Coping Predictors of Children’s Laboratory-Induced Pain Tolerance, Intensity, and Unpleasantness
advertisement

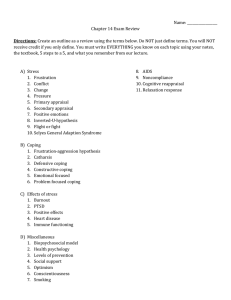
The Journal of Pain, Vol 8, No 9 (September), 2007: pp 708-717 Available online at www.sciencedirect.com Coping Predictors of Children’s Laboratory-Induced Pain Tolerance, Intensity, and Unpleasantness Qian Lu,* Jennie C. I. Tsao,* Cynthia D. Myers,† Su C. Kim,* and Lonnie K. Zeltzer* *Pediatric Pain Program, Department of Pediatrics, David Geffen School of Medicine, University of California Los Angeles, Los Angeles, California. † Integrative Medicine Program, Department of Interdisciplinary Oncology, H. Lee Moffitt Cancer Center & Research Institute, Tampa, Florida. Abstract: This study examined coping predictors of laboratory-induced pain tolerance, intensity, and unpleasantness among 244 healthy children and adolescents (50.8% female; mean age, 12.73 ⴞ 2.98 years; range, 8 –18 years). Participants were exposed to separate 4-trial blocks of pressure and thermal (heat) pain stimuli, as well as 1 trial of cold pain stimuli. Strategies for coping with pain were measured using the Pain Coping Questionnaire (PCQ). Linear regression analyses were conducted to examine the associations between the 8 PCQ subscales and pain responses (pain tolerance, intensity, and unpleasantness) to all 3 pain tasks, controlling for age and sex. We found that internalizing/ catastrophizing predicted higher pain intensity across the 3 pain tasks and higher cold pain unpleasantness; seeking emotional support predicted lower pressure pain tolerance; positive self-statements predicted lower pressure pain intensity and lower cold pain intensity and unpleasantness; and behavioral distraction predicted higher pressure pain tolerance and lower heat pain unpleasantness. These results suggest that in healthy children, internalizing/catastrophizing, and seeking emotional support may be conceptualized as pain-prone coping strategies, and positive self-statements and behavioral distraction as pain-resistant coping strategies within the context of laboratory pain. Perspective: These results support investigation of interventions with children that aim to reduce acute pain responses by modifying coping to reduce seeking of emotional support and catastrophizing and enhance the use of positive self statements and behavioral distraction. © 2007 by the American Pain Society Key words: Laboratory pain, children, seeking emotional support, positive self-statements, internalizing/catastrophizing, distraction. T he study of pre-existing coping strategies within the context of laboratory induced pain has important clinical implications for the management of children undergoing painful medical procedures.25 In contrast to clinical pain studies where it is difficult to partial out the influence of highly variable pain sympReceived December 8, 2006; Revised March 23, 2007; Accepted April 30, 2007. Supported by R01DE012754, awarded by the National Institute of Dental and Craniofacial Research, and UCLA General Clinical Research Center Grant MO1-RR-00865 (PI: Lonnie K. Zeltzer). Dr. Lu is supported by UCLA Jonsson Comprehensive Cancer Center Postdoctoral Fellowship. Address reprint requests to Qian Lu, PhD, MD, Pediatric Pain Program, Department of Pediatrics, David Geffen School of Medicine at UCLA, 10940 Wilshire Blvd, Suite 1450, Los Angeles, CA 90024. E-mail: qlu@ucla.edu 1526-5900/$32.00 © 2007 by the American Pain Society doi:10.1016/j.jpain.2007.04.005 708 toms on coping strategies, laboratory pain studies have the advantage of controlling the administration of painful stimuli across participants. The recent development of the Pain Coping Questionnaire (PCQ)27 provides a standardized instrument to assess how children cope with pain. Only 1 study25 has examined how pre-existing coping strategies assessed by the PCQ predicted laboratory pain responses in children. However, this study excluded the subscales of the PCQ, which assessed behavioral distraction and seeking social support, and these constructs represent potentially important aspects of pain-related coping. The PCQ contains 3 higher-order factors and 8 subscales. Avoidance coping includes 2 subscales (catastrophizing and externalizing); approach coping includes 4 subscales (information seeking, problem solving, positive selfstatement, and seeking social support); and distraction ORIGINAL REPORT/Lu et al Figure 1. Theoretical model of coping and laboratory pain outcomes. Solid line indicates hypothesized positive association between coping and pain responsivity and the dotted line indicates hypothesized negative association between coping and pain responsivity. No hypothesized associations were advanced for the coping subscales of externalizing, information seeking, and problem solving. Note that increased pain responsivity is indicated by lower pain tolerance, higher pain intensity, and unpleasantness. coping includes 2 subscales (behavioral distraction and cognitive distraction) (Fig 1). Overwhelming evidence suggest that behavioral and cognitive distraction copings are associated with reduced pain,1,5,6,19 whereas catastrophizing is associated with increased pain.17,28,29 Some preliminary evidence suggests that positive selfstatements, which represent an active strategy of affirming “everything will be ok” was associated with less pain among children with juvenile idiopathic arthritis32; seeking emotional support, which might represent a passive strategy for attempting to get sympathy by amplifying pain or worries,36 was associated with higher headache severity in schoolchildren1 and higher emotional distress in children experiencing pain associated with rheumatologic diseases.35 Mixed findings have been reported for information seeking, problem solving,1,33 and externalizing.1,5,32 Despite evidence supporting the existence of 3 higher-order PCQ factors,27 the above results highlight the need to examine individual PCQ subscales in studies on children’s pain coping. As noted above, only 1 prior study25 has examined the relationship between the PCQ subscales and laboratory pain responses in children. Not only were key PCQ subscales excluded, only 1 aspect of the pain response, pain tolerance, was examined in this earlier study. Pain intensity and pain unpleasantness are important dimensions of pain responsivity that may be separately influenced by various psychological factors.26 We have previously demonstrated age and sex differences in laboratory pain responses20 and, therefore, it was important to examine whether the PCQ subscales explained additional variance above and beyond age and sex. The current study thus examined the associations between the 8 individual PCQ subscales and pain 709 tolerance, intensity and unpleasantness of 3 different types of laboratory pain stimuli (cold, heat, pressure) in a sample of healthy children, controlling for child age and sex. We assessed pain tolerance rather than pain threshold because our pilot work revealed that the assessment of pain threshold interfered with children’s natural coping style by influencing them to attend to the painful stimuli. It was hypothesized that for all 3 types of pain stimuli: 1) internalizing/catastrophizing and seeking emotional support would predict increased pain responses (ie, lower pain tolerance, and higher pain intensity and unpleasantness), and 2) positive selfstatements and behavioral/cognitive distraction would predict lower pain responses. In light of the mixed findings to date, we explored the associations between pain responsivity and the remaining 3 coping strategies (ie, externalizing, problem solving, and information seeking). Methods Participants The University of California, Los Angeles (UCLA) Institutional Review Board (IRB) as well as the IRBs for recruitment sites approved all recruitment and study procedures. Participants were recruited from a major urban area through mass mailing, posted advertisements, and classroom presentations. Initial eligibility was confirmed by telephone: All 489 individuals were screened for eligibility by telephone; 17 children (3.5% of those screened) were excluded due to ongoing acute or chronic illness, or use of medications that could affect study outcomes. Of the 472 (96.5%) invited to participate, 228 (48%) declined participation mainly because of parental lack of interest (54%) or time (21%). In total, 244 healthy children (124 female; 50.8%) with a mean age of 12.73 years (SD ⫽ 2.98 years; range, 8 –18 years) participated in the study. The average ages of males and females were 12.44 years (SD ⫽ 2.89) and 13.01 years (SD ⫽ 3.05 years), respectively. The ethnic composition of the sample was 40.2% Caucasian, 23.8% Hispanic, 13.9% African-American, 9.8% Asian-American, and 12.3% other. Parent socioeconomic status14 was: Unskilled workers 3.7%, semi-skilled workers 4.1%, clerical/sales 11.9%, technical 41.8%, and professional 34.8%. Overview of Procedure The UCLA IRB approved all study procedures. Both parents and children were informed by an experimenter about the study, which was described as an investigation on how children experienced pain. Parents and children signed consent and assent forms, respectively. Participants received a $30 video store gift certificate and a t-shirt for their participation. On the day of the laboratory session, participants and their parents were greeted by an experimenter and escorted to separate rooms; there was no contact between them until after the session was finished. After participants completed ques- 710 tionnaires (described below) in a quiet room, they were escorted individually to the laboratory. Participants were instructed on the use of the visual analog scales (VAS) for rating pain intensity and unpleasantness (see below for detailed descriptions). Participants were then exposed to 3 pain tasks: Pressure, heat, and cold pressor. For pressure and heat pain tasks we used 2 sites to avoid local sensitization or habituation, and we used 2 magnitudes of stimulus to allow for greater variation in pain response. Each pressure and heat pain task included 4 trials presented separately in counterbalanced order (setting and site of exposure) across participants. The cold pressor tasks consisted of 1 trial with a 1 minute informed ceiling (CPT-1) and 1 trial with a 3 minute uninformed ceiling (CPT-3). The CPT-3 has been discussed elsewhere34 and this paper focused on CPT-1. Before the start of each trial, subjects were informed that they would experience moderate sensation that might eventually be perceived as pain. Participants were instructed to continue with the task for as long as they could and to remove their finger or arm from the apparatus at any time during the procedures if it became too uncomfortable or painful. All tasks were extensively piloted on volunteers in the targeted age range. Coping Predictors of Children’s Laboratory Pain quickly and will cause some discomfort. Keep your arm on the spot as long as you can, but you are free to remove your arm at anytime.” Cold Pressor Task (CPT-1) Participants underwent a trial of 10°C water using a commercial ice chest measuring 38 cm wide, 71 cm long, and 35 cm deep. A plastic mesh screen separated crushed ice from a plastic large-hole mesh armrest in the cold water. Water was circulated through the ice by a pump to prevent local warming about the hand. Participants were instructed to keep the dominant hand in cold water to a depth of 2 inches above the wrist for as long as they could for an informed 1-minute period. Participants were instructed, “In this cooler is cold water. I am going to ask you to put 1 hand in the water and to keep it in for as long as you possibly can. When you put your hand in, do it with the palm of your hand facing up towards the ceiling, so that the back of your hand lays flat against the surface of the grate. I am going to ask you to leave your hand in for 1 minute. I will tell you when the time is up. When the time is up, you will take your hand out of the water. Try to keep your hand in until I tell you to take it out, but, if you need to, you can take it out before I tell you to.” Laboratory Pain Tasks Pressure Task The Ugo Basile Analgesy-Meter 37215 (Ugo Basile Biological Research Apparatus, Comerio, Italy) was used to administer focal pressure through a lucite point approximately 1.5 mm in diameter to the second dorsal phalanx of the middle finger and index finger of each hand. Four trials, 2 at each of 2 levels of pressure (322.5 g and 465 g), were run with an uninformed ceiling of 3 minutes. A comparable device has been used in healthy and clinical pediatric samples (ages 5–17 years) without adverse effects.7 Participants were instructed as follow: “During this task you will experience pressure on your finger. When I ask you to, you will place either your index or middle finger and the location onto this flat surface and I will lower this point onto your finger. The point should contact your finger at the spot I marked earlier. Leave your finger in place for as long as you can but you are free to remove the weight at any time. To remove the weight, lift this lever up like so.” Thermal Heat Task The Ugo Basile 7360 Unit (Ugo Basile Biological Research Apparatus) was used to administer a total of 4 trials of 2 infrared stimulus intensities15,20 of radiant heat 2 inches proximal to the wrist and 3 inches distal to the elbow on both volar forearms with an uninformed ceiling of 20 seconds. Thermal pain tolerance was electronically measured with an accuracy of 0.1 seconds. A similar task has been used in a sample aged 6 to 17 years without adverse effects.22 Participants were instructed as follow: “This part of the experiment will involve heat. When you are ready, you will place your forearm over a small spot on this metal block. This spot will heat up Laboratory Pain Measures Pain Tolerance Pain tolerance was defined as time in seconds elapsed from the onset of the pain stimulus to the participant’s withdrawal from the stimulus. Tolerance was measured for all 3 tasks (pressure, thermal heat, and cold). Pain Intensity and Pain Unpleasantness Pain intensity and pain unpleasantness were assessed through a vertical sliding visual analogue scale (VAS) immediately after each trial. The VAS is brief, easily understood, and sensitive to changes in pain. With excellent psychometric properties,11 it can be used by children in the age range included in the current study (8 –18 years of age).21 Prior research has used the VAS to rate pain in children in laboratory pain tasks.23 Participants were asked to rate their pain using the slider VAS, which was anchored with 0 at the bottom and 10 at the top. The scale also had color cues, graded from white at the bottom to dark red at the top, as well as a neutral face at the bottom and a negative facial expression at the top. Participants were given the following instructions regarding the use of VAS. “This scale is like a thermometer, only rather than measure your temperature; we will use it to measure your feeling or mood. The white color on the bottom represents the lowest values and the dark red at the very top represents the highest values for a particular feeling. By using this thermometer you’ll let me know how much pain or discomfort you feel. You will do this by sliding the bar up and down on the colors until you get to the shade that equal how you feel.” Three practice ratings were completed to ensure that participants understood the ORIGINAL REPORT/Lu et al VAS. The practice trials asked: (1) “How afraid or nervous would you be right before taking an important exam or test?’’ (2) “How much would it bother you to eat your favorite dessert?’’ (3) “How afraid, nervous, or worried do you feel right now?’’ The instructions and practice trials were repeated until participants fully understood the VAS. Pain intensity. Immediately after each trial, participants were asked to use the VAS and rate the amount of pain they experienced during the task. Participants were asked, “At its worst, how much pain did you feel?” during the task. Pain unpleasantness. Immediately after each trial and after rating the pain intensity, participants were also asked to rate the amount of distress or bother they experienced during the task using the same vertical sliding VAS. This time, participants were asked, “at its worst, how much did the task bother you?” Questionnaire Measure: Pain Coping Strategies Pain coping strategies were measured using the PCQ.27 Children completed the PCQ with respect to how they dealt with general pains that lasted a few hours or days by rating the frequency of how often each coping strategy was used ranging from “never ⫽ 1”, “hardly ever”, through “sometimes”, “often”, to “very often ⫽ 5.” The PCQ is a 39-item questionnaire that was developed and validated in relation to self-report responses to questionnaires and dolorimeter pressure pain threshold with samples of children age 8 and older. It has 8 subscales: 1) seeking social support with a focus on seeking emotional support and empathy (5 items, “let my feelings out to a friend”), 2) information seeking (4 items, eg, “find out more information”), 3) problem solving (6 items, eg, “figure out what I can do about it”), 4) positive selfstatements (5 items, eg, “say to myself, things will be ok”), 5) behavioral distraction (4 items, eg, “do something fun”), 6) cognitive distraction (5 items, “ignore the situation”), 7) externalizing (5 items, eg, “get mad and throw or hit something”), and 8) internalizing/catastrophizing (5 items, eg, “worry that I will always be in pain”). Statistical Analysis Independent sample t tests were used to examine mean differences in the PCQ subscales between boys and girls. Bivariate analyses were used to preliminarily examine relationships among the variables before multivariate modeling. Pearson product moment correlation coefficients were generated to explore the associations between the 8 PCQ subscales and the laboratory pain responses. In confirmatory analyses, sequential linear regression was used to predict pain outcomes from the 8 PCQ subscales simultaneously, controlling for age and sex. The demographic variables (age and sex) were entered as predictors in the first step (Step 1) of the regression analyses, followed by the 8 coping subscales together in the second step (Step 2). Adjusted R2 is reported for model fit (note that adjusted R2 is a more 711 2 stringent criterion than R to determine model fit because adjusted R2 can decline in value if the contribution to the explained variance by the additional variable is less than the impact on the increased degrees of freedom). R2 increments from Step 1 to Step 2 were reported to show the additional variance explained by the coping predictors above and beyond the effects of age and sex (note that the R2 increments are the difference of the unadjusted R2 between the 2 steps). A standard ␣ level of .05 (two-tailed) was used to evaluate the preliminary bivariate results. Bonferroni-Holm step-down test15 was used to reduce the likelihood of Type I error associated with conducting the confirmatory multiple regression tests. We ordered the P values for all the regression models from lowest to highest, and then compared these P values with corresponding critical values of ␣ according to the Bonferroni-Holm step-down test (these values were indicated in Table 3). Critical cutoff values of ␣ were calculated using this formula, ␣ ⫽ 0.05/k, and k ⫽ n, n-1, n-2, n-3 . . ., 1 (n ⫽ the total number of regression models). If the P value was less than the critical value, then null-hypothesis would be rejected and the next P value would be compared with the next critical value. If the P value was larger than the critical value, the null-hypothesis would not be rejected, and comparison would be stopped. Pain intensity ratings for the thermal and pressure tasks were highly correlated across the 4 trials within each task (r’s ⫽ .71–.89, P ⬍ .001). Pain unpleasantness ratings for the thermal and pressure tasks were highly correlated across the 4 trials within each task (r’s ⫽ .72–.88, P ⬍ .001). Pain tolerance for the thermal and pressure tasks were also highly correlated across the 4 trials within each task (r’s ⫽ .55 –.78, P ⬍ .001). Therefore, these data were averaged across trials yielding a single mean rating for pressure intensity, heat intensity, pressure unpleasantness, heat unpleasantness, pressure tolerance, and heat tolerance, respectively. Outliers and distributions of the dependent variables were examined before multivariate modeling. The number of participants that reached the tolerance ceiling for the pressure, heat, and cold tasks were 1, 20, and 79, respectively. Given the large number of participants who reached the ceiling in the heat and cold tasks (20 and 79, respectively), additional analysis was conducted to examine predictors of pain tolerance in a subset of the sample who did not reach ceiling, as well as predictors of whether or not ceiling was reached. The results using the whole sample were confirmed in the subset that did not reach ceiling as well as in the analysis for predicting whether ceiling was reached or not. Pressure pain tolerance was not normally distributed and therefore a log transformation was used to normalize the distribution. Furthermore, cases were monitored for undue influence on the final models; however, none were determined to have standardized residuals in excess of 3 standard deviations. Residuals for all models were normally distributed. 712 Coping Predictors of Children’s Laboratory Pain Table 1. Descriptive Statistics of Laboratory Pain Responses and PCQ Subscales With Reliabilities of PCQ Subscales Seeking emotional support Information seeking Problem solving Positive self-statements Behavioral distraction Cognitive distraction Externalizing Internalizing/catastrophizing Mean pressure tolerance Mean heat tolerance Cold tolerance Mean pressure VAS intensity Mean heat VAS intensity Cold VAS intensity Mean pressure VAS unpleasantness Mean heat VAS unpleasantness Cold VAS unpleasantness N MINIMUM MAXIMUM MEAN STD. DEVIATION RELIABILITY 242 242 242 242 242 242 242 242 239 240 239 239 240 240 187 188 188 1.00 1.00 1.00 1.00 1.00 1.00 1.00 1.00 2.22 1.05 0.83 0.00 0.00 0.00 0.00 0.00 0.00 5.00 5.00 5.00 5.00 5.00 5.00 5.00 4.60 180.00 20.00 60.00 9.76 9.76 10.00 9.76 9.76 9.76 3.03 2.63 3.32 3.22 3.47 3.24 1.63 1.93 40.27 10.77 47.77 4.87 4.99 3.97 3.49 3.48 3.23 1.03 0.94 0.94 0.92 0.88 0.87 0.69 0.73 45.71 5.14 17.09 2.60 2.77 3.08 2.62 2.69 2.97 0.83 0.42 0.74 0.85 0.83 0.82 0.76 0.75 — — — — — — — — — NOTE: Unpleasantness VAS was not administered until after the study started and thus, the n for the pain unpleasantness ratings is smaller than the other measures. Tolerance is in seconds. Results Descriptive Statistics for PCQ Subscales and Laboratory Pain Responses Table 1 shows descriptive statistics of laboratory pain responses and the PCQ subscales including the reliability of each of the subscales. Overall, the PCQ subscales were reliable, with Cronbach’s ␣ ranging from 0.74 – 0.83, except for the information seeking subscale with Cronbach’s ␣ of 0.42. Note that pain unpleasantness VAS was not administered until after data collection was underway and thus, the n for the pain unpleasantness ratings is smaller than that for the other measures. Age and Sex Differences in PCQ Subscales Older participants were more likely to use more problem-solving and externalizing coping strategies than Table 2. younger participants. The associations between age and problem solving, and age and externalizing were r ⫽ .22 (P ⬍ .001), and r ⫽ .16 (P ⫽ .02), respectively. However, there were no significant correlations between age and the other PCQ subscales. Independent sample t tests were used to examine mean differences in the PCQ subscales between boys and girls. Females were more likely to use seeking emotional support as a coping strategy than males (t ⫽ 5.02, P ⬍ .001, df ⫽ 240). No sex differences were found in the other 7 PCQ subscales. Exploration of Bivariate Correlations Between Coping Subscales and Laboratory-Induced Pain Outcomes Bivariate analyses were used to preliminarily examine relationships among the variables before multivariate modeling. Table 2 shows the significant correla- Bivariate Correlations Between PCQ Subscales and Laboratory Pain Response PCQ SUBSCALES Internalizing/catastrophizing Seeking emotional support Positive self-statements Behavioral distraction Cognitive distraction PRESSURE PAIN TOLERANCE PRESSURE PAIN INTENSITY HEAT PAIN INTENSITY 0.23* 0.28* COLD PAIN INTENSITY 0.24* HEAT PAIN UNPLEASANTNESS COLD PAIN UNPLEASANTNESS 0.20† 0.27* ⫺0.23* ⫺0.15‡ ⫺0.17‡ ⫺0.16‡ ⫺0.16‡ ⫺0.13‡ ⫺0.17† 0.13‡ ⫺0.14‡ NOTE: n ⫽ 237 for correlations involving pain tolerance, n ⫽ 238 for correlations involving pain intensity, n ⫽ 187 for correlations involving pain unpleasantness. Heat and cold pain tolerance and pressure pain unpleasantness are not shown in the table because of their nonsignificant associations with pain coping strategies. Information seeking, problem solving, and externalizing are not shown in the table because of their nonsignificant associations with pain responses. *P ⬍ .001. †P ⬍ .01. ‡P ⬍ .05. ORIGINAL REPORT/Lu et al 713 Sequential Multiple Regression of Sex, Age, and PCQ Subscales on Laboratory Pain Response Outcomes Table 3. Dependent Variables Predictors (B) (Independent Variables) Step 1 Age Sex Step 1 - Adjusted R2 Step 2 Internalizing/catastrophizing Seeking emotional support Positive self-statements Behavioral distraction Step 2 - Adjusted R2 Critical values of ␣ Step1-2: R2 increments PRESSURE PAIN TOLERANCE PRESSURE PAIN INTENSITY HEAT PAIN INTENSITY COLD PAIN INTENSITY HEAT PAIN UNPLEASANTNESS 0.38* 0.20* 0.17* ⫺0.30* ⫺0.34* ⫺0.25* 0.09* 0.11* 0.05† 0.25* 0.23* 0.22† COLD PAIN UNPLEASANTNESS 0.23† ⫺0.26† ⫺0.19‡ 0.16‡ 0.20* 0.008 0.06‡ 0.14* 0.012 0.08† ⫺0.19‡ 0.18* 0.01 0.10* 0.05† 0.025 0.09† ⫺0.18‡ ⫺0.21‡ 0.10* 0.017 0.09‡ 0.07‡ 0.05 0.12† NOTE: Only significant predictors are shown in the table.  ⫽ standardized regression coefficient; Adjusted R2 ⫽ goodness of fit for overall regression model taking into account of the number of independent variables; R2 increments ⫽ incremental contribution of the eight coping subscales to R2 in the total set of independent variables (ie, the variance explained by these 8 coping subscales on pain above and beyond age and sex). For sex, girls and boys were coded as 0 and 1, respectively. Critical values of ␣ were determined following the Bonferroni-Holm step-down method. All 6 models had P values lower than the critical values of ␣. *P ⬍ .001. †P ⬍ .01. ‡P ⬍ .05. tions between the PCQ subscale scores and the laboratory pain outcome variables. Pressure tolerance was positively associated with behavioral distraction and negatively associated with seeking emotional support. For pain intensity, internalizing/catastrophizing was positively associated with pain intensity for all 3 tasks; positive self-statements was negatively associated with pressure and cold pain intensity; and cognitive distraction was negatively associated with heat pain intensity. For pain unpleasantness, whereas internalizing/ catastrophizing was positively associated with heat and cold pain unpleasantness, behavioral distraction was negatively associated with pain unpleasantness for the same 2 tasks; positive self-statements and cognitive distraction were both negatively associated with cold pain unpleasantness. Information seeking, problem solving and externalizing subscales were not significantly related to pain responses. Three of the pain outcomes (ie, pain tolerance for heat and cold, or pain unpleasantness for pressure) were not associated with any coping subscales, and thus were eliminated from multivariate analysis. Multivariate Analysis: Coping Predictors of Children’s Pain Tolerance, Intensity, and Unpleasantness Based on the bivariate findings, the 6 pain outcomes (pressure tolerance, pain intensity for pressure, cold and heat tasks, and pain unpleasantness for cold and heat tasks) that showed significant correlations with the PCQ subscale(s) were examined in separate regressions in confirmatory analyses. Sequential linear regression was used to predict each of the 6 pain outcomes from the 8 PCQ subscales simultaneously, controlling for age and sex. Pain Tolerance Dependent variable pressure pain tolerance was regressed onto age and sex in Step 1, followed by the 8 coping subscales in Step 2. The PCQ subscales together explained 6% of the variance in pressure pain tolerance above and beyond age and sex (Table 3). Examination of the individual PCQ subscales revealed that seeking emotional support predicted lower pressure pain tolerance whereas behavioral distraction predicted higher pressure pain tolerance, controlling for the other coping subscales, age, and sex. The other coping subscales did not significantly predict pressure pain tolerance. Older age predicted higher pain tolerance, regardless of whether or not coping strategies were taken into account. Consistent with our previous study, boys exhibited increased pressure pain tolerance than girls,20 but this relationship disappeared after coping subscales were taken into account. Pain Intensity Dependent variables pain intensity for all 3 pain tasks were regressed onto age and sex in Step 1, and additional 8 coping subscales in Step 2. The R2 increments from Step 1 to Step 2 were significant for all pain tasks. The coping subscales together explained 8% to 10% of the variance in pain intensity for these pain tasks above 714 Coping Predictors of Children’s Laboratory Pain and beyond age and sex (Table 3). Internalizing/ catastrophizing predicted higher pain intensity across all 3 tasks; positive self-statements predicted lower pain intensity for the pressure and cold task, controlling for the other coping subscales, age, and sex. The other coping subscales did not predict pain intensity. Older age predicted lower pain intensity for the pressure and heat tasks regardless of whether coping strategies were taken into account. Sex was not a significant predictor of pain intensity for any of the pain tasks. Pain Unpleasantness Dependent variables pain unpleasantness for the heat and cold were regressed onto age and sex in Step 1 and the 8 coping subscales in Step 2. The R2 increments from Step 1 to Step 2 were significant for both tasks. The coping subscales together explained 9% to 12% of the variance in pain unpleasantness for the heat and cold tasks above and beyond age and sex (Table 3). Internalizing/ catastrophizing predicted higher pain unpleasantness during the cold task; positive self-statements predicted lower pain unpleasantness during the cold task; and behavioral distraction predicted lower pain unpleasantness during the heat task, controlling for the other coping subscales, age, and sex. Older age predicted lower pain unpleasantness during the heat task regardless of whether coping strategies were taken into account; sex did not significantly predict pain unpleasantness for the pain tasks. Discussion We hypothesized 1) internalizing/catastrophizing and seeking emotional support would predict increased pain responses, and 2) positive self-statements and behavioral and cognitive distraction would predict reduced pain responses (Fig 1). Our hypotheses were partially confirmed in that internalizing/catastrophizing predicted higher pain intensity across all 3 pain tasks (ie, cold, heat, and pressure) and higher cold pain unpleasantness; seeking emotional support was associated with lower pressure pain tolerance; positive self-statements was associated with lower pressure and cold pain intensity as well as lower cold pain unpleasantness; and behavioral distraction was associated with higher pressure pain tolerance and lower heat pain unpleasantness (Fig 2). The PCQ subscales explained 6% to 12% of variance in pain responsivity above and beyond age and sex. Although the amount of variance would appear to be small, the effect sizes for the PCQ subscales ranged from 0.5 to 0.75 (Cohen’s d), corresponding to a medium to large effect according to Cohen’s guidelines (d ⫽ 0.5 to 0.8).2 It has been suggested that different coping strategies may serve either as risk factors for, or as protective factors against, a poor pain outcome.35 The current findings support the notion that internalizing/catastrophizing and seeking emotional support are pain-prone/pain-risk factors, and positive self-statements and distraction are Figure 2. Associations between coping subscales and pain responsivity. Solid line indicates positive association between coping and pain responsivity and the dotted line indicates negative association between coping and pain responsivity. Note that increased pain responsivity is indicated by lower pain tolerance, higher pain intensity and unpleasantness. pain-protective factors within the context of acute laboratory-induced pain. The communal Coping Model proposes that pain catastrophizers may engage in more intense pain expression in order to solicit support or empathy from their social environment,30,31 and solicitous responses from others may serve to trigger, to maintain, or to reinforce the more intense pain expression of catastrophizers.30 An earlier study has shown that children displayed more intense pain expression to elicit parent support in the presence of parents during painful medical procedures.10 Our study demonstrated that even without parents’ presence, children with tendencies of seeking emotional support were more likely to exhibit lower pain tolerance, possibly due to habitual behavior of more intense pain expression. However, the meaning of seeking emotional support might depend on the nature of pain and the social or familial context within which pain is experienced, as suggested by a study that revealed that seeking emotional support predicted decreased distress in adolescents with chronic pain.5 The nature of pain might also influence the links between pain responsivity and other coping strategies, such as information seeking, problem solving, and externalizing, which might be more relevant when pain is chronic or lasting to allow individuals enough time to engage in these coping strategies. Thus, the findings in our study might have more relevance for children’s coping with acute pain in clinical settings, such as procedural pain in primary care settings or in the emergency department. The association between positive self-statements coping and reduced pain was consistent with previous findings in a clinical sample.32 By reassuring oneself, “be strong” “everything will be ok,” and “I can handle anything that happens,” those who engage in positive selfstatements might increase perceived control and thus reduce anxiety and pain perception.12,16 In a previous study, direct efforts to maintain control were found to ORIGINAL REPORT/Lu et al be the most frequently used coping strategy among children during medical procedure.13 The use of positive self-statements may be a promising skill to be taught to children who undergo painful medical procedures. Behavioral distraction predicted lower pain responses for pressure and heat pain, a finding consistent with a meta-analysis on the effects of distraction on children’s responses to painful medical procedures.19 The metaanalysis revealed that distraction had a modest effect on reducing children’s distress behavior (eg, crying, whimpering, fighting) and a larger but more variable effect on reducing children’s self-report of pain. In contrast, our nonsignificant findings for cognitive distraction are inconsistent with the study by Piira et al,25 who found that cognitive distraction was associated with greater cold pressor tolerance. Piira et al’s study tested the partial correlation between cognitive distraction and pain tolerance, controlling for pain threshold, whereas we tested the independent effect of cognitive distraction, controlling for the other PCQ subscales as well as age and sex. In fact, our bivariate correlation results suggested that cognitive distraction was associated with pain intensity and unpleasantness; however, the associations were not robust, and disappeared in the multivariate tests. The behavioral distraction items include “do something fun” and “do something I enjoy,” whereas the cognitive distraction items include “try to forget it” and “ignore the situation.” Perhaps behavioral distraction with a focus on “fun” is more effective than cognitive distraction with a focus on “ignoring or avoiding.” Indeed, recent studies suggest that cartoon TV and video games that are fun and enjoyable for children may be promising and effective distraction methods for painful medical procedures.3,4,9 Conversely, the PCQ cognitive distraction items are representative of an avoidant approach coping style associated with more pain-related disability in children with recurrent abdominal pain.33 Older children exhibited greater pressure pain tolerance, lower pressure and heat pain intensity, and lower heat pain unpleasantness, findings that are consistent with our previous study.20 Older children may be better able than younger children to understand that experimental pain is temporary, and thus less threatening. Older children may have more experience with more intensely painful events and understand that much more painful events are possible than those administered in this study. This experience/knowledge may have influenced their ratings of the pain tasks on a VAS scale. Older children may also have a larger repertoire of coping strategies to assist them in tolerating the tasks longer than younger children and finding them less aversive.25 We found that older age was related to increased use of problem solving and externalizing coping; however, these coping strategies did not seem to be associated with laboratory pain responsivity. Girls exhibited less pressure pain tolerance than boys, and they also were more likely to use seeking emotional 715 support coping than boys, a finding consistent with a recent study of adolescent chronic pain sufferers.18 Interestingly, seeking emotional support was also linked to lower pressure tolerance. These findings point to the possibility that seeking emotional support might play a role in sex difference in pressure pain tolerance. Gender role socialization results in sex-differentiated reinforcement and punishment for girls and boys with regard to seeking social support when in pain,24 which may contribute to our present findings. A mediation analysis in a future study, however, will shed additional light on this issue. Several caveats to the current findings should be mentioned. The present data are cross-sectional and, therefore, conclusions regarding causality cannot be inferred. Administrating the PCQ before the laboratory tasks also subjects the findings to an order effect. The PCQ could potentially change participants’ reaction to pain because they were alerted to ways of coping. Counterbalancing the order of PCQ and pain tasks is recommended in future studies. Another limitation is that the PCQ measures children’s ways of dealing with naturally-occurring pain in a retrospective manner. Future studies should examine models incorporating trait measures of coping strategies to deal with chronic pain in real life in combination with momentary coping strategies to deal with laboratory-induced pain as well as clinical acute pain situations. We do not have a clear explanation for why certain PCQ subscales were associated with certain pain responses for 1 type of pain stimulation but not others. Perhaps distinctive temporal, sensory, or affective characteristics of the pain stimuli contribute to the lack of uniformity in findings. Future studies of momentary coping strategies might also help clarify why associations between coping and pain response differed by types of pain stimulation. Finally, while our analyses revealed statistically significant relationships between coping strategies and pain responses in a controlled laboratory environment, it remains to be tested whether findings regarding coping in the pain laboratory will generalize to coping in clinical pain contexts. In sum, our findings support the maladaptive role of catastrophizing and seeking sympathy from others when coping with acute pain, and the adaptive role of distraction and positive self-statements. Distraction has been extensively studied in interventions for clinical samples and shown to be effective at reducing acute pain.6,19 However, few intervention studies have focused on other coping strategies. The relationships that were found between coping and laboratory pain responses provide support for the potential use of laboratory pain tasks to teach new coping strategies for acute pain, as has been done previously for children with recurrent pain.8 Further studies are warranted to examine whether interventions aimed at modifying coping in the direction of reduced seeking of emotional support, reduced emotional avoidance and internalization/catastrophizing, and enhanced use of 716 positive self-statements may lead to reductions in children’s pain responses to acute pain stimuli such as those that are encountered during routine medical procedures. References 1. Bell-Hoekstra IENG, Abu-Saad HH, Passchier J, Frederiks CMA, Feron FJM, Knipschild P: Coping and Quality of Life in relation to headache in Dutch schoolchildren. Eur J Pain 6:315, 2002 2. Cohen J: Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Erlbaum; 1988 3. Cohen LL, Blount RL, Panopoulos G: Nurse Coaching and cartoon distraction: An effective and practical intervention to reduce child, parent, and nurse distress during immunizations. J Pediatr Psychol 22:355-370, 1997 4. Das D, Grimmer K, Sparnon A, McRae S, Thomas B: The efficacy of playing a virtual reality game in modulating pain for children with acute burn injuries: A randomized controlled trial [ISRCTN87413556]. BMC Pediatrics 5:1, 2005 5. Eccleston C, Crombez G, Scotford A, Clinch J, Connell H: Adolescent chronic pain: Patterns and predictors of emotional distress in adolescents with chronic pain and their parents. Pain 108:221, 2004 6. Fernandez E, Turk DC: The utility of cognitive coping strategies for altering pain perception: a meta-analysis. Pain 38:123, 1989 7. Gil KM, Edens JL, Wilson JJ, Raezer LB, Kinney TR, Schultz WH, Daeschner C: Coping strategies and laboratory pain in children with sickle cell disease. Annu Behav Med 19:22-29, 1997 8. Gil KM, Wilson JJ, Edens JL, Workman E, Ready J, Sedway J, Redding-Lallinger R, Daeschner CW: Cognitive coping skills training in children with sickle cell disease pain. Int J Behav Med 4:364-377, 1997 9. Gold JI, Kant AJ, Kim SH, Rizzo AS: Virtual anesthesia: The use of virtual reality for pain distraction during acute medical interventions. Semin Anesth Perioperative Med Pain 24: 203, 2005 10. Gonzalez JC, Routh DK, Saab PG, Armstrong FD, Shifman L, Guerra E, Fawcett N: Effects of parent presence on children’s reactions to injections: Behavioral, physiological, and subjective aspects. J Pediatr Psychol 14:449-462, 1989 Coping Predictors of Children’s Laboratory Pain Acknowledgments We thank Norman Turk for his contribution to data management. 16. Jensen MP, Turner JA, Romano JM, Karoly P: Coping with chronic pain: A critical review of the literature. Pain 47:249, 1991 17. Keefe FJ, Lefebvre JC, Egert JR, Affleck G, Sullivan MJ, Caldwell DS: The relationship of gender to pain, pain behavior, and disability in osteoarthritis patients: The role of catastrophizing. Pain 87:325, 2000 18. Keogh E, Eccleston C: Sex differences in adolescent chronic pain and pain-related coping. Pain 123:275, 2006 19. Kleiber C, Harper DC: Effects of distraction on children’s pain and distress during medical procedures: A meta-analysis. Nurs Res 48:44-49, 1999 20. Lu Q, Zeltzer LK, Tsao JCI, Kim SC, Turk N, Naliboff BD: Heart rate mediation of sex differences in pain tolerance in children. Pain 118:185, 2005 21. McGrath PA, Gillespie J: Pain assessment in children and adolescents. In: Turk DC, Melzack R, eds. Handbook of pain assessment, 2nd Edition. New York: Guilford; 2001:97-118 22. Meier PM, Berde CB, DiCanzio J, Zurakowski D, Sethna NF: Quantitative assessment of cutaneous thermal and vibration sensation and thermal pain detection thresholds in healthy children and adolescents. Muscle Nerve 24:13391345, 2001 23. Miller A, Barr RG, Young SN: The cold pressor test in children: Methodological aspects and the analgesic effect of intraoral sucrose. Pain 56:175, 1994 24. Myers CD, Tsao JCI, Glover DA, Kim SC, Turk N, Zeltzer LK: Sex, gender, and age: Contributions to laboratory pain responding in children and adolescents. J Pain 7:556, 2006 25. Piira T, Taplin JE, Goodenough B, von Baeyer CL: Cognitive-behavioural predictors of children’s tolerance of laboratory-induced pain: Implications for clinical assessment and future directions. Behav Res Ther 40:571, 2002 26. Price DD: Central neural mechanisms that interrelate sensory and affective dimensions of pain. Mol Interv 2:392403, 2002 27. Reid GJ, Gilbert CA, McGrath PJ: The Pain Coping Questionnaire: Preliminary validation. Pain 76:83, 1998 11. Gragg RA, Rapoff MA, Danovsky MB, Lindsley CB, Varni JW, Waldron SA, Bernstein BH: Assessing chronic musculoskeletal pain associated with rheumatic disease: Further validation of the Pediatric Pain Questionnaire. J Pediatr Psychol 21:237-250, 1996 28. Spinhoven P, ter Kuile M, Kole-Snijders AMJ, Hutten Mansfeld M, den Ouden D-J, Vlaeyen JWS: Catastrophizing and internal pain control as mediators of outcome in the multidisciplinary treatment of chronic low back pain. Eur J Pain 8:211, 2004 12. Haythornthwaite JA, Menefee LA, Heinberg LJ, Clark MR: Pain coping strategies predict perceived control over pain. Pain 77:33, 1998 29. Sullivan MJL, Rodgers WM, Wilson PM, Bell GJ, Murray TC, Fraser SN: An experimental investigation of the relation between catastrophizing and activity intolerance. Pain 100: 47, 2002 13. Hodgins MJ, Lander J: Children’s coping with venipuncture. J Pain Sympt Manage 13:274, 1997 14. Hollingshead AB: Four-factor Index of Social Status. New Haven, CT, Department of Sociology, Yale University, 1975 15. Holm S: A simple sequentially rejective multiple test procedure. Scand J Statist 6:65-70, 1979 30. Sullivan MJL, Martel MO, Tripp D, Savard A, Crombez G: The relation between catastrophizing and the communication of pain experience. Pain 122:282, 2006 31. Sullivan MJL, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, Lefebvre JC: Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain 17:52-64, 2001 ORIGINAL REPORT/Lu et al 32. Thastum M, Herlin T, Zachariae R: Relationship of paincoping strategies and pain-specific beliefs to pain experience in children with juvenile idiopathic arthritis. Arthritis Care Res 53:178-184, 2005 33. Thomsen AH, Compas BE, Colletti RB, Stanger C, Boyer MC, Konik BS: Parent reports of coping and stress responses in children with recurrent abdominal pain. J Pediatr Psychol 27:215-226, 2002 34. Tsao JCI, Myers CD, Craske MG, Bursch B, Kim SC, Zeltzer LK: Role of anticipatory anxiety and anxiety sensitivity in 717 children’s and adolescents’ laboratory pain responses. J Pediatr Psychol 29:379-388, 2004 35. Varni JW, Waldron SA, Gragg RA, Rapoff MA, Bernstein BH, Lindsley CB, Newcomb MD: Development of the Waldron/Varni Pediatric Pain Coping Inventory. Pain 67:141, 1996 36. Walker LS, Smith CA, Garber J, Claar RL: Testing a model of pain appraisal and coping in children with chronic abdominal pain. Health Psychol 24:364, 2005