Diagnosis Suggested by skin thickening and sclerosis Supported by extracutaneous features and autoantibodies (ANA) Serologic tests confirm but do not exclude diagnosis of systemic sclerosis >99.5% specific, but 20-50% sensitive >95% of SSc patients have at least one: Anti-topoisomerase I (anti-Scl-70) Anti-RNA polymerase III antibodies Anti-centromere (ACA) Anti-U3 RNP (fibrillarin) Anti-PM-Scl myositis overlap Anti-beta2 glycoprotein I Additional Studies BAL fluid: exclude infection typically increased neutrophils and eosinophils, sometimes lymphocytes and mast cells Lung biopsy: limited utility symptomatic and physiologic severity of ILD are better predictors of outcome Skin biopsy: differentiate from other etiologies Treatment Cyclophosphamide with low dose glucocorticoids Azathioprine plus glucocorticoids Pneumocystis jirovecii prophylaxis Methotrexate (but risk for pulmonary fibrosis) ? Rituximab ? IVIG Lung Transplantation in select SSc patients Prognosis SSc has the highest case-specific mortality of any of the auto-immune rheumatic diseases Predictors of poor prognosis Diffuse skin involvement Symptomatic cardiac involvement: two- and five-year mortality rates of 60 and 75% Interstitial lung disease and rapid DLCO decline: nine-year survival rate of 30% References Denton, Christopher P. Immunomodulatory and antifibrotic approaches to the treatment of systemic sclerosis (scleroderma). Uptodate. Denton, Christopher P. Overview of the treatment and prognosis of systemic sclerosis (scleroderma) in adults. Uptodate. Vargas, John. Clinical manifestations of systemic sclerosis (scleroderma) lung disease. Uptodate. Vargas, John. Diagnosis and differential diagnosis of systemic sclerosis (scleroderma) in adults. Uptodate. Vargas, John. Overview of the clinical manifestations of systemic sclerosis (scleroderma) in adults. Uptodate. Vargas, John. Prognosis and treatment of interstitial lung disease in systemic sclerosis (scleroderma). Uptodate.