Animal Reproduction Science 82–83 (2004) 267–280
Major histocompatibility antigen expression on the
bovine placenta: its relationship to abnormal
pregnancies and retained placenta
C.J. Davies a,∗ , J.R. Hill b , J.L. Edwards c , F.N. Schrick c ,
P.J. Fisher d , J.A. Eldridge a , D.H. Schlafer d
a
Department of Veterinary Microbiology and Pathology & Center for Reproductive Biology, College of
Veterinary Medicine, Washington State University, P.O. Box 647040, Pullman, WA 99164-7040, USA
b CSIRO Livestock Industries, Armidale, NSW 2350, Australia
c Department of Animal Science, Institute of Agriculture, Tennessee Agricultural Experiment Station,
The University of Tennessee, Knoxville, TN 37996, USA
d Department of Biomedical Sciences, College of Veterinary Medicine, Cornell University,
Ithaca, NY 14853, USA
Abstract
In viviparous animals, regulation of expression of major histocompatibility complex (MHC) class
I antigens by the trophoblast cells, which constitute the outermost layer of the placenta, seems to
be critical for maternal immunological acceptance of an allogeneic fetus. Cattle are unusual in this
regard, since the bovine trophoblast cells, in specific regions of the uterine/placental interface, normally express MHC class I antigens during the third trimester of gestation. This expression appears
to be biologically relevant as MHC class I compatibility between a cow and her fetus has been
associated with an increased incidence of placental retention. We have found significant differences
in lymphocyte populations, cytokine production, and trophoblast cell apoptosis in the placentomes
of MHC-compatible and -incompatible pregnancies at parturition. This suggests that maternal immunological recognition of fetal MHC class I proteins triggers an immune/inflammatory response
that contributes to placental separation at parturition in cattle. Early in pregnancy, a complete shutdown of MHC class I expression by trophoblast cells appears to be critical for normal placental
development and fetal survival. In bovine somatic cell nuclear transfer (SCNT) pregnancies, there
is an extremely high rate of fetal loss between days 30 and 90 of pregnancy. We have shown that
in bovine SCNT pregnancies, between days 34 and 63 of gestation, there is both abnormal expression of MHC class I antigens by trophoblast cells and an abnormal accumulation of lymphocytes
within the uterine stroma. Consequently, it is likely that activation of the maternal mucosal immune
system, within the uterus at the same time when placentomes are being established, interferes with
∗ Corresponding author. Tel.: +1 509 335 7106; fax: +1 509 335 8529.
E-mail address: cdavies@vetmed.wsu.edu (C.J. Davies).
0378-4320/$ – see front matter © 2004 Elsevier B.V. All rights reserved.
doi:10.1016/j.anireprosci.2004.05.016
268
C.J. Davies et al. / Animal Reproduction Science 82–83 (2004) 267–280
the process of placentome development and leads to immune-mediated abortion. Our data suggest
that bovine MHC-compatible pregnancies provide a unique model for studying regulation of the
uterine immune system, as well as immune-mediated placental rejection.
© 2004 Elsevier B.V. All rights reserved.
Keywords: Bovine placenta; Major histocompatibility complex; Reproductive immunology; Retained placenta;
Immune-mediated abortion
1. Introduction
In viviparous animals, an allogeneic fetus must develop within its mother’s uterus. Consequently, maternal immunological acceptance of the fetus is vital for reproductive success.
In most mammals, tolerance of the fetal allograft appears to involve both a lack of expression
of polymorphic major histocompatibility complex (MHC) antigens on the trophoblast cells
that cover the exterior of the placenta as well as the maintenance of an immunologically
quiescent or immunosuppressive state of the uterus.
The MHC region got its name because alloantigens encoded by this genetic region
are extremely potent at stimulating rejection of transplanted tissues or organs. It is now
known that the MHC encodes two types of extremely polymorphic cell surface glycoproteins, the class I and class II proteins, that present peptide antigens to T lymphocytes. The
‘classical’, MHC class I molecules are expressed on most somatic cells and present peptides
derived from an animal’s own proteins, or from proteins of intracellular pathogens, to cytotoxic/suppressor T lymphocytes (CTL). In most species that have been studied, trophoblast
cells do not express ‘classical’, class I molecules (Hunt et al., 1987; Gogolin-Ewens et al.,
1989; Loke, 1989; Donaldson et al., 1990; Low et al., 1990; Kydd et al., 1991). Consequently, lack of MHC class I expression is believed to protect the placenta from attack
by the maternal immune system. This hypothesis is substantiated by experiments demonstrating that allografts expressing classical, class I antigens do not survive in the uterus
(Beer and Billingham, 1974; Reimers and Dziuk, 1974; Hansen et al., 1986). Pregnancy
or pseudopregnancy in rats, or progesterone treatment in sheep, prolonged allograft survival but did not protect allografts from eventual rejection (Beer and Billingham, 1974;
Hansen et al., 1986). Additional class I genes encode ‘non-classical’, class I molecules.
The ‘non-classical’, class I genes are much less polymorphic and have restricted cellular
expression. Furthermore, the products of these genes appear to have distinct functions.
An example of a ‘non-classical’, class I gene is HLA-G, encoded in the human leukocyte
antigen (HLA) complex. In humans, HLA-G is expressed specifically on invasive, cytotrophoblast cells and may protect these cells from attack by CD4+ T lymphocytes and/or
natural killer (NK) cells (Ellis et al., 1986, 1990; Kovats et al., 1990; Le Bouteiller, 2000;
Bainbridge et al., 2000, 2001a; Park et al., 2004a). MHC class II molecules are usually expressed only on professional antigen-presenting cells (APC): dendritic cells, macrophages,
and B lymphocytes. This pattern of expression is consistent with their function, which
is to present peptides from extracellular pathogens or proteins to helper T lymphocytes.
Under normal circumstances, MHC class II antigens are not expressed on trophoblast
cells.
C.J. Davies et al. / Animal Reproduction Science 82–83 (2004) 267–280
269
2. Trophoblast cell MHC class I expression in normal bovine pregnancies
Numerous studies have failed to detect the expression of the highly polymorphic, ‘classical’
MHC class I antigens by trophoblast cells of various species (Hunt et al., 1987; GogolinEwens et al., 1989; Loke, 1989; Donaldson et al., 1990; Kydd et al., 1991). However, in
some species, it was found that subpopulations of trophoblast cells expressed monomorphic, ‘non-classical’ MHC class I proteins. An example of this is the expression of HLA-G
by human, invasive cytotrophoblast cells (Ellis et al., 1986, 1990; Kovats et al., 1990). Low
et al. (1990) reported finding areas of MHC class I expression in the interplacentomal region of three of six bovine placentas, examined by immunohistochemistry. In a subsequent
study, we used immunohistochemistry to quantitate MHC class I expression in three regions
of the uterine/placental interface: the interplacentomal region, the arcade region where the
placenta covers the luminal surface of the placentomes, and the villous/crypt region within
the placentomes (Davies et al., 2000). During the fourth month of pregnancy, on an average,
only 2% of interplacentomal trophoblast cells expressed class I antigens. However, during
the sixth and eighth months of pregnancy, and at parturition, 26–100% of interplacentomal
trophoblast cells expressed class I antigens. As pregnancy progressed, class I expression
was also upregulated in the arcade region of the placentomes, reaching maximum expression just prior to parturition, when on average, 62% of arcade trophoblast cells expressed
class I antigens. We never detected the presence of class I antigens on trophoblast cells
of the cotyledonary villi by immunohistochemistry. However, another group has reported
detecting both MHC class I mRNA and protein in cotyledonary, binucleate trophoblast cells
isolated from placentomes collected on day 275 of pregnancy, which is 4–15 days prior to
normal parturition (Ellis et al., 1998; Bainbridge et al., 2001b). The difference between our
results and those of other investigators (Ellis et al., 1998; Bainbridge et al., 2001b) probably
reflects the difference in the time relative to parturition when examination was carried out,
or the fact that these investigators did not distinguish between class I antigen expression by
villous and arcade binucleate trophoblast cells.
Placentomes are the areas of interface, providing tight attachments between maternal and
fetal membranes, for nutrient exchange. They are formed by branching fetal cotyledonary
villi, which grow down into the maternal caruncular crypts in a finger-in-glove arrangement
(Schlafer et al., 2000). A novel finding, in our study, on uterine and placental class I antigen
expression in cattle was that the endometrial epithelial cells of the maternal crypts lacked
detectible class I expression, throughout pregnancy (Davies et al., 2000). We know of no
other species in which class I antigen expression by endometrial epithelial cells is shut down.
Bovine binucleate trophoblast cells produce a number of important steroids and proteins
including progesterone, placental lactogen, and the pregnancy-associated glycoproteins
(Reimers et al., 1985; Duello et al., 1986; Myers and Reimers, 1988; Roberts et al., 1995).
The binucleate cells are unique in that they migrate across the interface and fuse with
endometrial epithelial cells forming hybrid trinucleate cells (Wooding and Wathes, 1980;
Wooding, 1982, 1992). If these trinucleate cells were to express maternal MHC class I
antigens, they would almost certainly present fetal peptides. Presentation of fetal peptides
by maternal class I glycoproteins could provoke attack by maternal cytotoxic T lymphocytes.
Consequently, lack of MHC class I expression by cryptal, endometrial epithelial cells may
be an important mechanism for protecting the fetus from immune-mediated rejection.
270
C.J. Davies et al. / Animal Reproduction Science 82–83 (2004) 267–280
Bainbridge et al. (2001b) reported that class I mRNA isolated from bovine binucleate cells
corresponded to both, classical and non-classical class I proteins. Recently, we profiled the
mRNA expression at term in intercotyledonary trophoblast cells, and in fetal and maternal
lymphocytes. We found that the trophoblast cells expressed both, classical and non-classical,
class I genes and that the percentage of transcripts corresponding to non-classical genes was
much higher in trophoblast cells than in lymphocytes (Davies, unpublished). In addition,
different non-classical, class I mRNA were isolated from trophoblast cells with distinct
MHC genotypes. It is, therefore, likely that the classical class I proteins, and possibly
some of the non-classical proteins, expressed by bovine trophoblast cells are capable of
stimulating a maternal, anti-placental immune response.
3. MHC class I compatibility and placental retention
Tight attachment of the placenta to the maternal endometrium must be maintained
throughout pregnancy. On the other hand, placental attachments must be rapidly broken
down at parturition. The importance of placental separation at term in cattle is underscored
by the clinical problem of placental retention. The overall rate of placental retention in cattle
is approximately 6.6% (Joosten et al., 1987). Established risk factors for placental retention
include abortion, stillbirth, twin births, dystocia, induction of parturition, metabolic disorders, or short gestation length (Larson et al., 1985; Joosten et al., 1987). Nevertheless, only
about a third of retained placentas are associated with these risk factors. Even in normal
pregnancy and delivery, there is a 4.1% incidence of placental retention (Joosten et al., 1987,
1991b). Recent data suggest that in these cases placental retention may be due to failure of
immune-mediated rejection of the placenta at parturition.
Gunnink (1984a–d) was the first to suggest that an inflammatory response was involved
in normal placental separation. In a series of elegant experiments, this investigator demonstrated that bovine placentomes from cows with normal placental separation contained a
chemotactic factor for leukocytes and that this factor was lacking in placentomes from cows
with retained placentas. In addition, he demonstrated that blood leukocytes from cows with
retained placentas responded poorly to chemotactic stimuli, presumably because they were
not activated. A recent study also found that blood neutrophils from cows with retained
placenta were in a less activated state than those from cows with normal placental separation (Kimura et al., 2002). Furthermore, this study provided evidence indicating that
one of the chemotactic factors in placentomes at parturition is IL-8. Another recent study
found that placentomal macrophages from cows that released their placentas normally contained immunoreactive acid phosphatase, but that cows with retained placentas had much
lower levels of this lysosomal enzyme (Miyoshi et al., 2002). In a particularly intriguing
study, Joosten and coworkers (Joosten et al., 1991a; Joosten and Hensen, 1992) found that
placental retention following normal parturition was associated with MHC class I compatibility, or identity, between a dam and her calf. One explanation for this finding is that the
presence of classical, class I antigens on trophoblast cells stimulates a beneficial trophic,
and/or anti-inflammatory, immune response that is required for normal placental maturation
(Wegmann, 1987; Joosten and Hensen, 1992). Alternatively, immunological recognition of
trophoblast, class I proteins at parturition could initiate a destructive, but necessary, im-
C.J. Davies et al. / Animal Reproduction Science 82–83 (2004) 267–280
271
mune response that results in the breakdown of placentomal attachments and placental
release.
Another interesting observation, although not necessarily linked to immune function, is
that in pregnancies with normal placental separation, virtually all placentomal binucleate
cells degranulate prior to parturition; however, in cattle with retained placentas binucleate
cell degranulation is incomplete (Williams et al., 1987; Gross et al., 1991). We have used
immunohistochemistry with the SBU-3 monoclonal antibody (mAb) to study the process
of binucleate cell degranulation (Lee et al., 1985, 1986a, b, 1990; Morgan et al., 1989;
Schlafer et al., 2000). This antibody reacts with one of the pregnancy-associated glycoproteins (Atkinson et al., 1993; Xie et al., 1997). In prepartum samples, collected following
the drop in progesterone that occurs less than 24 h before parturition, we found that virtually all SBU-3-positive binucleate cells had fused with endometrial epithelial cells and
degranulated (Schlafer et al., 2000).
Based on these findings, we proposed the hypothesis that an immune/inflammatory process triggered by periparturient expression of foreign class I molecules on placentomal
trophoblast cells is required for normal placental separation. To test this hypothesis, we conducted a breeding study with the objective of comparing cellular and molecular events at parturition in MHC-compatible and -incompatible pregnancies. Prepartum samples, consisting
of intact placentomes, and full-thickness, apposed, interplacentomal uterine and placental
tissues, were collected from two groups of five heifers, one carrying MHC-incompatible and
the other MHC-compatible pregnancies. The samples were collected during cesarean sections, performed under local anesthesia, within 24 h of normal parturition as determined by
a drop in progesterone to <2 ng/ml (Matsas et al., 1992). In addition, postpartum samples,
consisting of intact placentomes with caruncular and cotyledonary tissues, were collected
per vagina, within half an hour of parturition, from five heifers carrying MHC-incompatible
and four heifers carrying MHC-compatible pregnancies. Immunohistochemistry was used to
assess the level of trophoblast and endometrial epithelial cell class I expression, the number
of binucleate trophoblast cells, the leukocyte populations in the uterus and placenta, and the
amount of immunoreactive IL-2 and TNF-␣. Apoptosis was assessed both by end-labeling
of fragmented DNA with Klenow (FragEL DNA Fragmentation Detection Kit; Calbiochem)
and by quantitation of cells with apoptotic bodies in Hoechst 33342-stained sections.
The extent of class I expression by interplacentomal and placentomal arcade trophoblast
cells were not significantly different in compatible and incompatible pregnancies. However,
compatible pregnancies had significantly greater numbers of SBU-3-positive binucleate
cells at term than incompatible pregnancies, both in placentomal villi (Wilcoxon rank sum
test P = 0.037) and in arcades (P = 0.005). In our previous studies, we had detected a greater
than 10-fold increase in the number of CD68+ (mAb EMB11; DACO Corp., Carpinteria,
CA) fetal macrophages in the cotyledonary villi between the sixth and the eighth month of
pregnancy (Bielefeldt-Ohmann et al., 1988; Ackermann et al., 1994; Schlafer et al., 2000).
Fetal macrophage counts in the MHC-compatible and -incompatible pregnancies were not
significantly different. However, with the exception of one case, in the maternal, caruncular
crypts of cesarean section samples from the incompatible pregnancy group (n = 4), there
were significantly more macrophages than in the caruncular crypts of the compatible pregnancies (n = 5; Wilcoxon rank sum test, P = 0.028 for manual counts and P = 0.014 for
counts done by digital image processing).
272
C.J. Davies et al. / Animal Reproduction Science 82–83 (2004) 267–280
We assessed both maternal and fetal lymphocyte populations in the interplacentomal,
placentomal arcade, and placentomal villous/crypt regions of the interface. In addition to
the MHC-compatible and -incompatible term pregnancies described above, nine pregnancies at earlier stages of gestation, including three each in the fourth, sixth, and eighth
month, were also examined. Cryostat sections that included both fetal and maternal tissues were stained using mAb specific for CD2 (CC42, BioSource International, Camarillo, CA), CD3 (MM1A, VMRD, Pullman, WA), CD4 (CC30, BioSource), CD8 (CC63,
BioSource), and ␥/␦-TCR (GB21A, VMRD). Although lymphocyte populations in all regions of the uterus changed over the course of pregnancy, significant differences between
MHC-compatible and -incompatible pregnancies were restricted to the maternal arcade
region. In MHC-incompatible pregnancies, there were significantly fewer arcade cytotoxic/suppressor T lymphocytes at parturition than during gestation (Wilcoxon rank sum
test, P = 0.001 for CD2 and P = 0.023 for CD8). This decrease in the number of arcade
CTL did not occur in MHC-compatible pregnancies. Consequently, the numbers of CTL
were significantly different in compatible and incompatible pregnancies (Wilcoxon rank
sum test, P = 0.008 for CD2 and P = 0.014 for CD8). Presumably, the decline in the arcade CTL population in MHC-incompatible pregnancies was a consequence of recognition
of foreign, paternally encoded class I antigens. However, the mechanism underlying this
decline is not known. In both mice and horses, pregnancy-associated induction of transient
CTL tolerance to paternal MHC antigens has been described (Tafuri et al., 1995; Jiang and
Vacchio, 1998; Zhou and Mellor, 1998; Baker et al., 1999). Furthermore, there is evidence for a Fas-mediated clonal deletion of trophoblast-specific CTL in mice (Jiang and
Vacchio, 1998). It is therefore possible that uterine inflammation at parturition is initiated
by indirect, helper T-lymphocyte recognition of processed MHC class I peptides, presented
by MHC class II molecules on maternal antigen-presenting cells in the caruncular crypts,
rather than direct recognition of MHC class I antigens by reactivated CTL in the placentomal
arcades.
The most exciting findings involved cytokine production and apoptosis. In comparison
to incompatible pregnancies, compatible pregnancies had dramatically reduced amounts
of immunoreactive IL-2 in endometrial epithelial and trophoblast cells at term (mAb IL-2
14.1, VMRD). In addition, maternal and fetal macrophages in MHC-compatible pregnancies at term stained more intensely with antibodies against TNF-␣ than macrophages in
incompatible pregnancies (mAb 2C4-1D3 and rabbit anti-rBoTNF-␣, both gifts from Dr.
Ted Elsasser). This may reflect release of immunoreactive TNF-␣ in MHC-incompatible
pregnancies. We also found fragmented DNA, indicative of apoptosis, in virtually all endometrial epithelial and trophoblast cells in prepartum, cesarean section samples from
MHC-incompatible but not compatible pregnancies (Klenow FragEL DNA Fragmentation
Detection Kit; Calbiochem, Cambridge, MA). To confirm that these cells were undergoing
apoptosis, we counted apoptotic bodies in sections stained with the DNA stain Hoechst
33342 (Molecular Probes, Eugene, OR). Apoptotic bodies are generally detected during
the later stages of apoptosis. Consequently, the proportion of villous trophoblast cells with
apoptotic bodies was significantly greater in samples collected postpartum than those collected at cesarean section or during gestation (Kruskal–Wallis test, P < 0.001). However,
MHC-compatible and -incompatible pregnancies were not significantly different in the parameters compared.
C.J. Davies et al. / Animal Reproduction Science 82–83 (2004) 267–280
273
It is clear that there are significant differences in the events that occur at parturition in
MHC class I-compatible and -incompatible pregnancies. Presumably, these differences are
due to immunological recognition of class I proteins. However, recognition may involve
indirect recognition by helper T lymphocytes rather than direct recognition by CTL. Activation of T helper type 1 (Th1) cells and macrophages, with release of IFN-␥, TNF-␣, and other
inflammatory mediators, may induce apoptosis of trophoblast cells and endometrial epithelial cells resulting in placental release. There are probably also redundant mechanisms that
contribute to placental release. Some of the differences observed between MHC-compatible
and -incompatible pregnancies may be due to a delay in molecular and cellular events in
compatible pregnancies rather than their complete absence. Nevertheless, MHC compatibility has significant molecular consequences and can result in an increased incidence of
retained placentas (Joosten et al., 1991a; Joosten and Hensen, 1992).
4. MHC class I expression and immune-mediated abortion
Bovine pregnancies established by somatic cell nuclear transfer (SCNT), often referred
to as cloning, fail at a much higher frequency than those established by in vivo or in vitro
fertilization (IVF) (reviewed by Edwards et al., 2003). Much of the pregnancy failure in
SCNT pregnancies is associated with abnormal placental development (Stice et al., 1996;
Hill et al., 2000). Recently, Hill et al. (2002) reported that trophoblast cells from 34- to
63-day-old SCNT pregnancies expressed MHC class I antigens. In contrast, trophoblast
cells from age-matched control pregnancies were completely negative for class I expression. Another striking feature of days 34–63 SCNT pregnancies was the presence of large
lymphoid aggregates, and an increased number of scattered CD3+ lymphocytes, in the
uterine stroma of the SCNT embryo transfer (ET) recipients (Hill et al., 2002).
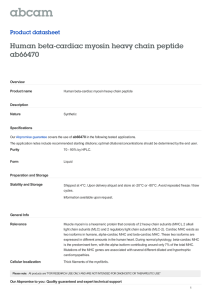
Immunohistochemical characterization of uterine lymphocytes in SCNT pregnancies revealed that the majority of lymphocytes in lymphoid aggregates were CD4+ helper T lymphocytes (Fig. 1). The aggregates also contained CD8+ T lymphocytes, B lymphocytes, and
a small number of ␥/␦-TCR-positive T cells (Figs. 1 and 2). The large number of CD4+ T
lymphocytes in lymphoid aggregates suggests that in SCNT pregnancies the primary mode
of immunological response to trophoblast class I antigens may involve indirect recognition.
Indirect recognition is a well-established mechanism of graft rejection (Benichou et al.,
1998; Game and Lechler, 2002). In cattle, binucleate trophoblast cells migrate across the
interface and fuse with endometrial epithelial cells leading to the formation of hybrid giant
or trinucleate cells (Wathes and Wooding, 1980; Wooding and Wathes, 1980). The hybrid
cells are short lived, and dead cells with pyknotic nuclei have been observed within the
endometrium and inside the mononuclear trophoblast cells (Wathes and Wooding, 1980;
Wooding and Wathes, 1980). It is likely that uterine macrophages, and/or dendritic cells,
also phagocytize debris from dead giant and trinucleate cells and that these cells process and
present trophoblast antigens. We do not currently have any data regarding the specificity of
the endometrial lymphocytes present in SCNT pregnancies. Demonstration that these cells
are specific for fetal MHC class I antigens is an important objective that we would like
to pursue in the near future. However, demonstration of indirect recognition of fetal MHC
class I proteins by CD4+ helper T lymphocytes would require that the appropriate class I
274
C.J. Davies et al. / Animal Reproduction Science 82–83 (2004) 267–280
Fig. 1. Photomicrographs of uterine lymphoid nodules from SCNT pregnancies stained by immunohistochemistry
with mAb for lymphocyte subset markers: (A) CD2, mAb CC42; (B) CD4, mAb CC30; (C) CD8, mAb CC63;
and (D) ␥/␦ TCR, mAb GB21A (CC42, CC30, and CC63 – BioSource International, Camarillo, CA; GB21A
– VMRD, Pullman, WA). Antigen-positive cells were visualized using an avidin–biotin amplification kit and
the red chromogen 3-amino 9-ethyl carbazole (AEC; Zymed Laboratories, San Francisco, CA); sections were
counterstained with hematoxylin. The majority of lymphocytes in the lymphoid nodules were CD4+ helper T
lymphocytes. In addition, the nodules contained a moderate number of CD8+ cytotoxic/suppressor T lymphocytes
and a few ␥/␦-T cells. Bars represent 100 m.
proteins be cloned and expressed in vitro, so that purified class I proteins could be used in
lymphocyte proliferation or activation assays.
Bovine placentome development begins around day 30 of pregnancy (Schlafer et al.,
2000). We have shown that by day 34 of pregnancy SCNT trophoblast cells express class
I antigens (Hill et al., 2002). Furthermore, in a recent study that employed microarrays to
compare gene expression in individual day 7 blastocysts produced by SCNT and in vitro
fertilization, Pfister-Genskow et al. (submitted for publication) found that MHC class I genes
were upregulated in SCNT blastocysts, derived from a somatic tissue cell line created from
a 58-day-old bovine fetus. The authors used immunofluorescence to confirm that SCNT
blastocysts expressed MHC class I antigens, while IVF blastocysts did not. Expression of
class I antigens by SCNT blastocysts suggests that class I expression on the placenta results
from incomplete reprogramming of somatic cell nuclei by egg cytoplasm. Abnormal class I
expression early in pregnancy may result in presentation of fetal class I peptides by uterine
antigen-presenting cells just when mature placentation should be developing. Presentation
of foreign, fetal class I peptides by MHC class II molecules of maternal, uterine APC
would likely induce a massive CD4+ T-lymphocyte response similar to the response seen in
SCNT pregnancies (Fig. 1). The response in SCNT pregnancies is probably an inflammatory
C.J. Davies et al. / Animal Reproduction Science 82–83 (2004) 267–280
275
Fig. 2. Photomicrograph of a uterine lymphoid nodule and surrounding uterine stroma stained by immunohistochemistry with mAb BLA-36 (Dako, Carpinteria, CA). BLA-36 is specific for an antigen on B lymphocytes
and plasma cells (Kelley et al., 1997). Positive mAb staining is red (AEC); the section was counterstained with
hematoxylin. The uterine lymphoid nodules found in SCNT pregnancies contained a moderate number of B lymphocytes. However, the majority of the B lymphocytes and plasma cells were located in the uterine stroma around
the nodules. Bar represents 100 m.
T-cell response with the production of mediators such as IFN-␥. To determine if this is the
case, we are using real-time RT-PCR to evaluate uterine and placental cytokine mRNA
transcription in SCNT and control pregnancies. In theory, inflammatory mediators could
upset the normal hormone/cytokine balance, modulate cell surface protein expression, and
interfere with placentome development.
If SCNT pregnancies fail as a result of trophoblast cell class I expression, which induces a maternal anti-placental immune response that interferes with placental development, MHC class I compatible SCNT pregnancies, in which the fetus carries only class I
antigens also carried by the ET recipient, should have much better fetal survival rates than
MHC-incompatible SCNT pregnancies. It is likely that the greatest improvement would be
between days 30 and 90 when placentation is occurring. Although we have not had the opportunity to do a controlled experiment to test the hypothesis that MHC class I compatible
SCNT pregnancies have significantly improved fetal survival rates, we have examined the
level of MHC class I compatibility in successful and unsuccessful SCNT pregnancies. In
SCNT pregnancies produced at the University of Tennessee in 2001 and 2002, we observed
a substantial difference in the number of successful pregnancies with different SCNT donor
cell lines. Consequently, we used a microarray-based MHC typing system, and genomic
MHC class I sequencing, to characterize the MHC haplotypes carried by the donor cell lines
and most of the ET recipients (Park et al., 2004b). The objective was to see if there was
a difference in MHC compatibility in successful and unsuccessful pregnancies. Because
the SCNT donor cell lines were derived from Jersey cows and the ET recipients were either Angus or Angus crosses, none of the pregnancies were completely MHC-compatible.
Nevertheless, the data strongly support the hypothesis that MHC compatibility results in
improved fetal survival. The two SCNT donor cell lines with substantial numbers of successful pregnancies were both derived from MHC homozygous cows. In contrast, the SCNT
276
C.J. Davies et al. / Animal Reproduction Science 82–83 (2004) 267–280
Table 1
Comparison of abortion rates with MHC homozygous and heterozygous SCNT cell lines
SCNT cell line
Year
MHC typea
Number of
embryos
transferred
Number of pregnant ET recipients
Day 28b
Day 90c
Day 200c
Termc
48
21
39
29
6
10
21
5
8
21
5
6
13
4
6
108
45
34
32
23
MHC class I heterozygous SCNT cell lines
UT4381
2001
AH12/AH68
UT4472
2002
AH12/AH68
48
5
18
3
0
1
0
1
0
1
Total
53
21
1
1
1
MHC class I homozygous SCNT cell lines
UT3888
2001
AH68/AH68
UT3888
2002
AH68/AH68
UT4585
2002
AH67/AH67
Total
–
–
–
–
a
MHC class I haplotypes (AH) carried by the SCNT donor cell lines were determined by MHC class I
microarray typing and genomic MHC class I sequencing.
b Day 28 pregnancy rates following transfer of a single SCNT embryo to each ET recipient were not significantly
different for the two groups (P = 0.80).
c Abortion rates for class I homozygous and heterozygous SCNT cell lines were compared for three time
periods: from days 28 to 90, days 28 to 200, and day 28 to term. For all three time periods, abortion rates were
significantly different at P < 0.001 (chi-square test).
donor cell lines with poor fetal survival were from MHC heterozygous cows (Table 1). Furthermore, many of the ET recipients carried MHC haplotypes that were closely related to
the haplotypes of the two MHC homozygous cell lines. Day 28 pregnancy rates following
transfer of a single SCNT blastocyst to each ET recipient were similar, with 42% for MHC
homozygous donor cell lines and 40% for MHC heterozygous donor cell lines (P = 0.80).
However, the abortion rates from days 28 to 90, days 28 to 200, and day 28 to term were
significantly different with the chi-square test giving a probability of P < 0.001 for the null
hypothesis (Table 1). Furthermore, analysis of the microarray class I typing data revealed
that the homozygous SCNT cell lines expressed only a few class I peptides that were not
expressed by the ET recipients that carried SCNT fetuses beyond day 90 of pregnancy. Consequently, it seems unlikely that the strong association between MHC homozygous SCNT
fetuses and improved fetal survival is simply a coincidence.
Results from two lines of investigation in this area may seem to contradict our hypothesis that a substantial portion of the fetal mortality in bovine SCNT pregnancies is due
to inappropriate expression of MHC class I antigens by placental trophoblast cells and
immune-mediated abortion. Studies conducted with MHC class I transgenic mice have
demonstrated that in allogeneic pregnancies, trophoblast class I expression during the second half of pregnancy does not result in increased fetal mortality (Tafuri et al., 1995; Rogers
et al., 1998; Shomer et al., 1998; Zhou and Mellor, 1998; Ait-Azzouzene et al., 2001). In
mice, instead of increased fetal mortality, trophoblast class I expression during the second
half of pregnancy induced both cytotoxic T-cell and B-cell, class I allotype-specific tolerance (Tafuri et al., 1995; Zhou and Mellor, 1998; Ait-Azzouzene et al., 2001). Cattle also
routinely tolerate MHC class I expression on trophoblast cells during the third trimester of
C.J. Davies et al. / Animal Reproduction Science 82–83 (2004) 267–280
277
pregnancy (see Section 2 above; Davies et al., 2000). The transgenic mice discussed thus far
expressed class I proteins on trophoblast cells during the second half of pregnancy. Transgenic mice, with a class I transgene under the control of a housekeeping gene promoter,
expressed MHC class I proteins early in pregnancy and were unable to survive beyond
midgestation (Ait-Azzouzene et al., 1998). In these transgenic mice, fetal death was not
due to immunological rejection, since it occurred in syngeneic as well as allogeneic pregnancies. Although this study demonstrates that in mice MHC class I expression early in
embryogenesis can have profound negative effects, it does not provide direct support for our
hypothesis. Nonetheless, in both mice and cattle abnormal class I expression early in pregnancy seems to be detrimental, while class I expression later in pregnancy is tolerated. Other
studies that need to be considered are those showing that in sheep and rodents allogeneic
skin grafts transplanted into the uterus are rejected; however, progesterone administration
delays the rejection (Beer and Billingham, 1974; Reimers and Dziuk, 1974; Hansen et al.,
1986; Hansen, 1998). In sheep, progesterone has both direct and indirect immunosuppressive effects (Hansen, 1998). During early pregnancy, progesterone stimulates the production
of uterine milk protein, which inhibits lymphocyte function. However, the concentration of
progesterone within the ovine uterus is probably not high enough to have a direct immunosuppressive effect until after day 50 of pregnancy, when placental progesterone production
is sufficient to maintain pregnancy (Hansen, 1998). In cattle, the placenta never produces
enough progesterone to maintain pregnancy. Therefore, it is doubtful that the concentration
of progesterone in the bovine uterus is ever sufficient to directly inhibit lymphocyte activation. We do not believe that the immunosuppressive effects of uterine milk protein would
be sufficient to suppress immunological rejection of SCNT fetuses during the first trimester
of bovine pregnancy.
5. Conclusions
Histocompatibility complex class I expression in bovine trophoblast cells is tightly regulated and biologically relevant. Our findings suggest that in cattle, maternal immunological
recognition of fetal MHC class I proteins expressed by trophoblast cells triggers an immune/inflammatory response that contributes to placental separation at parturition. This
is an intriguing example of adaptation of the immune system for a function distinct from
protection against pathogens. It also appears that aberrant MHC class I expression by trophoblast cells of SCNT fetuses early in pregnancy induces immune-mediated abortion. In
conclusion, we believe that bovine MHC-compatible pregnancies provide a unique model
for studying regulation of the immune system at the uterine/placental interface, as well as
both normal and abnormal, immune-mediated placental rejection.
Acknowledgements
Funds for this work were provided by: USDA NRICGP grant 96-35203-3356; a grant
from Cyagra Inc., Elizabethtown, PA; USDA CSREES Animal Health Formula Funds
provided by the Animal Health Research Center, Washington State University; and funds
278
C.J. Davies et al. / Animal Reproduction Science 82–83 (2004) 267–280
from the Robert Fast Food Animal Research Endowment of the College of Veterinary
Medicine, Washington State University. Funds for the data generated at The University of
Tennessee using somatic cell nuclear transfer were provided by USDA Hatch funds and
the State of Tennessee through the Tennessee Agricultural Experiment Station Department
of Animal Science, The University of Tennessee Food Safety Center of Excellence, and
USDA NRICGP grant 99-35208-8402.
References
Ackermann, M.R., DeBey, B.M., Stabel, T.J., Gold, J.H., Register, K.B., Meehan, J.T., 1994. Distribution of
anti-CD68 (EBM11) immunoreactivity in formalin-fixed, paraffin-embedded bovine tissues. Vet. Pathol. 31,
340–348.
Ait-Azzouzene, D., Langkopf, A., Cohen, J., Bleux, C., Gendron, M.C., Kanellopoulos-Langevin, C., 1998.
Selective loss of mouse embryos due to the expression of transgenic major histocompatibility class I molecules
early in embryogenesis. Mol. Reprod. Dev. 50, 35–44.
Ait-Azzouzene, D., Caucheteux, S., Tchang, F., Wantyghem, J., Moutier, R., Langkopf, A., Gendron, M.C.,
Kanellopoulos-Langevin, C., 2001. Transgenic major histocompatibility complex class I antigen expressed in
mouse trophoblast affects maternal immature B cells. Biol. Reprod. 65, 337–344.
Atkinson, Y.H., Gogolin-Ewens, K.J., Hounsell, E.F., Davies, M.J., Brandon, M.R., Seamark, R.F., 1993.
Characterization of placentation-specific binucleate cell glycoproteins possessing a novel carbohydrate.
Evidence for a new family of pregnancy-associated molecules. J. Biol. Chem. 268, 26679–26685.
Bainbridge, D.R., Ellis, S.A., Sargent, I.L., 2000. HLA-G suppresses proliferation of CD4(+) T-lymphocytes. J.
Reprod. Immunol. 48, 17–26.
Bainbridge, D., Ellis, S., Le Bouteiller, P., Sargent, I., 2001a. HLA-G remains a mystery. Trends Immunol. 22,
548–552.
Bainbridge, D.R., Sargent, I.L., Ellis, S.A., 2001b. Increased expression of major histocompatibility complex
(MHC) class I transplantation antigens in bovine trophoblast cells before fusion with maternal cells.
Reproduction 122, 907–913.
Baker, J.M., Bamford, A.I., Antczak, D.F., 1999. Modulation of allospecific CTL responses during pregnancy in
equids: an immunological barrier to interspecies matings? J. Immunol. 162, 4496–4501.
Beer, A.E., Billingham, R.E., 1974. Host responses to inta-uterine tissue, cellular and fetal allografts. J. Reprod.
Fertil. Suppl. 21, 59–88.
Benichou, G., Malloy, K.M., Tam, R.C., Heeger, P.S., Fedoseyeva, E.V., 1998. The presentation of self and
allogeneic MHC peptides to T lymphocytes. Hum. Immunol. 59, 540–548.
Bielefeldt-Ohmann, H., Sabara, M., Lawman, M.J., Griebel, P., Babiuk, L.A., 1988. A monoclonal antibody
detects macrophage maturation antigen which appears independently of class II antigen expression. Reactivity
of monoclonal EBM11 with bovine macrophages. J. Immunol. 140, 2201–2209.
Davies, C.J., Fisher, P.J., Schlafer, D.H., 2000. Temporal and regional regulation of major histocompatibility
complex class I expression at the bovine uterine/placental interface. Placenta 21, 194–202.
Donaldson, W.L., Zhang, C.H., Oriol, J.G., Antczak, D.F., 1990. Invasive equine trophoblast expresses conventional
class I major histocompatibility complex antigens. Development 110, 63–71.
Duello, T.M., Byatt, J.C., Bremel, R.D., 1986. Immunohistochemical localization of placental lactogen in
binucleate cells of bovine placentomes. Endocrinology 119, 1351–1355.
Edwards, J.L., Schrick, F.N., McCracken, M.D., van Amstel, S.R., Hopkins, F.M., Welborn, M.G., Davies, C.J.,
2003. Cloning adult farm animals: a review of the possibilities and problems associated with somatic cell
nuclear transfer. Am. J. Reprod. Immunol. 50, 113–123.
Ellis, S.A., Sargent, I.L., Redman, C.W., McMichael, A.J., 1986. Evidence for a novel HLA antigen found on
human extravillous trophoblast and a choriocarcinoma cell line. Immunology 59, 595–601.
Ellis, S.A., Palmer, M.S., McMichael, A.J., 1990. Human trophoblast and the choriocarcinoma cell line BeWo
express a truncated HLA class I molecule. J. Immunol. 144, 731–735.
Ellis, S.A., Sargent, I.L., Charleston, B., Bainbridge, D.R.J., 1998. Regulation of MHC I gene expression is at
transcriptional and post-transcriptional levels in bovine placenta. J. Reprod. Immunol. 37, 103–115.
C.J. Davies et al. / Animal Reproduction Science 82–83 (2004) 267–280
279
Game, D.S., Lechler, R.I., 2002. Pathways of allorecognition: implications for transplantation tolerance. Transpl.
Immunol. 10, 101–108.
Gogolin-Ewens, K.J., Lee, C.S., Mercer, W.R., Brandon, M.R., 1989. Site-directed differences in the immune
response to the fetus. Immunology 66, 312–317.
Gross, T.S., Williams, W.F., Russek-Cohen, E., 1991. Cellular changes in the peripartum bovine fetal placenta
related to placental separation. Placenta 12, 27–35.
Gunnink, J.W., 1984a. Influence of dilution on the chemotactic properties of cotyledon suspensions. Vet. Q. 6,
57–59.
Gunnink, J.W., 1984b. Post-partum leucocytic activity and its relationship to caesarian section and retained
placenta. Vet. Q. 6, 55–57.
Gunnink, J.W., 1984c. Pre-partum leucocytic activity and retained placenta. Vet. Q. 6, 52–54.
Gunnink, J.W., 1984d. Retained placenta and leucocytic activity. Vet. Q. 6, 49–51.
Hansen, P.J., Bazer, F.W., Segerson Jr., E.C., 1986. Skin graft survival in the uterine lumen of ewes treated with
progesterone. Am. J. Reprod. Immunol. Microbiol. 12, 48–54.
Hansen, P.J., 1998. Regulation of uterine immune function by progesterone-lessons from the sheep. J. Reprod.
Immunol. 40, 63–79.
Hill, J.R., Burghardt, R.C., Jones, K., Long, C.R., Looney, C.R., Shin, T., Spencer, T.E., Thompson, J.A.,
Winger, Q.A., Westhusin, M.E., 2000. Evidence for placental abnormality as the major cause of mortality
in first-trimester somatic cell cloned bovine fetuses. Biol. Reprod. 63, 1787–1794.
Hill, J.R., Schlafer, D.H., Fisher, P.J., Davies, C.J., 2002. Abnormal expression of trophoblast major
histocompatibility complex class I antigens in cloned bovine pregnancies is associated with a pronounced
endometrial lymphocytic response. Biol. Reprod. 67, 55–63.
Hunt, J.S., Andrews, G.U., Wood, G.W., 1987. Normal trophoblasts resist induction of class I HLA. J. Immunol.
138, 2481–2487.
Jiang, S.P., Vacchio, M.S., 1998. Multiple mechanisms of peripheral T cell tolerance to the fetal “allograft”. J.
Immunol. 160, 3086–3090.
Joosten, I., van Eldik, P., Elving, L., van der Mey, G.J.W., 1987. Factors related to the etiology of retained placenta
in dairy cattle. Anim. Reprod. Sci. 14, 251–262.
Joosten, I., Sanders, M.F., Hensen, E.J., 1991a. Involvement of major histocompatibility complex class I
compatibility between dam and calf in the aetiology of bovine retained placenta. Anim. Genet. 22, 455–463.
Joosten, I., van Eldik, P., Elving, L., van der Mey, G.J.W., 1991b. Factors affecting occurrence of retained placenta
in cattle. Effect of sire on incidence. Anim. Reprod. Sci. 25, 11–22.
Joosten, I., Hensen, E.J., 1992. Retained placenta: an immunological approach. Anim. Reprod. Sci. 28, 451–461.
Kelley, L.C., Mahaffey, E.A., Bounous, D.I., Antczak, D.F., Brooks Jr., R.L., 1997. Detection of equine and
bovine T- and B-lymphocytes in formalin-fixed paraffin-embedded tissues. Vet. Immunol. Immunopathol. 57,
187–200.
Kimura, K., Goff, J.P., Kehrli Jr., M.E., Reinhardt, T.A., 2002. Decreased neutrophil function as a cause of retained
placenta in dairy cattle. J. Dairy Sci. 85, 544–550.
Kovats, S., Main, E.K., Librach, C., Stubblebine, M., Fisher, S.J., DeMars, R., 1990. A class I antigen, HLA-G,
expressed in human trophoblasts. Science 248, 220–223.
Kydd, J.H., Butcher, G.W., Antczak, D.F., Allen, W.R., 1991. Expression of major histocompatibility complex
(MHC) class 1 molecules on early trophoblast. J. Reprod. Fert. 44 (Suppl.), 463–477.
Larson, L.L., Ishak, M.A., Owen, F.G., Erickson, E.D., Lowry, S.R., 1985. Relationship of physiological factors
to placental retention in dairy cattle. Anim. Reprod. Sci. 9, 31–43.
Le Bouteiller, P., 2000. HLA-G in the human placenta: expression and potential functions. Biochem. Soc. Trans.
28, 208–212.
Lee, C.S., Gogolin-Ewens, K., White, T.R., Brandon, M.R., 1985. Studies on the distribution of binucleate cells
in the placenta of the sheep with a monoclonal antibody SBU-3. J. Anat. 140, 565–576.
Lee, C.S., Gogolin-Ewens, K., Brandon, M.R., 1986a. Comparative studies on the distribution of binucleate cells
in the placentae of the deer and cow using the monoclonal antibody, SBU-3. J. Anat. 147, 163–179.
Lee, C.S., Wooding, F.B.P., Brandon, M.R., 1986b. Immunogold co-localization of ovine placental lactogen and
the antigen recognized by the SBU-3 monoclonal antibody in sheep placental granules. J. Reprod. Fertil. 78,
653–662.
280
C.J. Davies et al. / Animal Reproduction Science 82–83 (2004) 267–280
Lee, C.S., Ralph, M.M., Gogolin-Ewens, K.J., Brandon, M.R., 1990. Monoclonal antibody (SBU-1 and SBU-3)
identification of cells dissociated from the sheep placentomal trophoblast. J. Histochem. Cytochem. 38, 649–
652.
Loke, Y.W., 1989. Trophoblast antigen expression. Curr. Opin. Immunol. 1, 1131–1134.
Low, B.G., Hansen, P.J., Drost, M., Gogolin-Ewens, K.J., 1990. Expression of major histocompatibility complex
antigens on the bovine placenta. J. Reprod. Fertil. 90, 235–243.
Matsas, D.J., Nebel, R.L., Pelzer, K.D., 1992. Evaluation of an on-farm blood progesterone test for predicting the
day of parturition in cattle. Theriogenology 37, 859–868.
Miyoshi, M., Sawamukai, Y., Iwanaga, T., 2002. Reduced phagocytotic activity of macrophages in the bovine
retained placenta. Reprod. Dom. Anim. 37, 53–56.
Morgan, G., Wooding, F.B., Beckers, J.F., Friesen, H.G., 1989. An immunological cryo-ultrastructural study of a
sequential appearance of proteins in placental binucleate cells in early pregnancy in the cow. J. Reprod. Fertil.
86, 745–752.
Myers, D.A., Reimers, T.J., 1988. Purification and endocrine evaluation of bovine binucleate and mononucleate
trophoblastic cells in vitro. J. Tissue Cult. Meth. 11, 83–88.
Park, G.M., Lee, S., Park, B., Kim, E., Shin, J., Cho, K., Ahn, K., 2004a. Soluble HLA-G generated by proteolytic
shedding inhibits NK-mediated cell lysis. Biochem. Biophys. Res. Commun. 313, 606–611.
Park, Y.H., Joo, Y.S., Park, J.Y., Moon, J.S., Kim, S.H., Kwon, N.H., Ahn, J.S., Davis, W.C., Davies, C.J.,
2004b. Characterization of lymphocyte subpopulations and major histocompatibility complex haplotypes of
mastitis-resistant and susceptible cows. J. Vet. Sci. 5, 29–39.
Reimers, T.J., Dziuk, P.J., 1974. The survival of intrauterine skin autografts and allografts in sheep. J. Reprod.
Fertil. 38, 465–467.
Reimers, T.J., Ullmann, M.B., Hansel, W., 1985. Progesterone and prostanoid production by bovine binucleate
trophoblastic cells. Biol. Reprod. 33, 1227–1236.
Roberts, R.M., Xie, S., Nagel, R.J., Low, B., Green, J., Beckers, J.F., 1995. Glycoproteins of the aspartyl proteinase
gene family secreted by the developing placenta. Adv. Exp. Med. Biol. 362, 231–240.
Rogers, A.M., Boime, I., Connolly, J., Cook, J.R., Russell, J.H., 1998. Maternal-fetal tolerance is maintained
despite transgene-driven trophoblast expression of MHC class I, and defects in Fas and its ligand. Eur. J.
Immunol. 28, 3479–3487.
Schlafer, D.H., Fisher, P.J., Davies, C.J., 2000. The bovine placenta before and after birth: placental development
and function in health and disease. Anim. Reprod. Sci. 60/61, 145–160.
Shomer, B., Toder, V., Egorov, I., Ehrlich, R., 1998. Expression of allogeneic MHC class I antigens by transgenic
mouse trophoblast does not interfere with the normal course of pregnancy. Transgenic Res. 7, 343–355.
Stice, S.L., Strelchenko, N.S., Keefer, C.L., Matthews, L., 1996. Pluripotent bovine embryonic cell lines direct
embryonic development following nuclear transfer. Biol. Reprod. 54, 100–110.
Tafuri, A., Alferink, J., Moller, P., Hammerling, G.J., Arnold, B., 1995. T cell awareness of paternal alloantigens
during pregnancy. Science 270, 630–633.
Wathes, D.C., Wooding, F.B., 1980. An electron microscopic study of implantation in the cow. Am. J. Anat. 159,
285–306.
Wegmann, T.G., 1987. Placental immunotrophism: maternal T cells enhance placental growth and function. Am.
J. Reprod. Immunol. Microbiol. 15, 67–70.
Williams, W.F., Margolis, M.J., Manspeaker, J., Douglass, L.W., Davidson, J.P., 1987. Peripartum changes in the
bovine placenta related to fetal membrane retention. Theriogenology 28, 213–223.
Wooding, F.B.P., Wathes, D.C., 1980. Binucleate cell migration in the bovine placentome. J. Reprod. Fertil. 59,
425–430.
Wooding, F.B.P., 1982. The role of the binucleate cell in ruminant placental structure. J. Reprod. Fert. 31 (Suppl.),
31–39.
Wooding, F.B.P., 1992. Current topic: the synepitheliochorial placenta of ruminants: binucleate cell fusions and
hormone production. Placenta 13, 101–113.
Xie, S., Green, J., Bixby, J.B., Szafranska, B., DeMartini, J.C., Hecht, S., Roberts, R.M., 1997. The diversity
and evolutionary relationships of the pregnancy-associated glycoproteins, an aspartic proteinase subfamily
consisting of many trophoblast-expressed genes. Proc. Natl. Acad. Sci. USA 94, 12809–12816.
Zhou, M., Mellor, A.L., 1998. Expanded cohorts of maternal CD8+ T-cells specific for paternal MHC class I
accumulate during pregnancy. J. Reprod. Immunol. 40, 47–62.




![Anti-MHC class I antibody [ER-HR 52] ab15681 Product datasheet 6 References 1 Image](http://s2.studylib.net/store/data/012449669_1-61566b2deb79d6d5b1dcdf9524974dfd-300x300.png)