Estimating Cancer Risk Attributable to Computed Tomography Coronary Tomography Coronary Angiography
advertisement
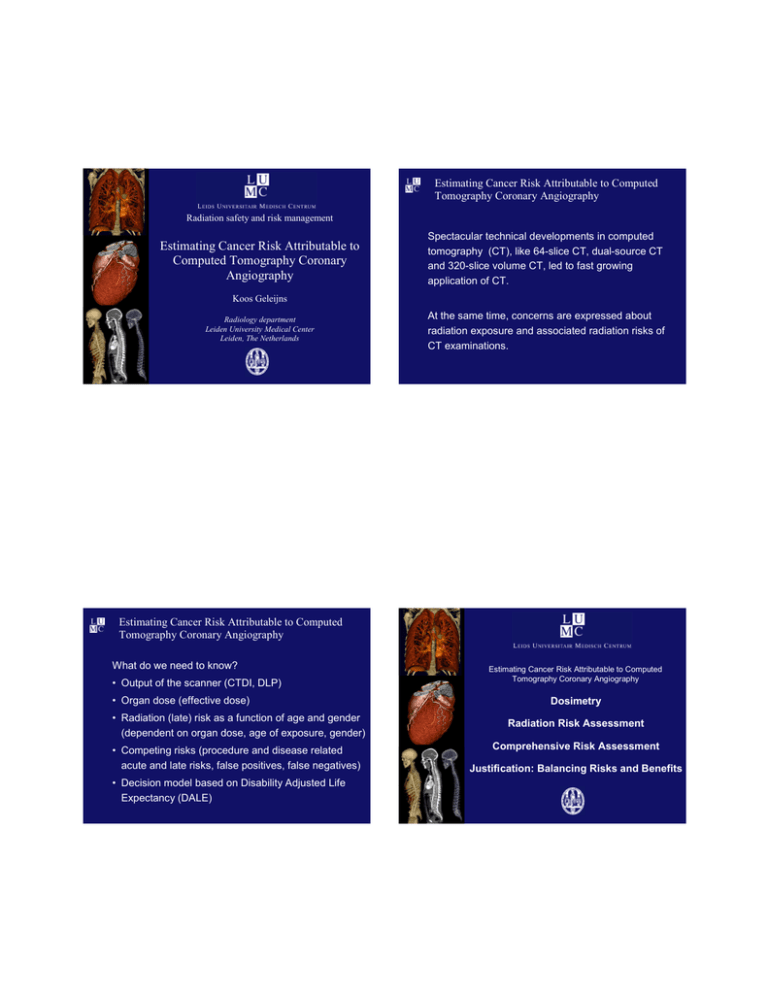
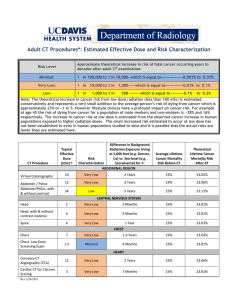
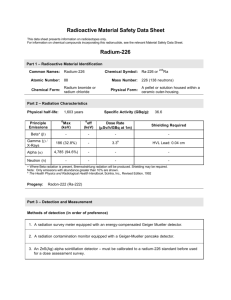
Estimating Cancer Risk Attributable to Computed Tomography Coronary Angiography Radiation safety and risk management Estimating Cancer Risk Attributable to Computed Tomography Coronary Angiography Spectacular technical developments in computed tomography (CT), like 64-slice CT, dual-source CT and 320-slice volume CT, led to fast growing application of CT. Koos Geleijns Radiology department Leiden University Medical Center Leiden, The Netherlands At the same time, concerns are expressed about radiation exposure and associated radiation risks of CT examinations. Estimating Cancer Risk Attributable to Computed Tomography Coronary Angiography What do we need to know? • Output of the scanner (CTDI, DLP) • Organ dose (effective dose) • Radiation (late) risk as a function of age and gender (dependent on organ dose, age of exposure, gender) • Competing risks (procedure and disease related acute and late risks, false positives, false negatives) • Decision model based on Disability Adjusted Life Expectancy (DALE) Estimating Cancer Risk Attributable to Computed Tomography Coronary Angiography Dosimetry Radiation Risk Assessment Comprehensive Risk Assessment Justification: Balancing Risks and Benefits Dosimetry, general considerations • Operational dose quantities, easy Estimating Cancer Risk Attributable to Computed Tomography Coronary Angiography • Measurable but also rather accurately provided on the operators console • Computed Tomography Dose Index (CTDI, mGy) Dosimetry Radiation Risk Assessment Comprehensive Risk Assessment Justification: Balancing Risks and Benefits • Dose Length Product (DLP, mGy.cm) • Dose quantities required for risk assessment, more difficult • Not measurable! Should be measured in anthropomorphic phantoms or calculated for (mathematical or voxel) phantoms • Organ dose (HT, mSv) • Effective dose (E, mSv) Dosimetry, organ dose and effective dose assessment Dosimetry, organ dose and effective dose assessment Toshiba 64 slice, medium bow tie filter, measured nCTDIw 8.6 mGy/100 mAs • Several software applications are available • CT Expo • WinDose • ImPACT CT Patient Dosimetry Calculator • The software may be inaccurate • It does not accommodate patients of different sizes • It is not validated for modern scanners • It does not allow the off-center position of the patient in cardiac CT Note: Look up of nCTDIw for Aquilion 16 was 14.3 mGy/100mAs, measured 8.6 mGy/100mAs! Calculation of organ dose for the Toshiba Aquilion ONE scanner (own research) 1x5 4x1 16 x 0.5 64 x 0.5 320 x 0.5 1998 2001 2004 2008 Dosimetry, organ dose and effective dose assessment New scanners, e.g. Toshiba Aquilion ONE, 320 slice Dosimetry, organ dose and effective dose assessment CT scan Entire trunk, male Different sizes Organ segmentation Dose calculation Dosimetry, organ dose and effective dose assessment Dosimetry, k-factor of 0.017 mSv/(mGy.cm) Core64: size and gender adepted acquisition protocols • K-factor • Simple assessment of effective dose from dose length product • Defined for a general chest CT (120 kV) and a normal sized patient, derived from dose characteristics of old, axial scanners • The k-factor may be inaccurate in CT Coronary Angiography • It was not derived for CT Coronary Angiography • It does not accommodate patients of different sizes • It is not validated for modern scanners Dosimetry, organ dose and effective dose assessment • The k-factor of 0.017 mSv/(mGy.cm) may be inaccurate in CT Coronary Angiography Estimating Cancer Risk Attributable to Computed Tomography Coronary Angiography • We derived higher k-factors for CTCA of respectively • 0.030 mSv/(mGy.cm), 0.030 mSv/(mGy.cm) and 0.024 mSv/(mGy.cm) for small, normal and obese female voxel phantoms; • 0.023 mSv/(mGy.cm); 0.018 mSv/(mGy.cm) and 0.020 mSv/(mGy.cm) for small, normal and obese male voxel phantoms. Dosimetry Radiation Risk Assessment Comprehensive Risk Assessment Justification: Balancing Risks and Benefits • The k-factor for chest CT yielded systematic and substantial underestimation of effective dose. Risk of radiation induced cancer – The Lancet Risk of radiation induced cancer – The Lancet International popular press The Lancet, 2004 Current risk estimations of radiation induced cancer Example of a radiation risk model • Methods for calculation of radiation induced mortality: The BEIR VII ERR (excess relative risk) model • One single effective dose dependent risk coefficient, e.g. 0.05 per Sv ERR model: the excess radiation risk is expressed relative to the background risk: (s,a,b,d) = (s,a,b) [1 + Better: (s,a,b): • Organ dose dependent risk coefficient from BEIR VII, as a function of: • Age and • Gender s ERR(e,a)d] background rate at zero dose, depends on sex (s), attained age (a), and birth cohort (b). s ERR(e,a): ERR unit of dose, depends on sex (s), age at exposure (e), and attained age (a). d: dose ERR(e,a): exp ( e*) a , where e* is equal to e – 30 when e < 30, and equal to zero when e 30 Excess radiation risk is expressed relative to the background risk Example of a radiation risk model The BEIR VII risk model, parameters s, and are provided: ERR Model for Estimating Mortality from SiteSpecific Solid Cancer Mortality leukemia mortality all solid cancer mortality Age-time patterns in radiation-associated risks for all solid cancer mortality and leukemia mortality. Curves are sex-averaged estimates of the risk at 1 Sv for people exposed at age 10 (solid lines), age 20 (dashed lines), and age 30 or more (dotted lines). How to assess radiation risk, e.g. years life lost Example of a radiation risk model, based on dose assessment Dose assessment, organ dose and effective dose (mSv) CCTA CAG Bone marrow 11.0 3.7 Stomach 6.9 2.3 Colon 0.1 0.0 Liver 10.0 3.3 Lung 58.0 19.3 Breast 69.0 23.0 Prostate 0.1 0.0 Uterus 0.1 0.0 Ovary 0.1 0.0 Bladder 0.0 0.0 Other solid cancers 15.0 5.0 Thyroid 0.9 0.3 Effective dose 15 5 Life tables that represent age and gender related functions pertaining to mortality. age <1 1-2 2-3 3-4 4-5 5-6 6-7 7-8 8-9 9 - 10 10 - 11 … … 70 - 71 71 - 72 72 - 73 73 - 74 74 - 75 … … ax 0.33 0.5 0.5 0.5 0.5 0.5 0.5 0.5 0.5 0.5 0.5 … … 0.5 0.5 0.5 0.5 0.5 … … Mx 0.004551 0.000391 0.000252 0.000197 0.000167 0.00014 0.000148 0.000135 0.000129 0.000117 0.000129 … … 0.086713 0.089787 0.093459 0.096347 0.100576 … … qx 0.004537 0.000391 0.000252 0.000197 0.000167 0.00014 0.000148 0.000135 0.000129 0.000117 0.000129 … … 0.083109 0.085929 0.089286 0.091919 0.095761 … … px 0.995463 0.999609 0.999748 0.999803 0.999833 0.99986 0.999852 0.999865 0.999871 0.999883 0.999871 … … 0.916891 0.914071 0.910714 0.908081 0.904239 … … lx 100000 99546.28 99507.37 99482.3 99462.7 99446.09 99432.17 99417.45 99404.03 99391.21 99379.58 … … 40797.24 37406.61 34192.3 31139.39 28277.1 … … nd x 453.7165 38.91499 25.0727 19.59608 16.60888 13.92148 14.71487 13.42045 12.82229 11.62809 12.81914 … … 3390.631 3214.313 3052.906 2862.293 2707.829 … … Lx 99696.01 99526.83 99494.83 99472.5 99454.4 99439.13 99424.81 99410.74 99397.62 99385.4 99373.17 … … 39101.93 35799.46 32665.85 29708.25 26923.19 … … Tx 6786114 6686418 6586891 6487397 6387924 6288470 6189031 6089606 5990195 5890797 5791412 … … 344851 305749 269949 237283 207575 … … ex 67.86114 67.16894 66.19501 65.21157 64.22432 63.23496 62.24374 61.25288 60.26109 59.2688 58.27567 … … 8.452792 8.173653 7.89503 7.620038 7.34075 … … qx: Conditional probablity that an individual who has survived to start of the age interval will die in the age interval. How to assess radiation risk, e.g. years life lost Mx qx px lx dx Lx Tx ex Life tables that represent age and gender related functions pertaining to mortality. In a cohort of 100000 males 61 radiation induced deaths, in a cohort of 100 000 females 147 radiation induced deaths. Fraction of the age interval lived by those in the cohort population who die in the interval. Age-specific death rate. Conditional probability that an individual who has survived to start of the age interval will die in the age interval. Conditional probability that an individual entering the age interval will survive the age interval. Life table cohort population. Number of life table deaths in the age interval Number of years lived during the age interval. Cumulative number of years lived by the cohort population in the age interval and all subsequent age intervals. Life expectancy at the beginning of the age interval. Radiation induced mortality is a late effect: reduction of life expectancy 3 days (males) and 9 days (females). Survival, cohort of 100 000 ax Survival, exposure to 15 mSv at age 40 80000 60000 Males, no radiation Females, no radiation Males, with radiation (15mSv) Females, with radiation (15 mSv) 40000 20000 0 0 20 40 60 Age, years Estimating Cancer Risk Attributable to Computed Tomography Coronary Angiography Dosimetry Radiation Risk Assessment Comprehensive Risk Assessment Justification: Balancing Risks and Benefits These data support the calculation of Disability Adjusted Life Expactancy (DALE). 100000 80 100 120 Current risk estimations of radiation induced cancer Methods for calculation of radiation induced mortality: Comparison of CCTA and CAG Consider radiation exposure from CCTA (15 mSv) and CAG (5 mSv), but also the fatal complications of diagnostic cardiac catheterization • One single dose dependent risk coefficient, e.g. 0.05 per Sv • Dose dependent risk coefficient as a function of: • Age and/or • Gender • Suggested improvements, taking into account in the life tables: • Disease related morbidity and mortality • Other acute and late risks, e.g.: • Imaging procedure related acute risks • Risk of missing a diagnosis Comprehensive Risk Assessment de Bono D. Complications of diagnostic cardiac catheterisation: results from 34 041 patients in the United Kingdom confidential enquiry into cardiac catheter complications. Br Heart J 1993; 70:297-300 Comprehensive Risk Assessment • Invasive coronary angiography (CAG) 30 • Assume organ doses that correspond with an effective dose of 5 mSv and the BEIR VII organ dose specific late radiation risks 0.11% acute CAG mortality 20 5 mSv CAG 15 10 5 25 • Assume organ doses that correspond with an effective dose of 15 mSv and the BEIR VII organ dose specific late radiation risks 15 mSv CCTA 20 Days life lost 25 Days life lost • Non Invasive CT Coronary Angiography (CTCA) 30 15 10 5 0 20 30 40 50 60 70 Age at CAG 80 90 100 • Assume an acute CAG mortality risk of 0.11% *) *) Noto TJ et al.. Cardiac catheterization 1990: a report of the Registry of the Society for Cardiac Angiography and Interventions (SCA&I). Cathet Cardiovasc Diagn 1991 October;24(2):75-83. 0 20 30 40 50 60 70 Age at CCTA 80 90 100 • Assume no acute mortality risk for non invasive CTCA Comprehensive Risk Assessment 30 30 25 25 0.11% acute CAG mortality 15 15 10 10 5 5 0 Dosimetry 15 mSv CCTA 20 5 mSv CAG Days life lost Days life lost 20 Estimating Cancer Risk Attributable to Computed Tomography Coronary Angiography Radiation Risk Assessment Comprehensive Risk Assessment Justification: Balancing Risks and Benefits 0 20 30 40 50 60 70 Age at CAG 80 90 100 20 30 40 50 60 70 80 90 100 Age at CCTA Medical decision making for symptom-based diagnosis …a sign is an objective symptom of a disease; a symptom is a subjective sign of disease… Clinical decisions may be supported by objective clinical decision rules Probability of CAD in % as function of age, gender and type of chest pain Age Non-anginal Atypical Angina Typical Angina Chest Pain Year Men Women Men Women Men Women 30-39 5.2±0.8 0.8±0.3 21.8±2.4 4.2±1.3 40-49 14.1±1.3 2.8±0.7 46.1±1.8 13.3±2.9 87.3±1.0 55.2±6.5 50-59 21.5±1.7 8.4±1.2 58.9±1.5 32.4±3.0 92.0±0.6 79.4±2.4 60-69 28.1±1.9 18.6±1.9 67.1±1.3 54.4±2.4 94.3±0.4 90.6±1.0 69.7±3.2 25.8±6.6 Hamm CW, Goldmann BU, Heeschen C, Kreymann G, Berger J, Meinertz T. Emergency room triage of patients with acute chest pain by means of rapid testing for cardiac troponin T or troponin I. N Engl J Med 1997; 337:1648-53. Bayesian network for probability of CAD based on the most important test results prior to imaging or intervention Decision analysis is based on the premise that humans are reasonably capable of framing a decision problem, listing possible decision options, determining relevant factors, and quantifying uncertainty and preferences, but are rather weak in combining this information into a rational decision. A Bayesian network, or belief network, shows conditional probability and causality relationships between variables. Probability of CAD, male 45 years old Probability of CAD, male 45 years old Chest pain Troponin Stress-ECG Probability CAD (%) Atypical Negative Negative 2 Non anginal Negative Positive 4 Atypical Negative Equivocal 5 Typical Negative Negative 15 Atypical Negative Positive 16 Typical Negative Equivocal 32 Non anginal Positive Negative 35 Disability adjusted life expectancies (LE) used in the model Chest pain Troponin Stress-ECG Probability CAD (%) Non anginal Positive Equivocal 58 Typical angina Negative Positive 61 Atypical angina Positive Negative 74 45 Male 45 Age Gender Normal LE LE for diagnosed CAD (years) Reduction of DALE due to missed CAD (years) Reduction of LE due to false positive (years) 33.5 22 1.04 0.27 Female 37.8 24 1.17 0.30 65 Male 16.3 11 0.51 0.13 65 Female 19.8 13 0.61 0.16 (years) Non angina Positive Positive 83 Atypical angina Positive Equivocal 88 Typical angina Positive Negative 96 Atypical angina Positive Positive 96 Typical angina Positive Equivocal 98 Disability-adjusted life expectancies and years of life lost (YLL) based on randomised trials. Typical angina Positive Positive 99 Mukherjee D et al., Am Heart J 2002; The PRISM-PLUS Study Investigators. N Engl J Med 1998; Anderson HV et al. J Am Coll Cardiol 1995 Excess mortality from imaging Meta analysis: ROC 64-slice CT for detection of CAD Age Gender YLL due to ICA YLL due to CCTA 45 Male 0.0387 0.0069 45 Female 0.0452 0.0108 65 Male 0.0192 0.0084 65 Female 0.0232 0.0045 Influence diagram to compute optimal policy Range of clinical probability of CAD where CTCA is optimal as a function of gender and age End point DALE is optimised as a function of - age Age - gender and - probability of CAD after clinical evaluation Yielding - the optimal imaging policy - way of handling uncertain scans and - diagnosis for each of these patient groups YLL = years of life lost DALE = disability-adjusted life expectancy Gender Lower bound (%) Uncertain negative below (%) Upper bound (%) 45 Male 2 6 50 45 Female 2 6 50 65 Male 2 6 55 65 Female 2 6 50 Conclusion 1 Conclusion 2 • A preliminary study on the efficacy of CCTA for the most important clinical CTCA indications has been performed for males and females for the ages of 45 and 65. • The model is based on meta-analysis results of CCTA, average radiation dose and radiation risks. • Outcomes in years of life lost (YLL) and disabilityadjusted life expectancy (DALE) were estimated. • The study integrates cancer risk attributable to CCTA in a medical decision making model Thank you for your attention … Ying Lie O Alex Meijer Job Kievit Jaap Sont Albert de Roos Lucia Kroft Safety and Efficacy in Computed Tomography: a broad perspective EC-EURATOM 6 Framework Programme call 2003 Project no. FP6/002388. 2005 – 2007. • The current practice of the use of 40- and 64-slice CT coronary angiography in suspected CAD seems to be justified in patients with a low to intermediate probability (i.e. 2-50% probability for CAD) after clinical evaluation. • Age and gender have little effect on the range of clinical probability where CTCA is optimal *) • For very low probabilities (i.e. below 6% probability for CAD), it seems most effective to assume non-diagnostic scans as negative results. *) Note: age and gender have a major impact on clinical probability