Journal of Perinatology (2006) 26, 67–70
r 2006 Nature Publishing Group All rights reserved. 0743-8346/06 $30
www.nature.com/jp
PERINATAL/NEONATAL CASE PRESENTATION
Neonatal respiratory failure associated with mutation in the
surfactant protein C gene
AS Soraisham, AJ Tierney and HJ Amin
Division of Neonatology, Department of Pediatrics, Foothills Medical Centre, University of Calgary, Alberta, Canada
We report on a term newborn with an unusual presentation and course of a
rare lung disease due to mutation in SFTPC gene. This particular SFTPC
mutation is novel, and the infant’s lung disease was unusually severe
compared to what has been previously reported in association with SFTPC
mutations.
Journal of Perinatology (2006) 26, 67–70. doi:10.1038/sj.jp.7211417
Keywords: neonate; respiratory distress; surfactant protein C
Introduction
Pulmonary surfactant is a complex mixture of phospholipids and
proteins that is synthesized by type II alveolar pneumocytes.
Surfactant lowers surface tension at the air–liquid interface,
thereby maintaining alveolar expansion at end expiration. Of the
four surfactant associated proteins (surfactant protein (SP)-A,
SP-B, SP-C and SP-D), SP-B and SP-C interact with phospholipid components in a tightly coordinated itinerary of synthesis,
secretion, film formation and recycling.1 Pulmonary SP-C is
a highly hydrophobic peptide produced by type II alveolar cells
through the processing of a high molecular weight precursor
(proSP-C) that enhances surface tension and facilitates the
recycling of pulmonary surfactant in vitro. SFTPC gene is short,
spanning only 3500 base pairs on the short arm of chromosome 8
(8p23.1) near the gene coding for bone morphogenetic protein 1.
SP-C deficiency and mutations in the SFTPC have been associated
with interstitial lung disease (ILD) in children and adults.2–5
Hereditary SP-B deficiency, with over 20 different mutations of
SP-B, is a well established cause of severe respiratory failure in
newborns.6 Mutation in SFTPC with resultant SP-C deficiency that
presents as respiratory failure in the neonatal period is a rare
entity. We report on a neonate who presented with progressive
respiratory failure and was diagnosed to have mutation in SFTPC
gene.
Correspondence: Dr AS Soraisham, Department of Pediatrics, Foothills Medical Centre,
University of Calgary, C-211, 1403, 29th Street, NW, Calgary, Alberta, Canada T2N2T9.
E-mail: amuchou@yahoo.com
Received 4 August 2005; revised 21 September 2005; accepted 22 September 2005
Case report
A full term (39 weeks), male infant weighing 2940 g was born to a
36-year-old healthy gravida 3 para 1 mother by cesarean section
after failed vacuum extraction. Apgar scores were 9 and 9 at 1 and
5 min, respectively.
The infant was well until day 3 of life. At that time, physical
examination revealed tachypnea and chest retractions; hence, the
infant was transferred to the special care nursery. A complete sepsis
work up was done and antibiotics were commenced. The infant was
started on 30% inspired oxygen via nasal prongs. A capillary blood
gas revealed pH ¼ 7.32, PCO2 ¼ 53, PO2 ¼ 45; HCO3 ¼ 27 and
BE ¼ 1. The chest radiograph revealed mildly hyperinflated lungs
and mild perihilar interstitial markings (Figure 1).
Echocardiogram showed an anatomically normal heart with no
structural malformation. On day 7, the infant developed progressive
increase in work of breathing with increasing oxygen requirement;
continuous positive airway pressure was initiated. Chest radiograph
showed increasing haziness of both lung fields with air
bronchograms (Figure 2). On day 10, the infant developed
progressive respiratory acidosis followed by intubation, mechanical
ventilation and transport to a neonatal intensive
care unit (NICU).
In the NICU, examination revealed the following: temperature
37.41C pulse rate 160/min, respiratory rate 90/min and blood
pressure 72/42 mmHg. Systemic examination was unremarkable
except for respiratory distress. There was no clinical evidence of
pulmonary hypertension. He was initially ventilated on pressure
settings of 20/4 cm H2O with a ventilatory rate of 60/min and 80%
inspired oxygen. An arterial blood gas revealed hypoxia and
respiratory acidosis (pH ¼ 7.35; PaCO2 ¼ 60; PaO2 ¼ 41 and
HCO3 ¼ 32 with a/A ratio of 0.13 and oxygenation index (OI)
of 14).
A complete sepsis work up was repeated. The white blood cell
count was unremarkable. Chest radiograph revealed diffuse ground
glass appearance with air bronchogram (Figure 3).
Nasopharyngeal and tracheal aspirates were sent for viral (antigen
testing for Influenza A and B, Para influenza A and B, Respiratory
syncytial virus, Herpes simplex and Adenovirus), chlamydia and
mycoplasma cultures that were subsequently reported as negative.
Neonatal respiratory failure
AS Soraisham et al
68
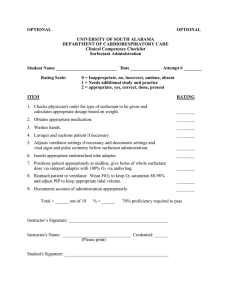
Figure 1 X-ray of chest (on day 3 of age) showing mild lung
hyperinflation and perihilar streaking.
Figure 2 X-ray of chest (on day 7) showing diffuse haziness of both
lung fields and air bronchograms.
He was treated with antibiotics; acyclovir and bovine lipid
extract surfactant. After the surfactant administration, the inspired
oxygen was reduced to 60% with improvement in the blood gas
(pH ¼ 7.39; PaCO2 ¼ 52; PaO2 ¼ 99; HCO3 ¼ 31 and a/A ¼ 0.37
with OI ¼ 5). Tracheal aspirate sample for surfactant protein
analysis was collected 24 h after the first dose of surfactant. Based
on the clinical response to surfactant and radiographic findings, he
was suspected to have surfactant protein deficiency. After informed
and written parental consent, tracheal aspirate and blood for
molecular typing for surfactant protein were sent to DNA Diagnostic
Journal of Perinatology
Figure 3 X-ray of chest (on day 10) showing diffuse pulmonary
atelectasis with air bronchograms and loss of cardiac silhouette.
laboratory (CLIA certified) at Johns Hopkins Hospital (http://
www.hopkinsmedicine.org/dnadiagnostic).
Assisted ventilatory support was continued. He required high
ventilatory pressures and FiO2. He was treated with repeated
doses of surfactant every 24–26 h. Dexamethasone treatment was
intermittently attempted with apparent pulmonary improvement
as assessed by ability to reduce the frequency of surfactant
administration. Computerized tomography (CT) studies of the
chest showed diffuse atelectasis, bronchial inflation and
accentuation of interlobular septa. There were no focal
parenchymal or mass lesions.
On day 25 of life, he developed temperature instability, feeding
intolerance, tachycardia and increasing oxygen requirement.
Laboratory studies showed leukocytosis with a left shift; C-reactive
protein of 28 mg/l (normal: 0–8 mg/l) and bacteremia
with coagulase negative staphylococcus. He was treated with
vancomycin for 7 days. During this episode, he required more
frequent surfactant therapy every 18–24 h. He also developed
hepatosplenomegaly and conjugated hyperbilirubinemia.
Abdominal ultrasonography showed hepatosplenomegaly,
but no structural or focal lesions on abdominal
ultrasonography.
Initial results of the surfactant protein studies showed the
presence of surfactant protein B in the tracheal aspirate. However,
his clinical course, response to surfactant and radiological findings
indicated functional surfactant protein deficiency. Subsequently,
DNA sequencing showed a single base deletion (Nt 392 del T) in
exon 4 of SFTPC gene.
On day of life 44, he developed unremitting hypoxemia that was
unresponsive to surfactant therapy. The ventilator management
was withdrawn with death ensuing thereafter.
Neonatal respiratory failure
AS Soraisham et al
69
Partial autopsy was performed. The lung histology showed
diffuse interstitial thickening with proliferation of mesenchymal
fibroblastic cells and chronic inflammatory infiltrates of
lymphocytes, plasma cells and scattered eosinophils. A
superimposed widespread acute bronchopneumonia affected all
lobes of both lungs. Hyperplasia of type II alveolar cells was
present. No misalignment of pulmonary vessels was evident.
All family members of this infant including the siblings are
healthy without respiratory symptoms.
Discussion
In this report, we describe a term infant with progressive fatal
respiratory failure during the first 2 months of life that was
associated with mutation (Nt 392 del T) in exon 4 of SFTPC gene.
This deletion causes a shift in the open reading frame resulting in
a premature stop codon approximately 54 amino-acids
downstream, and 13 codons upstream of the normal stop codon.
This SFTPC mutation has not been reported previously. In our
patient, this mutation was associated with early onset severe
respiratory insufficiency and on autopsy was appeared as a
nonspecific interstitial pneumonia.
Nogee et al.3 published the first report of an association between
mutation in SFTPC and a disease in a full-term female infant, who
presented with respiratory distress at 6 weeks of age. Hamvas et al.4
reported another infant with progressive and severe ILD associated
with mutation in SFTPC gene. This infant was healthy until 3
months of age and subsequently developed growth failure and ILD
resulting in lung transplantation by 14 months of age. Brasch
et al.7 reported a 13-month-old child with severe respiratory
insufficiency associated with de novo missense mutation of SFTPC.
The mutations in the SFTPC gene have been associated with
familial and sporadic ILD in children and adults.2–5 The clinical
and histological expressions of these mutations have been variable
with children exhibiting chronic pneumonitis of infancy or
nonspecific ILD and adults exhibiting usual interstitial
pneumonitis, desquamative interstitial pneumonitis or idiopathic
pulmonary fibrosis.
The exact mechanisms of lung disease associated with SFTPC
gene mutation are not completely known. The absence of mature
SP-C in the large aggregate surfactant and juxtanuclear
accumulation of pro-SP-C are consistent with a dominant-negative
effect of presumably misfolded peptide that prevents normal proSP-C trafficking into the multivesicular and lamellar bodies.8 It
has been speculated that the aggregation of misfolded pro-SP-C
may interfere with the unfolded protein response and result in toxic
gain of function similar to that seen in mice that overexpress SP-C
or in patients with Alzheimer’s disease, alpha 1 antitrypsin
deficiency and cystic fibrosis.9,10 Surfactant dysfunction may be
another factor that probably contributed to the infant’s
development of respiratory failure. Deficiency of SP-C could
predispose a person to recurrent atelectasis, lung injury and
inflammation.2
Unlike surfactant protein B deficiency, the age at presentation of
surfactant protein C mutation is variable and ranges from the
neonatal period to adulthood.11 The clinical presentation varies
from mild tachypnea, respiratory distress and failure to thrive to
progressive respiratory failure. The course of the infant in this case
report was more severe than previous case reports with SFTPC
mutations. The novel SFTPC gene mutation in this infant very
likely led to a frameshift. Frameshift mutations often result in the
unstable mRNA transcripts. This probably led to early disruption of
SP-C metabolism and surfactant dysfunction with associated
widespread lung injury and inflammation.12
At present, there is no definite treatment for respiratory failure
associated with mutation of SFTPC. Although, lung transplantation
may be an option in progressive respiratory failure,12 there are no
clear guidelines for SFTPC mutation since the time of presentation
and severity of illness are variable. Lung transplantation was
successful in children with SFTPC gene mutation as noted in one
case report.4 Few cases of surfactant protein C deficiency treated
with hydroxychloroquine have been reported.1,13
We report this case to highlight the high index of suspicion for
SFTPC mutation in a neonate presenting with an unusual course
of severe respiratory failure. This infant was found to have a novel
SFTPC gene mutation.
Acknowledgments
We acknowledge Dr Lawrence Nogee, who guided and assisted us with the
surfactant protein analysis.
References
1 Whitsett JA, Weaver TE. Hydrophobic surfactant proteins in lung function
and disease. N Engl J Med 2002; 347: 2141–2148.
2 Amin RS, Wert SE, Baughman RP, Tomashefski Jr JF, Nogee LM, Brody AS
et al. Surfactant protein deficiency in familial interstitial lung disease.
J Pediatr 2001; 139: 85–92.
3 Nogee LM, Dunbar AE, Wert SE, Askin F, Hamvas A, Whitsett JA. A mutation
in the surfactant protein C gene associated with familial interstial lung
disease. N Engl J Med 2001; 344: 573–579.
4 Hamvas A, Nogee LM, White FV, Schuler P, Hackett BP, Huddleston CB et al.
Progressive lung disease and surfactant dysfunction with a deletion in
surfactant protein C gene. Am J Respir Cell Mol Biol 2004; 30: 771–776.
5 Thomas AQ, Lane K, Philips III J, Prince M, Markin C, Speer M et al.
Heterozygosity for a surfactant protein C gene mutation associated with
usual interstitial pneumonitis and cellular non-specific interstitial
pneumonitis in one kindred. Am J Respir Crit Care Med 2002; 165:
1322–1328.
6 Nogee LM, Wert SE, Proffit SA, Hull WM, Whitsett JA. Allelic heterogeneity in
hereditary surfactant protein B (SP-B) deficiency. Am J Respir Crit Care
Med 2000; 161: 973–981.
Journal of Perinatology
Neonatal respiratory failure
AS Soraisham et al
70
7 Brasch F, Griese M, Tredano M, Johnen G, Ochs M, Rieger C et al.
Interstitial lung disease in a baby with a de novo mutation in the SFTPC
gene. Eur Respir J 2004; 24: 30–39.
8 Kabore AF, Wang WJ, Russo SJ, Beers MF. Biosynthesis of surfactant protein
C: characterization of aggresome formation by EGFP chimeras containing
propeptide mutants lacking conserved cysteine residues. J Cell Sci 2001; 114:
293–302.
9 Conkright JJ, Na CL, Weaver TE. Over expression of surfactant protein-C
mature peptide causes neonatal lethality in transgenic mice. Am J Respir
Cell Mol Biol 2002; 26: 85–90.
Journal of Perinatology
10
11
12
13
Perlmutter DH. The cellular response to aggregated proteins associated with
human disease. J Clin Invest 2002; 110: 1219–1220.
Cameron HS, Somaschini M, Carrera P, Hamvas A, Whitsett JA, Wert SE et al.
A common mutation in the surfactant protein C gene associated with lung
disease. J Pediatr 2005; 146: 370–375.
Moreno A, Maestre J, Balcells J, Marhuenda C, Cobos N, Roman A et al. Lung
transplantation in young infants with interstitial pneumonia. Transplant
Proc 2003; 35: 1951–1953.
Rosen DM, Waltz DA. Hydroxychloroquine and surfactant protein C
deficiency. N Engl J Med 2005; 352: 207–208.