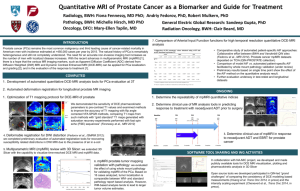
AbstractID: 9770 Title: MRI Simulation for Prostate Cancer
advertisement

AbstractID: 9770 Title: MRI Simulation for Prostate Cancer CT-simulation has become essential in the planning of external beam radiotherapy for prostate cancer. The 3D-localization of the prostate has reduced setup uncertainty and permitted the use of smaller margins. The trade-off is increased interobserver differences, particularly in contouring the apex of the prostate. MRI much more clearly delineates the borders of the prostate, especially the prostate-bladder interface, prostate-rectal interface and apex. MRI also provides greater resolution of tumor location and extent, although MRI-simulation is typically accomplished using a body coil, which has lower resolution as compared to an endorectal coil. Of note, MRI prostate volumes are consistently less than that from CT. One pitfall of MRI-simulation is that commercial planning systems are CT-based. Heterogeneity corrections incorporate CT-based Hounsfield units. Moreover, if fiducial markers or Calypso beacons are outlined on CT, it is best to demarcate the CTVs from the same image set, namely CT, using MRI as a reference. Accurate fusion of CT and MRI is essential in this process. If the fusion is based solely on bony anatomy, the prostate may be in a different position on MRI. The potential errors are magnified if the fiducials are outlined on CT and the anatomy defined on MRI, and the fusion is not based on soft tissue. A rationale for and the potential benefits of functional imaging (MR-spectroscopy and dynamic contrast enhanced MR) to define the dominant tumor prostatic lesion will be described.