Role of Inhibitory Neurotransmitter
Interactions in the Pathogenesis of Neonatal
Apnea: Implications for Management
Richard J. Martin,* Christopher G. Wilson,* Jalal M. Abu-Shaweesh,*
and Musa A. Haxhiu†
pnea of prematurity remains a troublesome
clinical problem in the care of low birth
weight infants. It may significantly impact the neonatal course of such patients by necessitating the
use of assisted ventilation, prolonging their hospitalization, and resulting in a need for xanthine or
other pharmacologic intervention. To better understand the physiologic basis for neonatal apnea,
the response of respiratory neural output to hypercapnia, hypoxia, and stimulation of laryngeal and
other mechanoreceptor-mediated afferents has
been extensively studied in both human infants
and various animal models. However, maturation
of the role of neurotransmitters that mediate these
neural pathways at the brainstem is poorly understood. As fetal and early neonatal life are characterized by greater inhibition of respiratory output
than in later life, it is tempting to speculate that
this period is associated with greater expression of
inhibitory versus excitatory neurotransmitters and
neuromodulators in respiratory-related neurons. A
variety of such substances have been implicated in
neonatal respiratory control and some, such as
serotonin and adenosine, may have excitatory or
inhibitory effects depending on the receptor subtypes activated (Fig 1). Although prostaglandins
and endorphins have both been studied for their
role as inhibitory neurotransmitters in relation to
neonatal respiratory control,1 the focus of this review will be on gamma aminobutyric acid (GABA),
adenosine, and their potential interaction as the
major modulators of respiratory neural output in
early life.
cell hyperpolarization by opening ligand-operated ion channels2; slow synaptic transmission is
mediated via activation of GABAB receptors and
modulation of downstream signaling pathways.
GABAA receptors consist of five protein subunits, the “mix” of which differs during maturation.3,4 While essentially an inhibitor of neural
activity in the central nervous system, GABA may
produce excitatory responses in the immature
brain; however, such excitatory effects have not
been clearly observed in relation to neonatal
respiratory control. What is the evidence that
GABA plays a prominent role in inhibition of
respiratory neural output in early life? Such a
concept is consistent with the data of Xia and
Haddad that GABAA receptors appear very early
in maturation, especially in brainstem regions of
the developing rat brain.5
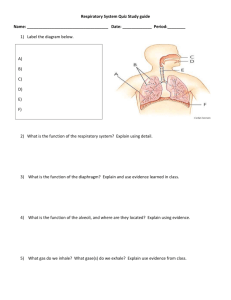
Part One
From the *Department of Pediatrics, Rainbow Babies & Children’s
Hospital, Cleveland, OH; and †Department of Physiology & Biophysics, Howard University, Washington, D.C.
This work is supported in part by NIH Grant HL 62527.
Address reprint requests to Richard J. Martin, MB, FRACP, Rainbow Babies & Children’s Hospital, 11100 Euclid Avenue, Cleveland, OH 44106-6010; e-mail: rxm6@cwru.edu
© 2004 Elsevier Inc. All rights reserved.
0146-0005/04/2804-0000$30.00/0
doi:10.1053/j.semperi.2004.08.004
A
GABA in Neonatal Respiratory Control
GABA is the major inhibitory neurotransmitter
in the mammalian central nervous system and
mediates its effects via fast and slow synaptic
transmission. In fast inhibitory transmission,
GABA binds to its GABAA receptor and results in
Role of GABA in Modulating Hypercapnic
Responses
Both prematurity and apnea are associated with
impaired ventilatory responses to hypercapnia in
human infants, in which the increase in tidal volume is associated with a progressive decrease in
frequency due to prolongation of expiratory time.6
In a series of studies in rat pups and piglets, we
sought to test the hypothesis that release of GABA
and activation of GABAA receptors contribute to
this phenomenon. In rat pups, we showed that
prolongation of expiration and slowing of breathing frequency, in response to hypercapnia, oc-
Seminars in Perinatology, Vol 28, No 4 (August), 2004: pp 273-278
273
274
Martin et al
Figure 1. Putative neurotransmitter/neuromodulator
regulators of neonatal respiratory control.
curred in 5-day-old, but not older (16 days and
beyond) animals.7 Furthermore, intravenous administration of the GABAA receptor blocker, bicuculline, eliminated hypercapnia-induced prolongation of expiration in the youngest animals. This
led us to conclude that centrally mediated prolongation of expiration during early postnatal life is
mediated via GABAergic inhibition of respiratory
timing mechanisms. A similar phenomenon was
observed in piglets exposed to hypercapnia, suggesting that this GABAergic effect on respiratory
timing is consistently observed in young animals
across species.8
These physiologic data are strengthened by our
neuroanatomic findings that hypercapnia actually
activates GABAergic neurons. In a series of experiments, we employed expression of c-Fos protein,
the product of an immediate early gene (c-Fos), to
localize CO2-activated cells within the piglet medulla oblongata.9 This gene is rapidly and transiently expressed following cell activation by different stimuli, including hypercapnia. It should be
noted that finding c-Fos expression in a subset of
neurons within respiratory-related medullary regions does not prove that these neurons are chemosensitive; however, it does indicate that they are
part of the CO2-chemosensitive network at that
site. After hypercapnic exposure (10% CO2 for 60
minutes) animals were killed, brains removed and
sectioned, and prepared for immunofluorescence.
As expected, CO2 elicited a significant increase in
c-Fos-expressing cells when compared with normocapnic controls.
Parvalbumin was then chosen as a marker for
GABAergic neurons to determine whether CO2
exposure elicited c-Fos expression in GABA-containing cells of the medullary network. Previous
work has shown that, at all developmental ages,
GABA-containing neuronal cell bodies, dendrites, and axonal terminals are parvalbumenimmunoreactive.10 Hence, parvalbumen expression can be used to define the organization of
GABAergic inhibitory circuits in the brain.11 Colocalization studies revealed that hypercapnia
significantly increased c-Fos expression in
GABA-containing neurons in the medulla oblongata, especially in the ventral aspect of the medulla, within the Bötzinger region, the gigantocellular reticular nucleus, and the caudal raphé
nuclei. An alternate approach, which we are pursuing, is the use of glutamic acid decarboxylase
(GAD) isoform staining as a marker for GABAergic neurons, as the GAD65 and GAD67 isoforms
are largely responsible for GABA production.
From these combined physiologic and neuroanatomic data, we propose that GABAergic neurons in the medullary network modulate the
ventilatory response to hypercapnia (Fig 2).
Thus, CO2 (potentially acting through interconnected glutamatergic neurons) excites respiratory output in parallel with GABAergic neurons
which may inhibit the firing of cells that modulate inspiratory rhythm generation. These and
future neuroanatomic observations, correlated
with physiologic data, should allow better definition of the role that this and other specific
neurotransmitter pathways play in modulating
neonatal respiratory control.
Role of GABA in Hypoxic Respiratory
Depression
Hypoxic exposure of many species in the newborn period results in a characteristic transient
Inhibitory Neurotransmitter Interactions and Neonatal Apnea
275
Figure 2. Schematic model
indicating the effect of increasing CO2 on the response of the neural network
regulating inspiratory drive
and respiratory timing. GLU,
glutamate. Reprinted with
permission.9
increase and subsequent decrease in respiratory
efforts, which is termed the biphasic ventilatory
response. Although the response of the respiratory system to single episodes of hypoxia of varying length has been extensively investigated in
humans as well as in anesthetized and unanesthetized animal species, studies have only recently begun to critically evaluate the effects of
recurrent hypoxia on respiratory neural output.
These studies are complicated by the fact that
responses appear to differ widely, dependent on
species studied, degree of maturation, confounding effects of anesthesia, and duration and
magnitude of hypoxic exposures. We employed
the anesthetized piglet model to begin to investigate the effects of recurrent hypoxia on respiratory neural output and whether GABA might
be implicated in any cumulative inhibition of
breathing induced by recurrent hypoxia. In re-
sponse to multiple exposures to 8% oxygen (5minute exposures, 10-minute recoveries) in 2- to
10-day-old animals, we observed that hypoxic
depression of phrenic neural output progressively increased with subsequent exposures.12
This progressive increase in hypoxic respiratory
depression could be largely reversed after intracisternal injection of the GABAA receptor
blocker bicuculline in the piglets (Fig 3). These
data suggest that central GABAergic inhibition
may contribute significantly to the cumulative
inhibitory effects of repeated hypoxia in the
newborn piglet model. It is unlikely that decreased peripheral chemoreceptor-mediated responses after recurrent hypoxic exposure contributed to these findings. Of interest in this
regard are the recent data of Prabhakar in mature rats that recurrent episodes of short duration hypoxia actually increase carotid body firing
Figure 3. The increase in
hypoxic ventilatory depression after recurrent hypoxia
was reversed by administration of bicuculline in piglets
ⱕ10 days of age (n ⫽ 7).
Hypoxic exposure 1, ●—●;
hypoxic exposure 6, 䊐—䊐;
hypoxic exposure after intracisternal bicuculline [40 g/
kg], ‚—‚. Reprinted with
permission.12
276
Martin et al
Figure 4. Effect of intravenous bicuculline on the
phrenic nerve frequency response to multiple levels of superior laryngeal nerve (SLN)
stimulation. SLN stimulation
caused a significant decrease
in phrenic nerve frequency
that was proportional to the
level of stimulation (P ⬍ 0.02).
Bicuculline attenuated the
decrease in phrenic nerve
frequency in response to
SLN stimulation (P ⬍ 0.05
between the two curves). Reprinted with permission.15
in response to subsequent hypoxic exposure,13
and the data of Nock and coworkers14 that preterm infants with more episodes of apnea actually exhibit greater increases in ventilation in
response to hypoxic exposure.
Role of GABA in Apnea Induced by Laryngeal
Stimulation
Stimulation of the laryngeal mucosa results in
apnea in humans as well as in animals of different species. This reflex apnea is mediated via
stimulation of the superior laryngeal nerve
(SLN), and is most prominent during early maturation. It has been suggested that an exaggerated reflex response in newborns may be implicated in multiple pathological processes,
including gastroesophageal reflux-induced apnea, sudden infant death syndrome, and apnea
of prematurity. We hypothesized that upregulation of inhibitory neurotransmitter-mediated
mechanisms in the immature brainstem might
explain the vulnerability of newborns to this reflex, and again, that GABA might be implicated.
In the unanesthetized 5- to 10-day-old piglet
model, we performed graded SLN stimulation
and measured phrenic neural output before and
after GABAA receptor blockade with intravenous
or intracisternal bicuculline. SLN stimulation
caused a significant decrease in phrenic nerve
amplitude, phrenic nerve frequency, minute
phrenic activity, and inspiratory time that was
proportional to the level of electrical stimulation.15 Increased levels of stimulation were more
likely to induce apnea during stimulation that
often persisted beyond cessation of the stimulus.
Bicuculline, administered intravenously or intracisternally, decreased the SLN stimulation-induced decrease in phrenic nerve amplitude,
minute phrenic activity, and phrenic nerve frequency (Fig 4). Bicuculline also reduced SLNinduced apnea and duration of poststimulation
apnea. These findings are consistent with our observations during hypercapnic and recurrent hypoxic exposure, and point to a prominent role for
GABA in the inhibitory timing mechanisms that
are an integral component of neonatal respiratory
reflex responses, and possibly apneic events.
Part Two
Adenosine in Neonatal Respiratory Control
A prominent role for adenosine in neonatal respiratory inhibition is suggested by the ability of
the nonspecific adenosine receptor antagonists,
theophylline and caffeine, to decrease the incidence of apnea of prematurity. Adenosine is a
product of nucleotides such as ATP, and is
formed as a consequence of metabolic and neural activity at many sites including the brain,
especially during hypoxia. Although four major
Inhibitory Neurotransmitter Interactions and Neonatal Apnea
adenosine receptor subtypes have been identified, the net effect of adenosine on neuronal
activity depends primarily on a balance between
activation of inhibitory A1 and excitatory A2 (especially A2A) receptors. It has been widely presumed that the stimulatory effects of caffeine are
secondary to A1 receptor blockade, and this appears to be the case in lambs.16 Studies implicating adenosine in hypoxia-induced respiratory
depression have employed primarily adenosine
analogues17 and nonspecific adenosine antagonists.18 Meanwhile, molecular techniques have
demonstrated widespread distribution of excitatory A2A receptor mRNA in mature and developing rat brain.19 Of particular interest are the
observations that adenosine A2A receptors are
expressed in GABA-containing striato-pallidal
neurons and that GABA-release may be regulated via A2A receptor activation.20,21 Based on
our earlier findings of a prominent role for
GABA in neonatal respiratory control, this led us
to speculate that GABA release may be a mechanism underlying the respiratory inhibitory effects mediated by adenosine in early postnatal
life.
Role of GABA in Mediating Adenosine-Induced
Respiratory Inhibition
In a series of preliminary experiments in 5- to
10-day-old piglets, we sought to test the hypothesis that adenosine inhibits respiratory drive at
this age via the selective activation of A2A receptors. This, in turn, causes activation of GABAergic inputs to the inspiratory drive center (preBötzinger complex and associated inspiratory
circuitry) located in the rostral ventrolateral medulla of the brainstem. In decerebrate animals
(to avoid the effects of anesthesia), we measured
phrenic neural output before and after intracisternal drug administration. Adenosine (5-50 L
of 10 or 50 mmol/L solution) invariably inhibited amplitude and frequency of phrenic neural
output, and eventually resulted in apnea.22 Intracisternally administered bicuculline (50 L)
blocked this effect (Fig 5).
Injection of the selective adenosine A2A receptor agonist (CGS21680, 50 L) also resulted
in brief apnea followed by respiratory inhibition.
Intracisternal bicuculline injection (50 L)
again blocked the respiratory inhibitory effects
of the adenosine A2A agonist. These physiologic
277
Figure 5. Adenosine inhibits phrenic nerve activity.
(A) Adenosine (5 L), injected intracisternally, results
in a pronounced apnea and inhibition of respiratory
frequency. (B) Bicuculline (50 L) blocks this effect.
Arrowheads and dashed lines indicate time of adenosine injection.
data, if supported by subsequent neuroanatomic
data, strongly suggest that respiratory inhibition
elicited by adenosine in this model may depend,
in part, on GABAergic inputs to the brainstem
inspiratory center.
Conclusion and Clinical Application
Xanthine therapy has been widely administered
to diminish the incidence of apnea of prematurity for nearly 30 years.23,24 While these drugs are
widely proven to increase central respiratory
neural output to the respiratory muscles—probably via adenosine receptor antagonism—the
precise mechanism whereby apnea is decreased
by xanthines is unknown. In fact, the wisdom of
such broad xanthine usage has been recently
challenged,25 and an international multicenter
randomized trial is currently testing the hypothesis that withholding such therapy may improve
the neurodevelopmental outcome of preterm
infants. Regardless of the outcome of that trial, it
is important to clarify the mode of action of this
therapy.
The data presented in this review provide
evidence for a prominent role for GABA in inhibiting respiratory neural output in early development. Such evidence is best assembled by
combining physiologic with neuroanatomic ex-
278
Martin et al
periments employing state-of-the-art experimental and molecular techniques. Perhaps more important, these data demonstrate the importance
of understanding neurotransmitter interactions
in elucidating the biologic basis of apnea in
preterm infants. In this way, it may be possible to
improve our pharmacologic interventions by developing specific, targeted approaches to the
clinical problem.
References
1. Milner AD, Lagercrantz H, Wickstrom R: Control of
breathing, Greenough A, Milner AD (ed): Neonatal Respiratory Disorders, 2nd ed London, UK, Arnold Health
Science, 2003, pp 37– 49
2. Greengard P: The neurobiology of slow synaptic transmission. Science 294:1024-1030, 2001
3. Seeburg PH, Wisden W, Verdoorn TA, et al: The GABAA
receptor family: Molecular and functional diversity. Cold
Spring Harbor Symp Quant Biol 55:29-40, 1990
4. Killisch I, Dotti CG, Lauri DJ, et al: Expression patterns
of GABAA receptor subtypes in developing hippocampal
neurons. Neuron 7:927-936, 1991
5. Xia Y, Haddad GG: Ontogeny and distribution of
GABAA receptors in rat brainstem and rostral brain regions. Neuroscience 49:973-989, 1992
6. Martin RJ, Carlo WA, Robertson SS, et al: Biphasic response of respiratory frequency to hypercapnia in preterm infants. Pediatr Res 19:791-796, 1985
7. Abu-Shaweesh JM, Dreshaj IA, Thomas AJ, et al: Changes
in respiratory timing induced by hypercapnia in maturing rats. J Appl Physiol 87:484-490, 1999
8. Dreshaj IA, Haxhiu MA, Abu-Shaweesh J, et al: CO2induced prolongation of expiratory time during early
development. Respir Physiol 116:125-132, 1999
9. Zhang L, Wilson CG, Liu S, et al: Hypercapnia-induced
activation of brainstem GABAergic neurons during early
development. Respir Physiol Neurobiol 136:25-37, 2003
10. Amadeo A, Ortino B, Frassoni C: Parvalbumin and
GABA in the developing somatosensory thalamus of the
rat: An immunocytochemical ultrastructural correlation.
Anat Embryol (Berl) 203:109-119, 2001
11. McDonald AJ, Betette RL: Parvalbumin-containing neurons in the rat basolateral amygdala: Morphology and
co-localization of Calbindin-D(28k). Neuroscience 102:
413-425, 2001
12. Miller MJ, Haxhiu MA, Haxhiu-Poskurica B, et al: Recurrent hypoxic exposure and reflex responses during development in the piglet. Respir Physiol 123:51-61, 2000
13. Peng Y-J, Overholt JL, Kline D, et al: Induction of sensory
long-term facilitation in the carotid body by intermittent
hypoxia: Implications for recurrent apneas. Proc Natl
Acad Sci 100:10073-10078, 2003
14. Nock ML, DiFiore JM, Arko MK, et al: Relationship of
the ventilatory response to hypoxia with neonatal apnea
in preterm infants. J Pediatr 144:291-295, 2004
15. Abu-Shaweesh JM, Dreshaj IA, Haxhiu MA, et al: Central
GABAergic mechanisms are involved in apnea induced
by SLN stimulation in piglets. J Appl Physiol 90:15701576, 2001
16. Koos BJ, Maeda T, Jan C: Adenosine A1 and A2A receptors modulate sleep state and breathing in fetal sheep.
J Appl Physiol 91:343-350, 2001
17. Runold M, Lagercrantz H, Fredholm BB: Ventilatory
effect of an adenosine analogue in unanesthetized rabbits during development. J Appl Physiol 61:255-258,
1986
18. Long WA, Lawson EE: Neurotransmitters and biphasic
respiratory response to hypoxia. J Appl Physiol 57:213222, 1984
19. Weaver DR: A2A adenosine receptor gene expression in
developing rat brain. Mol Brain Res 20:313-327, 1993
20. Ochi M, Koga K, Kurokawa M, et al: Systemic administration of adenosine A2A receptor antagonist reverses
increased GABA release in the globus pallidus of unilateral 6-hydroxydopamine-lesioned rats: A microdialysis
study. Neuroscience 100:53-62, 2000
21. Phillis JW: Inhibitory action of CDG 21680 on cerebral
cortical neurons is antagonized by bicuculline and picrotoxin: Is GABA involved? Brain Res 807:193-198, 1998
22. Wilson CG, Martin RJ, Jaber M, Abu-Shaweesh J, Jafri A,
Haxhiu MA, Zaidi S: Adenosine A2A receptors interact
with GABAergic pathways to modulate respiration in
neonatal piglets. Resp Physiol Neurobiol 141:201-206,
2004
23. Aranda JV, Sitar DS, Parsons WD, et al: Pharmacokinetic
aspects of theophylline in premature newborns. N Engl
J Med 295:413-416, 1976
24. Uauy R, Shapiro DL, Smith B, et al: Treatment of severe
apnea in prematures with orally administered theophylline. Pediatrics 55:595-598, 1975
25. Schmidt B: Methylxanthine therapy in premature infants: Sound practice, disaster or fruitless byway? J Pediatr 135:526-528, 1999