Systemic Vasculitis: a clinical approach Geordie Lawry MD Chief, Rheumatology
advertisement

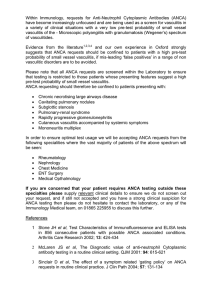
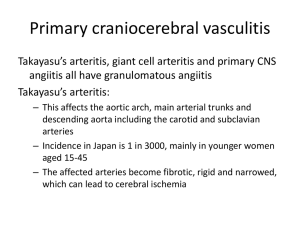
Systemic Vasculitis: a clinical approach Geordie Lawry MD Chief, Rheumatology UC IRVINE Medicine HS Noon Conference: October 2015 Objectives 1 • List the 4 clinical features which should prompt you to CONSIDER A DIAGNOSIS of systemic vasculitis • List the “Big 5” essential questions in patients with SUSPECTED GIANT CELL ARTERITIS • Describe what is meant by PULMONARY RENAL SYNDROME Objectives 2 • List at least 3 ORGANS / SITES commonly involved in: CRYOGLOBULINEMIC VASCULITIS GRANULOMATOUS POLYANGIITIS (GPA) MICROSCOPIC POLYANGIITIS (MPA) CLASSIC POLYARTERITIS NODOSA GIANT CELL ARTERITIS Objectives 3 • List at least 2 ANCA VASCULITIS SYNDROMES, associated ANCA pattern / target antigens • List at least 2 vasculitides which are NOT ASSOCIATED WITH ANCA • List at least 3 or more conditions that can MIMIC THE CLINICAL FEATURES OF VASCULITIS VASCULITIS: Talk Outline • Introduction and Definitions • Approach to vasculitis • Specific Disorders: – Giant Cell Arteritis – Granulomatous polyangiitis (Wegener’s) – Microscopic Polyangiitis – Polyarteritis Nodosa – Cryoglobulinemia • Take Home VASCULITIS: principles 1 group of clinical syndromes characterized by inflammation of blood vessels Normal Artery Artery: WBC inflammation in wall VASCULITIS: principles 2 systemic diseases that can affect many different organ systems can be difficult to diagnose: challenging clinical picture even for experienced clinicians can be life-threatening VASCULITIS: classification www.wegenersgranulomatosis.net/imageRJN.JPG General Approach to Vasculitis Throw up your hands…. General Approach to Vasculitis Slap at it …. When should vasculitis be suspected? 1 • MULTISYSTEM inflammatory disease • Significant CONSTITUTIONAL SYMPTOMS • RAPIDLY PROGRESSIVE organ dysfunction • HIGH ESR SEVERE anemia PLATELETS > 500K When should vasculitis be suspected? 2 CLINICAL FEATURES PARTICULARLY SUGGESTIVE of small vessel inflammation: • SKIN: palpable purpura * • LUNGS: pulmonary infiltrates / hemoptysis • KIDNEY: active urinary sediment • NEURO: foot drop ** What is the approach to a patient suspected of having vasculitis? WHAT IS YOUR APPROACH TO ANY COMPLEX MEDICAL PROBLEM? General Approach to Vasculitis Gather your equipment…. Find the target…. Take aim….. NAIL IT ! COMPLEX MEDICAL PROBLEMS 1 HISTORY: PATIENT’S STORY get careful CHRONOLOGY …….PROBLEMS PHYSICAL EXAM: BODY’S STORY thoughtful, thorough ……..MORE PROBLEMS LABORATORY: BEHIND-THE-SCENES STORY Basic CBC, CHEMS, LFTs, UA/micro, CXR ……..MORE PROBLEMS COMPLEX MEDICAL PROBLEMS 2 Develop a strategy: PROBLEM LIST CREATE PROBLEM LIST ……… LIST EVERYTHING [split don’t lump] PRIORITIZE PROBLEM LIST ……… WHAT’S THE BIG GORILLA(S) HERE? “WORK” the PROBLEM LIST COMPLEX MEDICAL PROBLEMS 3 “WORK” the PROBLEM LIST • Think of 3 explanations for each problem Create a differential diagnosis • What are the major organs involved? • Do they inter-relate? Do the patient’s, body’s and the behind-thescenes stories fit together in some way? COMPLEX MEDICAL PROBLEMS 4 SYSTEMIC VASCULITIS ? • Are there additional tests which could help confirm this suspicion? • Serologic tests • Imaging studies • Tissue biopsy VASCULITIS: additional testing 1 Serologic tests • ANCA • Hepatitis B surface antigen • Hepatitis C, C3 & C4 • HIV • ANA • ACA, “lupus” anticoag panel VASCULITIS: additional testing 2 Imaging studies • Sinus CT scan • Chest CT scan • Mesenteric angiogram VASCULITIS: additional testing 3 Tissue biopsy • Temporal artery • Sural nerve • Muscle • Lung • Renal Common Clinical Manifestations • Systemic – Fever, sweats, weight loss • Respiratory – Sinusitis / Epistaxis – Pulmonary infiltrates • Skin – Palpable Purpura • Neurologic – Mononeuritis Multiplex • Musculoskeletal – Arthralgia / arthritis – Muscle pain / claudication • Gastrointestinal – Abdominal Pain – Bloody stools • Renal – Glomerulonephritis – Hypertension CUTANEOUS Palpable Purpura Livedo Reticularis Splinter Hemorrhages NEUROLOGIC • Mononeuritis multiplex: check for FOOT DROP Sural nerve biopsy showing vasculitis RESPIRATORY: upper • Sinusitis • Or…… www.conseils-orl.com/.../sommaire_epistaxis.htm RESPIRATORY: lower • Pulmonary infiltrates • Nodules • Cavities GENITOURINARY • • • • Glomerulonephritis Hypertension Hematuria RBC casts • Testicular pain (especially PAN) www.bio.davidson.edu/.../Cresgn.jpg MUSCULOSKELETAL • Polyarthralgias - common • Polyarthritis - less common • Myalgias - common • Myositis - biopsy may demonstrate vasculitis in muscle GASTROINTESTINAL • Mesenteric ischemia – pain 30 minutes after eating – bloody diarrhea – bowel perforation • hepatitis • pancreatitis • cholecystitis library.med.utah.edu/WebPath/COW/COW125.html OCULAR Scleritis Retinal Vasculitis Iritis http://www.uveitis.org/images/sa rcoid6.jpg eyelearn.med.utoronto.ca/.../RedE ye/10Sclera.htm http://webmedia.unmc.edu/eye/iritis.jpg Common Laboratory Findings INFLAMMATION: Elevated ESR (can be > 100) Elevated CRP Leukocytosis Thrombocytosis Anemia Low Albumin VASCULITIS MIMICS • INFECTIOUS DISEASES – Endocarditis – HIV • DRUGS – Cocaine – Methamphetamine • CHOLESTEROL EMBOLI • ANTIPHOSPHOLIPID ANTIBODY SYNDROME Questions? • In the ACR diagnostic criteria for Giant Cell Arteritis (Temporal Arteritis), a patient needs to be greater than what age? A. B. C. D. E. > 40 years > 50 years > 60 years > 70 years > 80 years Questions? • In the ACR diagnostic criteria for Giant Cell Arteritis (Temporal Arteritis), a patient needs to be greater than what age? A. B. C. D. E. > 40 years > 50 years > 60 years > 70 years > 80 years -Almost all are > 60 -Average age is 70 Specific Entities www.wegenersgranulomatosis.net/imageRJN.JPG Giant Cell Arteritis ACR Criteria (3 of 5) • • • • Age > 50 New onset headache ESR (Westergren) 50 Abnormal artery biopsy (mononuclear cell infiltrate, granulomatous inflammation, usually multinucleated giant cells) • Temporal artery abnormality (tender or decreased pulse) Arthritis Rheum. 1990;33:1122. Giant Cell Arteritis (Other clinical manifestations) • Visual loss, jaw/tongue claudication, scalp tenderness • Fever, weight loss • PMR symptoms (proximal muscle pain) • 10% with large vessel involvement (e.g. subclavian artery) • Blindness (ischemic optic neuropathy) is major complication to avoid GCA:Biopsy • Temporal artery biopsy – large specimen (4-6 cm) – multiple sections evaluated • Infiltration of vessel wall with WBC • Granulomata, Giant Cells • Necrotic material GCA: Therapy • Corticosteroids mainstay of therapy (~1 mg/kg) – Calcium and vitamin D – Consider bisphosphonates • Try to prevent visual loss with therapy: – Treat, then biopsy! Questions? • The confirmatory antibody for a positive CANCA in a patient suspected of having Wegener’s Granulomatosus is: A. B. C. D. E. Topoisomerase Histidine tRNA synthetase Smith Proteinase-3 Myeloperoxidase Questions? • The confirmatory antibody for a positive CANCA in a patient suspected of having Wegener’s Granulomatosus is: A. B. C. D. E. Topoisomerase Histidine tRNA synthetase Smith (Sm) Proteinase-3 C is the 3rd letter Myeloperoxidase of the alphabet: Pr-3 C-ANCA Granulomatous Polyangiitis (GPA) … formerly Wegener’s • Necrotizing vasculitis that affects the small vessels of the respiratory tract and renal system: PULMONARY-RENAL SYNDROME • Age ~ 40s: M > F 2:1 Granulomatous Polyangiitis (GPA) ACR Criteria (3 of 5) • Nasal or oral inflammation (oral ulcers or bloody nasal drainage) • Abnormal chest radiograph (nodules, fixed infiltrates, cavities) • Urinary sediment (> 5 RBC/ hpf or casts) • Abnormal Biopsy: showing vasculitis • Proteinase-3 antibodies Arthritis Rheum 1990;33:1101. Granulomatous Polyangiitis (GPA) : Respiratory Involvement • Sinusitis – Nasal septal ulceration • Pneumonitis – few symptoms until late – usually no mediastinal lymphadenopathy – nodules that can cavitate Granulomatous Polyangiitis (GPA) : Renal Involvement • 85% of patients • Focal/segmental necrotizing glomerulonephritis • Usually progressive www.bio.davidson.edu/.../Cresgn.jpg Granulomatous Polyangiitis (GPA) : ANCA • AntiNeutrophil Cytoplasmic Antibody – C (cytoplasmic staining) ANCA – Proteinase 3 (C is the 3rd letter) • Pulmonary-renal disease – sensitivity of 95% – specificity of 95% • Limited disease… – lower sensitivity and specificity Granulomatous Polyangiitis (GPA): Tissue Biopsy • Yield of biopsy – Lung • Open – highest yield • Bronchoscopy - lower yield – Sinus - 40% yield – Renal • Vasculitis rarely seen • Focal proliferative GN is the typical finding Granulomatous Polyangiitis (GPA) : Rx • Prior to cyclophosphamide, 80-90% mortality • With cyclophosphamide, 5-10% mortality • Concern about long-term toxicity of PO cyclophosphamide (bladder especially) • IV CYTOXAN no significant bladder risk • Rituximab: very effective for induction & maintenance • Azathioprine for maintenance Microscopic Polyangiitis (MPA) • Systemic vasculitis with predominant small vessel involvement • Separate disease from PAN (Initially thought to be a variant of PAN) • Usually RPGN and sometimes with pulmonary hemorrhage • More common than PAN (both are rare) MPA: Clinical Manifestations • • • • • • • Renal manifestations Weight loss Skin involvement Mononeuritis multiplex Fever Arthralgias/Myalgias Pulmonary involvement 79% 73% 62% 58% 55% 50% 25% MPA: ANCA • P (perinuclear) ANCA • Myeloperoxidase antibodies • Sensitivity/Specificity unclear MPA: Epidemiology & Rx • Ave. age 57 • Males > Females (slightly) • Cyclophosphamide decreases mortality • IV CYTOXAN no significant bladder risk • Rituximab: very effective for induction & maintenance • Azathioprine for maintenance Polyarteritis Nodosa • Necrotizing vasculitis of medium & small arteries • Age ~ 40s; M > F • Constitutional symptoms are common – fever – weight loss 50% 50% • Vasculitis can be variable in distribution making diagnosis difficult Polyarteritis Nodosa ACR Criteria (3 of 10) • • • • Wt loss > 4 kg Livedo reticularis Testicular pain Myalgias, weakness or leg tenderness • Mononeuropathy or polyneuropathy • • • • Diastolic BP > 90 BUN or Creatinine Hepatitis B virus Arteriographic abnormality • Biopsy of small or medium artery containing PAN Arthritis Rheum. 1990;33:1088 Classic PAN: Manifestations • Mononeuritis multiplex • Renal involvement: 50% 60% (renal arteries, interlobular arteries) – Hypertension (more common) – Glomerulonephritis (uncommon) • • • • Abdominal involvement Arthralgias/Myalgias/Myositis Testicular pain Pulmonary involvement rare 45% 64% 25% Polyarteritis Nodosa • Association with Hepatitis B (surface antigen) • Classic PAN is NOT associated with ANCA ANCA Cryoglobulinemia 1 • • • • • Paradigm of small vessel vasculitis Association with hepatitis C infection Damage is immune complex-mediated Cryoprecipitate Hepatitis C Ag – Ab Complement fixing: C4 consumption C4 levels VERY low Cryoglobulinemia 2 Cryoglobulinemia 3 PATTERN OF ORGAN INVOLVEMENT: • constitutional • Cutaneous • articular • vascular • neurologic Cryoglobulinemia 4 PATTERN OF LABORATORY FINDINGS: • rheumatoid factor • complement C4 ↓ ↓ ↓ • cryoglobulin (cryocrit) TREATMENT: • Antiviral therapy …. clearance of hep C virus! VASCULITIS: classification www.wegenersgranulomatosis.net/imageRJN.JPG VASCULITIS OF SMALL >> MEDIUM-SIZED VESSELS: • drug-induced small vessel vasculitis (hypersensitivity vasculitis), • Henoch-Schönlein purpura (IgA vasculitis), • ANCA-associated vasculitis (granulomatosis with polyangiitis [Wegener’s], microscopic polyangiitis, eosinophilic granulomatosis with polyangiitis [Churg Strauss syndrome]), • infection-related vasculitis (bacterial endocarditis, poststreptococcal vasculitis and glomerulonephritis) plus hepatitis C-related cryoglobulinemia) • vasculitis associated with CTD (SLE, RA, Sjögren's) VASCULITIS OF MEDIUM-SIZED VESSELS: • classic polyarteritis nodosa (PAN) VASCULITIS OF LARGE VESSELS: • Giant cell arteritis • Takayasu arteritis MIMICS OF VASCULITIS: • infectious, thrombotic, and embolic disorders