Unusual anterior Uveitis in a Child
advertisement

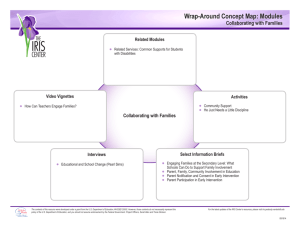
Unusual anterior Uveitis in a Child Ocular History 10 year old boy 1/2001: OD>OS red eyes iris thickening, endothelial precipitates, hyphema topical corticosteroids IOP: OD: 40mmHg YAG-iridotomy: unsuccessfull First Diagnosis Anterior uveitis of unknown origin Treatment topical corticosteroids every hour Ocular History at Presentation 6 weeks after first symptoms VA OD 8/20; OS 12/20 IOP: 18/16mmHg slitlamp OD: iris thickening, endothelial precipitates, hyphema Fundus: unremarkable First Presentation - OD First Presentation - OD massive granulomatous precipitates Ocular History at Presentation slitlamp OS iris prominence at 11 o´clock mild anterior chamber cells 1+ fundus: unremarkable First Presentation - OS General History unclassified malformation syndrome with anal atresia, insufficiency of the pituitary gland heart transplantation at the age of 3 due to dilative cardiomyopathy with endocardial fibrosis several transplant rejections (2000) Immunosuppression at the moment Cyclosporin A, Azathioprin Second Diagnosis CMV induced uveitis based on: CMV mismatch at transplantation leading to high IgG- and IgMantibody titers against CMV Change of Treatment systemic ganciclovir in addition repeated negative PCR and PP-65 ruled out active CMV, leading to stop of ganciclovir clinically and serologically no evidence for sarcoidosis, toxoplasmosis, toxocara or HIV-infection Follow up – After 3 Months angle closure - peripheral iridectomy severe hyphema systemic corticosteroids Histology of Irisbiopsy first view lymphocytes no lymphoma severe inflammation second view: very few mitotic cells probably low malignant non Hodgkin-lymphoma Irisbiopsy – HE-Staining polymorphic lymphocytic infiltration (brown) Rohrbach et al. Graefe´s Arch Clin Exp Ophthalmol 2004 Immunohistology of Irisbiopsy CD 20 +/ CD3 - lymphocytes Irisbiopsy- Immunostainig Rohrbach et al. Graefe´s Arch Clin Exp Ophthalmol 2004 Irisbiopsy - EBV irisbiopsy: positive PCR for EBNA-1 EBV-load: 5,6 x 10-3 (20 x elevated) monoclonal rearrangement in the CD2 region of Ig heavy chain gene in cells of the tumour (IgH-gene) Gel-Electrophoresis PCR with primers for the Ig heavy chain gene, hypervariable region A,B: tumour L: length marker P: pos. control lane 5, 6: neg. control A B P L Rohrbach et al. Graefe´s Arch Clin Exp Ophthalmol 2004 Diagnosis Posttransplantation-Lymphoproliferative Disease (PTLD) localized NH-lymphoma in children after severe immunosuppression nearly exclusively associated to EBV interpretation of histology known to be difficult Follow up – After 5 Months low dose CsA, azathioprine stopped ganciclovir orally OS: iris tumor regressed slightly OD: iris tumor progressed high EBV-replication rate in mononuclear blood cells Follow Up – After 6 Months Follow up - After 6 Months radiation (5 x 2.0 Gy/week) well tolerated at the end of the radiation mild conjunctivitis partial remission of the tumor Follow up - After 8-12 Months complete remission of the ocular tumor hypotonic situation cataract with convergent squint still very high EBV titers Follow Up- After 8 Months OD Follow Up – After 13 Months viral load half of the beginning still consistant with persistant active EBVinfection foscarnet started after a few weeks: viral load even higher than before begin of the foscarnet therapy probably high risk for more lymphoma Follow Up – After 17 Months collection of EBV-infected B-cells from the patient generation of patients own specific cytotoxic anti-EBV T-cells Center for Gene and Cell Therapy Houston TX, USA Follow Up – After 22 Months anti-EBV Treatment reinfusion of the T-cells in 3 portions reduction of the EBV load free of cells in the anterior chamber Last Control – After 32 Months VA: OD: hand movements, OS: 16/20 OU: clear cornea, no AC cells no iris tumors IOP 5 and 10 mmHg OD: dense cataract, surgery planned then lost for follow-up Posttransplantation Lymphoproliferative Disorder all age groups after transplantation of kidney, liver, heart, lung or bone marrow incidence ca. 2-3 % latency few weeks to 3 years highest incidence probably in the first year after transplantation Posttransplantation Lymphoproliferative Disorder special entity, no simple lymphoma 3 variants circumscribed lesion, typically later than 1 year after tranplantation, often localized in the CNS, gastrointestinal tract or salivary glands benign, selflimiting disease resembling mononucleosis malignant widespread lymphoproliferation with high mortality Ocular PTLD Brodsky et al 1991 until now 14 cases (50% with syst. disease) 7 with iris nodules 2 with iris nodules and subretinal mass 1 with widespread disease (uvea, retina, optic nerve,orbit) 1 vitritis,1chorioretinitis,1 anterior uveitis 1 orbital mass Histology of Ocular PTLD proliferation of B-cells and/or plasma cells proliferation of T-cells in 10% polyclonal or monoclonal Role of EBV most PTLD caused by a chronic EBV-infection EBV negativ recipients are at higher risk than positive detectable in the tumor and blood monocytes anti-T-cell treatment especially dangerous CMV-infection elevates risk for PTLD therapy: reduction of IS, increase antivirals Conclusion PTLD incidence ca. 2-3% diagnosis: history of solid organ transplantation can affect the eye iris nodules uveitis therapy: reduction of immunosuppresion virustatics generation of own anti-EBV cytotoxic T-cells