Disclosure Planning Delivery
advertisement
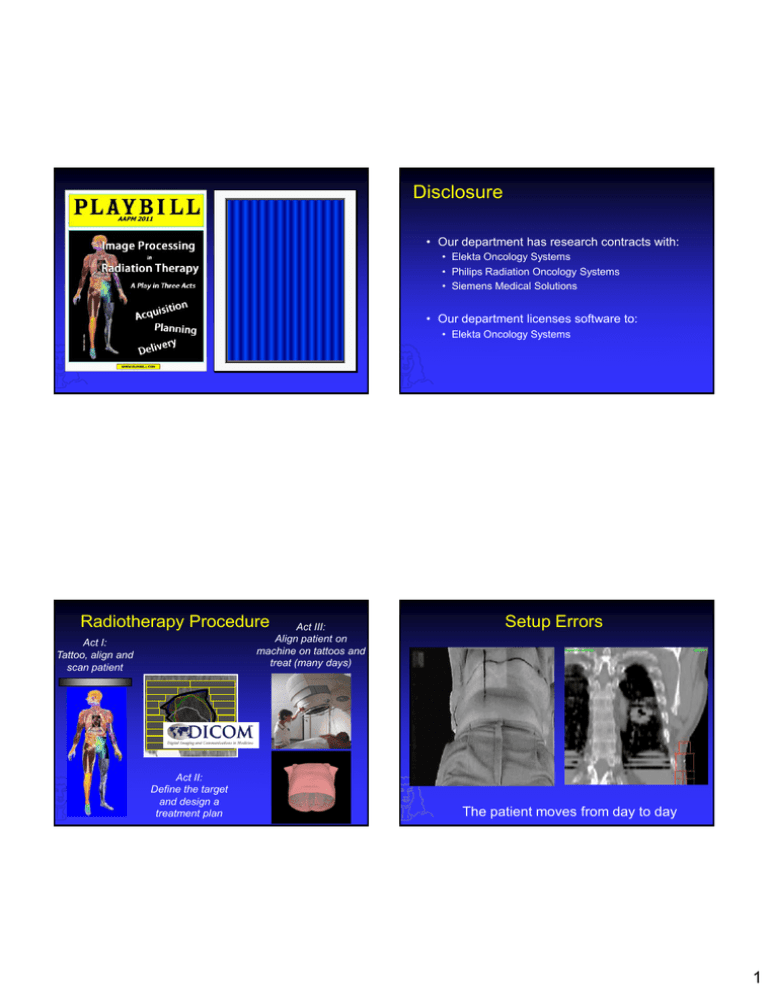
Disclosure AAPM 2011 Act Act III II Planning Delivery Image Processing for T Tx Delivery x Planning Jan-Jakob Marc Kessler Sonke Netherlands The University Cancer of Michigan Institute Radiotherapy Procedure Act III: Align patient on machine on tattoos and treat (many days) Act I: Tattoo, align and scan patient Act II: Define the target and design a treatment plan • Our department has research contracts with: • Elekta Oncology Systems • Philips Radiation Oncology Systems • Siemens Medical Solutions • Our department licenses software to: • Elekta Oncology Systems Setup Errors The patient moves from day to day 1 Organ Motion How can we solve this problem ? Organs move from day to day 1. Use large margins, irradiating too much healthy tissues 2. Use small margins, and risk missing the target 3. Or: use image guided radiotherapy Image Guided Radiotherapy Safety Margins • Image the tumor + organs-at-risk or their surrogates just prior or during treatment • Assess changes in patient position relative to treatment plan • Adapt treatment plan (couch shift) to account for changes, increasing treatment precision Verellen et al. Nature Reviews Cancer 2007 2 Many In-room Imaging Systems Visualization Visualization: Image Fusion Reference Image Visualization: Sliding Window Localization Image 3 Visualization: Overlay Complementary color overlay clearly shows gross differences and local differences provided adequate contrast Bone Registration Visualization: Animation Animation clearly shows local changes Bone Registration 4 Pop Quiz What is the purpose of IGRT 19% 20% 20% 21% 20% 1. 2. 3. 4. 5. Make pretty images Minimize setup errors Quantify organ motion Reduce PTV margins Sell more expensive treatment machines Pop Quiz What is the purpose of IGRT a) Make pretty images b) Minimize setup errors c) Quantify organ motion d) Reduce PTV margins e) Sell more expensive treatment machines Correct Answer: d) Seminars in Radiation Oncology Volume 17, Issue 4 Electronic Portal Imaging 2D Image Guidance 5 Portal Image Quality Preprocessing: unsharp masking Image quality is limited by: • Projective nature of 2D images A-P • Low DQE of EPIDs in MV range • Limited dose used for imaging (ALARA) Lat . Prostate • Limited contrast differences of tissue in the MV range Lung Mostly limited to bony anatomy alignment minimizing setup errors Top-hat transform Portal image analysis - 2D Reference image Match field-edge Match anatomy Original image Binary top-hat enhanced image Setup Error = Anatomy Match – Field-Edge Match 6 3D EPID Dose reconstruction prostate VMAT plan 3D Image Guidance EPID movie • Energy: 10 MV • 243 frames • delivery time: 96 s Dose per frame Accumulated dose axial slice through isocentre Jean-Pierre Bissonnette: PMH MV/kV Coincidence Jean-Pierre Bissonnette: PMH kV/MV Calibration Concept BB (reconstruction Isocentre) MV mechanical isocentre kV y • Treatment and imaging beams are orthogonal MV radiation isocentre x Calibrated isocentre z 7 2. Repeat MV Localization of BB for gantry angles of 90o, 180o, and 270o. 3. Analyze images and adjust BB to Treatment Isocentre (± 0.3 mm) +1mm qgantry qgantry u -1mm -180 v qgantry Jean-Pierre Bissonnette: PMH 1. MV Localization (0o) of BB; collimator at 0 and 90o. Geometry: Flex calibration +180 Reconstruction 4. Measure BB Location in kV radiographic coordinates (u,v) vs. q gantry. 5. Analysis of ‘Flex Map’ and Storage for Future Use. 6. Employment of ‘Flex Map’ During Routine Clinical Imaging. MV Flex kV Flex Geometry: Flex calibration 0.5 0.4 displacement [cm] 0.3 0.2 0.1 0 -0.1 X Y -0.2 -200 MV Flex kV Flex -150 -100 -50 0 50 G G 100 (AB) (GT) 150 200 ° angle [ ] 8 Marc Kessler / UM Geometric non-idealities (Flex) How many Degrees of Freedom? PET/CT 2 mm panel shift Correctly Calibrated Requirements for IGRT registration MR - CT 4D CT 0? 3 to 6 3xN None ? Few Many Automatic matching on region of interest built-in in Synergy system reference localization reference localization • Fast and robust image registration • Easy visual validation • Registration result drives a couch shift Rigid registration with 6 degrees of freedom is a likely candidate Tumor in top of neck Required table shift: (-3.2, -1.5, -0.6) mm Tumor in lower part of neck Required table shift: (+1.5, -3.2, -6.1) mm 9 Rotations Rotations Correction by Couch Shift Modify Rotation Point 10 Correction by Couch Shift Soft Tissue Guidance Grey-value registration TAP / TCC / TLR / RAP / RCC / RLR ** Smitsmans et al., IJROBP 60 (2004) Automatic prostate localization in CBCT (30 s) Pop Quiz How many degrees of freedom are typically used for IGRT image registration Cone beam CT 10 CBCT scans: automatic bone match 24% 20% 23% 16% 17% Planning CT contours placed automatically 1. 2. 3. 4. 5. 0 3 6 42 Not enough 10 CBCT scans: automatic prostate match help line (GTV+3.6 mm) Smitsmans et al., IJROBP 2004, 2005 11 Martin LaChaine: Elekta Ultrasound Guided RT (Clarity™) Pop Quiz Clarity Sim How many degrees of freedom are typically used for IGRT image registration a) 0 b) 3 c) 6 d) 42 e) Not enough Clarity AFC Workstation Clarity Guide Throughout Radiation Oncology Care Cycle Sim Frank Verhaegen: Maastro Correct Answer: c) Van Herk et al. Seminars in Radiation Oncology, 2007 Linac Frank Verhaegen: Maastro 3DUS vs CT for breast seroma cavity Planning CT Daily US Fusion 12 Radiotherapy systems with integrated MRI 1.5 T MRI accelerator for MRI guided RT at UMC Utrecht Bas Raaymakers: UMC Prototype MRI accelerator MRI-Linac Utrecht Courtesy of Bas Raaijmaakers MRI-Co60 ViewRay Courtesy of Jim Dempsey No impact of beam on MRI Bas Raaymakers: UMC Inter- and intra- fracation motion of cervix 4D Image Guidance Day to day variation 13 Breathing Respiratory signal extraction Vertical derivative filter Horizontal projection Temporal concatenation [Zijp, ICCR, 2004] [van Herk, ICCR, 2007] Amsterdam shroud (2D image) RCCBCT 3D versus 4D CBCT • 4D Data set • 8 x 84 projections • 3D Data set • 670 projections 14 ROI by GTV Expansion 4D CBCT + GTV Contour Local Rigid Body Registration Visual Validation 15 Apply Correction Impact of Respiratory Motion on Dose Distribution Planned distribution Delivered distribution • Shift of the dose distribution due to displacement of the mean tumor position • Blurring of the dose distribution due to breathing around the mean position Planned dose distribution: hypofractionated lung treatment 3x18 Gy Realized dose distribution with daily IGRT on tumor (no gating) 2 cm 9 mm margin is adequate even with 2 cm intrafraction motion 16 Jim Dempsey / ViewRay Bas Raaymakers: UMC 1D MRI, Navigator echos (NE) 15 ms per acquisition 1D MRI signal 4D Liver MRI Time Monitoring breathing at superior side of liver Bas Raaymakers: UMC • In diagnostics used to track/gate respiration • Imaging stack is moved according to NE signal • Diaphragm monitored • Can be positioned anywhere in any orientation Bas Raaymakers: UMC 1D MRI navigators, monitoring breath hold stability and on-set of breathing Gated radiation on moving cart • Cart in scanner bore, moving along FH-direction • Motion by electric motor/crankshaft mechanism • Radiation sensitive film to record dose • Water phantom to track position • 5x5 cm2 radiation beam, dose ~2Gy, in static situation T = 2.5 min. 1D MRI signal • Sinusoidal/respiratory-like motion Time Monitoring breath hold at inferior side of liver 17 Bas Raaymakers: UMC Gated radiation delivery Pop Quiz Which motion management strategy has the largest impact on the delivered dose: 18% 22% 20% 20% 20% 1. 2. 3. 4. 5. 4D Imaging 4D Planning 4D Delivery 4D Image Guidance The impact of respiration is over exaggerated Pop Quiz Which motion management strategy has the largest impact on the delivered dose: a) 4D Imaging b) 4D Planning c) 4D Delivery d) 4D Image Guidance e) The impact of respiration is over exaggerated Adaptive Radiotherapy Correct Answer: d) Guckenberger et al. Radiother. Oncol. 2009 18 Differential Variability Repeat 4D cone beam CT No couch correction can solve this problem Shows respiration, tumor shrinkage and baseline position variation Fraction at day # 36 Anatomical Changes Bony anatomy registration non-rigid registration 19 Results, volume change of target + OAR Deformable Registration Relative weight loss, neck radius and delineated volumes 1.10 1.00 CTV PTV Brain stem Left parotid Spinal cord Oral Cavity 1 Neck 0.80 0.8 weight 0.70 CTV Volume [%] units 0.90 PTV tot 0.60 Spinal cord Parotid Li 0.50 Parotid Re 0.40 0 5 10 15 20 25 30 35 40 0.6 0.4 treatment day day 0 1 7 14 21 28 36 CTV 387 381 378 373 373 344 315 PTV 1051 1036 1035 1008 1012 969 916 Spinal cord 20 20 20 20 20 21 20 Parotid Li 31 31 32 27 28 23 18 Parotid Re 21 21 21 20 19 17 15 t(s) 67 120 104 55 141 155 0.2 0 0 Pre-treatment Applications – dose painting 0.4 0.6 0.8 Dose [% Dmax] 1 1.2 1.4 Summary • Geometrical uncertainties limit the precision of radiotherapy Prescription function Treatment response Mid-treatment 0.2 • 2D,3D&4D image registration and guidance increases the precision of RT allowing margin reduction and dose escalation • Adaptive RT further individualized treatment delivery Robert Jeraj / UW 20 Acknowledgements Marcel van Herk Peter Remeijer Jochem Wolthaus Simon van Kranen Simon Rit Monique Smitsmans Anton Mans David Jaffray Doug Mosely Marc Kessler Jean-Pierre Bissonnette Robert Jeray Frank Verhaegen Bas Raaymakers Jim Dempsey Martin LaChaine 21