8/1/2011 Contents Routine Ultrasound Equipment Tests for Quality Assurance
8/1/2011
Routine Ultrasound Equipment Tests for
Quality Assurance
James A. Zagzebski, Ph.D.
Dept. of Medical Physics
University of Wisconsin, Madison, WI, USA
Contents
•
How we do US QA in our institution
•
Guidelines available from US facility accreditation bodies
(ACR; AIUM)
•
Emphasis is given to safety, cleanliness, and very basic performance tests.
•
Most common fault is transducer damage, element dropout.
•
Issues related to image performance, such as spatial resolution, are not included in QA (except ACR breast).
• Traditional “parameters” such as distance measurements are believed by many to be unnecessary for “routine” testing. Included in some protocols, as demands and challenges increase.
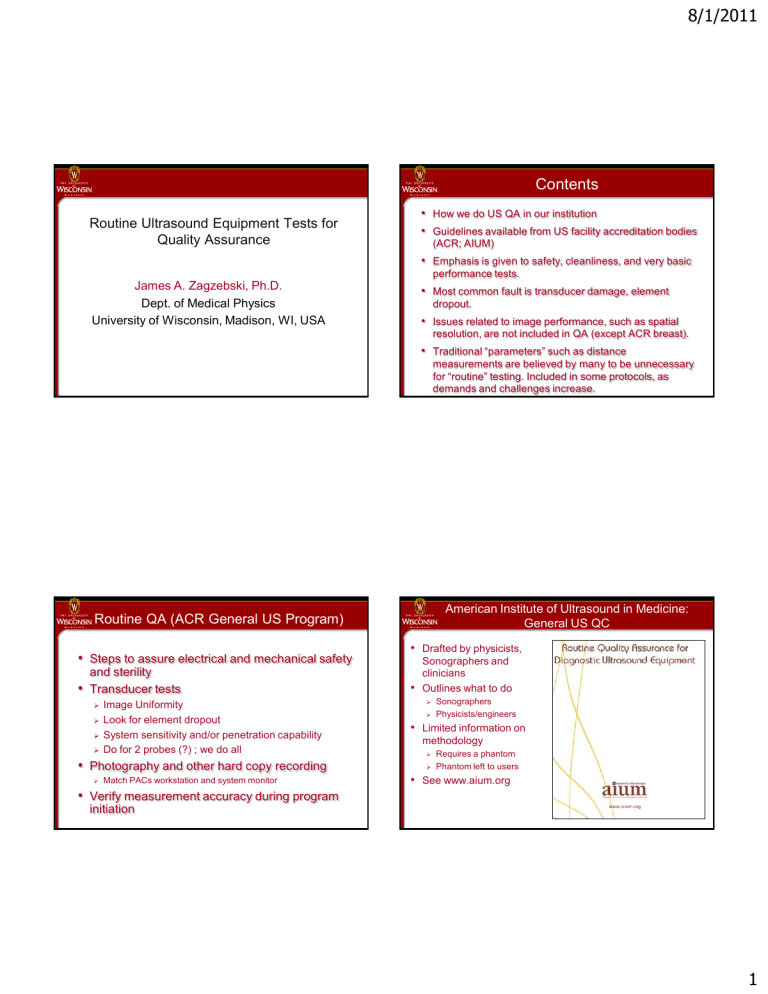
Routine QA (ACR General US Program)
•
Steps to assure electrical and mechanical safety and sterility
•
Transducer tests
Image Uniformity
Look for element dropout
System sensitivity and/or penetration capability
Do for 2 probes (?) ; we do all
•
Photography and other hard copy recording
Match PACs workstation and system monitor
•
Verify measurement accuracy during program initiation
American Institute of Ultrasound in Medicine:
General US QC
•
Drafted by physicists,
Sonographers and clinicians
•
Outlines what to do
Sonographers
Physicists/engineers
•
Limited information on methodology
Requires a phantom
Phantom left to users
•
See www.aium.org
1
American Institute of Ultrasound in Medicine: General
Sonography (physicist, engineer)
•
Cables OK, air filters clean, mechanical and electrical inspection
•
Transducer Uniformity
Phantom
Electronic probe tester
•
Sensitivity, Maximum depth of visualization into a phantom
•
Distance measurement accuracy
•
Target detection and imaging
Focal targets such as simulated cysts or low contrast objects
Choice of phantoms left to users
•
Image display fidelity
•
Minimum frequency: annual for physicists/engineer tests
Routine QA: Cleanliness, safety
Transducer Inspection
Delaminations
Frayed cables
Proper cleaning
Console
Air filters
Viewing monitor, keyboard clean
Lights, indicators
Wheels, wheel locks
Proper cleaning
8/1/2011
Currently used materials:
Water-based gels
Advantages:
Speed of sound = 1540 m/s
Attenuation proportional to frequency
Backscatter
Disadvantages:
Subject to desiccation (?)
Must be kept in containers
Requires scanning window
Currently used TM materials:
•
Solid, non-water-based materials (urethane)
•
Advantages:
Not subject to desiccation
No need for scanning window; possibility for soft, deformable scanning window
Produce tissue-like backscatter
Disadvantages:
C= 1430-1450 m/s
Attenuation not proportional to frequency (~f 1.6
)
Surface easily damaged if not cleaned regularly to remove gels
2
Maximum Depth of Visualization
•
Considered by many as a good overall check of the integrity of the system
•
FOV at 18 cm (or set to match the phantom)
•
Output power (MI) at max
•
Transmit focus at deepest settings
•
Gains, TGC for visualization to the maximum distance possible
Maximum Depth of Visualization
How far can you see the speckle pattern in the material?
8/1/2011
Objective Maximum Depth of Visualization
• Gibson, Dudley, Griffith, “A computerized Quality Control System for
Bmode Ultrasound,” Ultrasound Med Biol 27 :1697-1711, 2001.
•
Shi, Al-Sadah, Mackie, Zagzebski, Signal to Noise Ratio Estimates on Ultrasound Depth of Penetration (abstract only), Medical Physics
30 : 11367, 2003.
•
Gorny, Tradup, Bernatz, Stekel, and Hangiandreou , “Evaluation of an Automated Depth of Penetration Measurement ofr the Purpose of
23: S76, 2004.
•
Compute mean pixel value vs depth for phantom (signal) and for noise only (noise)
•
Depth where signal/noise = 1.5 =DOP
Routine QA: Image Uniformity
Considered to be the most important and useful test!
Ideally:
No evidence of element dropout
No vertical
„shadows‟
3
Uniformity
Turn off spatial compounding, speckle reduction
Use 1 tx focus
Search for
“shadows” emanating from transducer
Common in new and old probes!
Checking uniformity for curvilinear transducers
•
Solution 1: rock transducer from side to side
•
Solution 2: Use a liquid TM material
•
Solution 3: Use newer phantoms with special curved windows
8/1/2011
Difficulties with Uniformity (coupling)
•
Solution 1: rock transducer from side to side
Need Proper Technique to Detect Element Dropout
Transducer with severe element dropout scanned using compound imaging
4
Need Proper Technique to Detect Element Dropout
Transducer with severe element dropout
Disable spatial compounding
Use single, shallow transmit focus
Difficulties with Uniformity
•
Visualizing 1-2 element dropouts
•
Use persistence; translate transducer.
8/1/2011
Difficulties with Uniformity
•
Visualizing 1-2 element dropouts
•
Record Image loops while translating the transducer;
•
Compress a 100 frame loop into 1 image (averages speckle) - Project of the AAPM
1 image
Ultrasonix SonixTouch
Enables masking off individual elements
Elements 95 and 96 masked
Difficulties with Uniformity
•
Visualizing 1-2 element dropouts
•
Record Image loops while translating the transducer;
•
Compress a 100 frame loop into 1 image (averages speckle)
•
Computer analysis
Average image
Ultrasonix SonixTouch
Enables masking off individual elements
Elements 95 and 96 masked
5
Gray Scale Photography, Workstation Fidelity
•
Important for monitor on machine to be set up properly to view all echo levels available and entire gray bar pattern.
Set up during acceptance testing
Take steps to avoid the “meat hook” effect (mark or inscribe contrast and brightness controls)
•
Workstation monitors and/or hardcopy devices should be matched to the machine monitor.
AAPM,August, 2011
Check hardcopy, workstation displays.
Are all gray bar transitions visible?
8/1/2011
SMPTE or Other Gray Scale Test Pattern
•
Available on some scanners
•
0% to 100% gray bar pattern
•
Squares for detecting geometric distortion
•
Are all gray transitions visible?
Result of a recent test of system monitor
•
After seeing the test result, the sonographer mentioned that images being sent for accreditation tended to be washed out, cysts seemed to be filled in.
•
Sonographers were
“over-gaining” the machine to compensate for the poor monitor performance.
Pacs
Workstation
Logiq 9
Monitor
(simulation)
6
Distance Measurement Accuracy: Vertical
Actual 2.5
Measure 2.46
error 1.5%
Acceptable
Distance Measurement Accuracy: Horizontal
Actual 1.0
Measure 1.01
error <1%
Acceptable
8/1/2011
Routine QA (ACR General US Program)
•
Distance Measurement
Accuracy tests
Necessary?
(“Scanner is a transducer tied to a computer.”)
May be important for specific uses
• Images reregistered from 3-D data sets
• Workstation measurements
• Radiation seed implants
Acquisition Plane
(Normal 2-D view)
Reconstructed Elevational Plane
4-year Experience with a clinical ultrasound quality control program Hangiandreou et al, Mayo Clinic, Rochester, Minnesota,
•
About 50 scanners (47-55 over the 4 year period; most Siemens and a few Philips)
•
About 300 transducers (267-322 over the 4 year period)
•
Quarterly assessments of:
Depth of penetration
Distance measurement accuracy
Transducer uniformity (element dropout)
Mechanical integrity
7
8/1/2011
4-year Experience with a clinical ultrasound quality control program,
(Ultrasound Med Biol 37, 1350-1357, 2011)
Hangiandreou et al, Mayo Clinic, Rochester, MN
Minnesota, USA
Evaluation
Method
# of detected
“failures”
% of detected
“failures”
47 25.1
Mechanical
Integrity
Image uniformity
Distance
Accuracy
DOP
(penetration)
124
0
3
66.3
0.0
1.6
Clinical
Problems
TOTAL
13
187
7.0
100.
4-year Experience with a clinical ultrasound quality control program,
(Ultrasound Med Biol 37, 1350-1357, 2011)
Hangiandreou et al, Mayo Clinic, Rochester, MN , USA
Evaluation
Method
Mechanical
Integrity
Image uniformity
Distance
Accuracy
DOP
(penetration)
Clinical
Problems
TOTAL
# of detected
“failures”
47
124
0
3
13
187
% of detected
“failures”
25.1
Recommendation
Quarterly
66.3
0.0
1.6
7.0
100.
Quarterly
Annually
Annually, (if done with software)
Sonographer‟s daily inspections
Image of a phantom is useful for qualitative comparisons!
(DOP or Distance Measureent)
Image of a phantom is useful!
Conventional Spatial Compounding
Images obtained during routine Breast QC testing, 3/2010
Conventional Spatial Compounding
Images obtained 1 month later, after a software change;
8
Potentially Useful Aids
Use Stored Presets
Sonographers can set up
FOV
Focus
Gain
Compound off, etc
Generate a backup
updates often wipe out old presets
Summary
•
Setting up, maintaining an equipment QA program is straight forward
•
The ACR listed procedures are a useful, basic QA program
Directed by physicist or lab personnel
Integrated effort including lab and technical staff
Requires a Phantom
Closely correlates with AIUM list of factors needing to be tested
• Transducer uniformity is a frequent fault in today‟s scanning machines. I recommend testing ALL transducers.
•
Computational methods can be developed for objective tests
8/1/2011
References
• Goodsitt et al, “Real-time B-mode ultrasound quality control test procedures”, Medical Physics 1998; 25:1385-1406.
• J Zagzebski, “US quality assurance with phantoms.” In Categorical
Course in Diagnostic Radiology Physics: CT and US Cross-Sectional
Imaging, Edited by L. Goldman and B. Fowlkes, 2000, Oak Brook, IL:
Radiological Society of North America, pp. 159-170.
• J Zagzebski and J Kofler, “Ultrasound Equipment Quality Assurance,” in Quality Management in the Imaging Sciences, ed. By J Papp, 2002,
St. Louis, Mosby, pp. 207-215.
•
QA Manual for Gray Scale Ultrasound Scanners, 1995, American
Institute of Ultrasound in Medicine, Laurel, MA.
• D Groth et al, “Cathode ray tube quality control and acceptance program: initial results for clinical PACS displays, Radiographics
2001, 21: 719.
•
Hangiandreou, Stekel, Tradup, Gorny, and King, Four-Year experience with a clinical ultrasound quality control program, UMB
2011, 37: 1350-57.
9