PROTON THERAPY IN CLINICAL PRACTICE: PAST, PRESENT AND FUTURE Michael Goitein
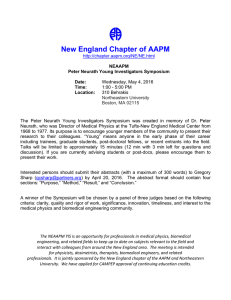
advertisement

PROTON THERAPY IN CLINICAL PRACTICE: PAST, PRESENT AND FUTURE Michael Goitein Harvard Medical School & Ankerstrasse 1, Windisch 5210 Switzerland AAPM Symposium, Baltimore, May 2009 Michael Goitein, AAPM Symposium, Baltimore, May 2009 1 Synopsis 1. Physics interactions of p protons with matter treatment planning 2. Technology beam generation generation, shaping and delivery patient handling integration 3 Radiobiology 3. RBE modelling and treatment strategy 4 Clinical Application 4. clinical experience clinical trials Michael Goitein, AAPM Symposium, Baltimore, May 2009 2 INTERACTIONS OF PROTONS WITH MATTER 69 MeV proton penetration ICRU (1993). (1993) S Stopping i P Powers and d Ranges for Protons and Alpha Particles, ICRU Report 49 multiple Coulomb scattering Gottschalk et al. ((1993)) Multiple p Coulomb scattering of 160 MeV protons. Nucl Instr Methods Phys Res B74:467–490. andd http://huhepl.harvard.edu htt //h h l h d d /~gottschalk/ When primary energy 231 changed MeV graph courtesy of Bernie Gottschalk ~ 2% of range, R range, R Based on a figure courtesy of Eros Pedroni, PSI nuclear interactions there is a vast literature Michael Goitein, AAPM Symposium, Baltimore, May 2009 3 DOSIMETRY • See ICRU report number 78 basically adopts IAEA’s prior protocol (TRS 398) (thus eliminating a 2% discrepancy) proton dosimetry is based on X-ray calibration off ion chambers, with correction factors f however, the largest correction factor is in the w-value of protons in the ion chamber gas, and d thi this value l llargely l relies li on C Calorimetric l i t i determinations • Stated standard error of from 2.0% to 2.3% • Most important point: Proton dosimetry is now standardized and the standard is (or will soon be) near-universally followed Michael Goitein, AAPM Symposium, Baltimore, May 2009 4 INHOMOGENEITIES and Michael Goitein, AAPM Symposium, Baltimore, May 2009 5 INFINITE SLAB Figure based on data of Eros Pedroni X-rays X rays dose protons range change intensity change interface effects are minor (few %) – Koehler (unpublished) depth Michael Goitein, AAPM Symposium, Baltimore, May 2009 6 SEMI-INFINITE SLAB (thin edge) plastic air Med Phys 5:265 (1978) scanning diode overlying l i material Goitein et al., Med Phys 5: 265 (1978) Michael Goitein, AAPM Symposium, Baltimore, May 2009 7 Q. How wide a sliver can cause range g shortening? g 2mm wide Teflon “sliver” angular l ffeathering th i Goitein & Sisterson Radiat Res Radiat. Res. 1978; 74:217 A: pretty small (~ 1mm) - at the edge of available imaging and computation resolution! Michael Goitein, AAPM Symposium, Baltimore, May 2009 8 DISTAL EDGE DEGRADATION Human skull pristine (water-filled) Bragg Peak detector in water, no skull water tank in water, no skull spread-out Bragg Peak Urie et al. Phys Med Biol 1986; 31: 1 Michael Goitein, AAPM Symposium, Baltimore, May 2009 9 lateral beam passing through inhomogeneities distal dose degradation position C; SOBP “ k up”” beam “make b to “fill in” the distal dose deficit Dose (%) 100 90 80 50 20 0 0 5 10 15 Depth (cm) Michael Goitein, AAPM Symposium, Baltimore, May 2009 10 PROTON CONSUMER’S REPORT SCHEMA past present d done / to t do d future currentt status t t almost nothing as good as it gets very little mostly understood some quite a lot l glass half full really a lot some work to be done, but not very critical pretty ignorant i Michael Goitein, AAPM Symposium, Baltimore, May 2009 11 INTERACTION OF PROTONS - SUMMARY past present future proton t penetration t ti multiple Coulomb scattering nuclear interactions dosimetry inhomogeneities awareness Michael Goitein, AAPM Symposium, Baltimore, May 2009 12 TREATMENT PLANNING • image-based geometric design • dosimetric design (manual) • uncertainty • intensity-modulated proton therapy (IMPT) • algorithmic l ith i plan l design d i - optimization and robustness Michael Goitein, AAPM Symposium, Baltimore, May 2009 13 WHAT IS DIFERENT ABOUT TREATMENT PLANNING FOR PROTON THERAPY? adapted from Radiation Oncology: A physicist physicist’ss-eye eye view view. Michael Goitein. Springer, New York, 2007 see also: ICRU report 78 Michael Goitein, AAPM Symposium, Baltimore, May 2009 14 GEOMETRIC DESIGN – image based Beam’s-eye view aperture p drawingg virtual simulation McShan et al. BJR 1979 use off CT sagittal / coronal reconstructions contour definition f image registration ( lti (multi-modality d lit imaging i i – “hat & head” technique Chen, Kessler, Pelizzari…) DRRs reference for setup film Michael Goitein, AAPM Symposium, Baltimore, May 2009 15 DOSIMETRIC DESIGN • algorithms broad beam - radiological path length pencill b beam e.g. Hong et al. A pencil beam algorithm for proton dose calculation. Phys Med Biol 41:1305–1330 Monte Carlo e g GEANT, e.g. GEANT purpose-written code 50 90 color wash (with scale!) side-by-side display dose-difference displays DVHs score functions 30 70 • dose display • plan assessment and comparison 0 10 110 130 X-rays protons Shipley et al. Proton radiation as boost therapy for Michael Goitein, AAPM Symposium, Baltimore, May 2009 localized prostatic carcinoma. JAMA 1979; 241:1912 16 UNCERTAINTY • Virtually all aspects of treatment planning are subject g (mainly ( y systematic) y ) uncertainties,, such as: to significant definition of gross tumor, CTV, and normal anatomy patient and organ localization and movement dose estimation (Goitein. Calculation of the uncertainty in treatment delivery the dose delivered in radiation therapy. Med Phys. Phys 1985; 12:608-612) 12:608 612) etc. t etc. t • It is the job of the plan designer(s) to: assess the h uncertainties i i (at ( a given i level l l off confidence) fid ) take steps to minimize them to the extent practically possible p plan the treatment taking the residual uncertainties into account Michael Goitein, AAPM Symposium, Baltimore, May 2009 17 COMPENSATION FOR MIS-REGISTRATION idealized compensation but, mis-registration can lead to undershoot: solution, (if one gives priority to tumor coverage): solution “open up” the compensator (at the price of certain overshoot) Michael Goitein, AAPM Symposium, Baltimore, May 2009 18 COMPENSATION FOR MULTIPLE SCATTERING At 15cm depth, ≃ 3mm ~ 2% of range, R range, R Based on a figure courtesy of Eros Pedroni, PSI unwanted undershoot Michael Goitein, AAPM Symposium, Baltimore, May 2009 19 COMPENSATION FOR MULTIPLE SCATTERING At 15cm depth, ≃ 3mm ~ 2% of range, R so, expand compensator range, R Based on a figure courtesy of Eros Pedroni, PSI Michael Goitein, AAPM Symposium, Baltimore, May 2009 20 COMPENSATOR DESIGN (physical and virtual) compensates for mis-registration and multiple scattering Urie M et al. (1984) Compensating for heterogeneities in proton radiation therapy. Phys Med Biol 29:553–566 Michael Goitein, AAPM Symposium, Baltimore, May 2009 21 COMPENSATING FOR REGISTRATION ERROR – simple p inhomogeneity g y simple (nominal) bolus “expanded” bolus correct alignment 3 mm misaligned Urie M et al. (1984) Compensating for heterogeneities in proton radiation therapy. Phys Med Biol 29:553–566 Michael Goitein, AAPM Symposium, Baltimore, May 2009 22 COMPENSATING FOR REGISTRATION ERROR – complex p inhomogeneities g simple (nominal) bolus correct alignment “expanded” (by 3mm) bolus 3 mm misaligned Urie M et al. (1984) Compensating for heterogeneities in proton radiation therapy. Phys Med Biol 29:553–566 Michael Goitein, AAPM Symposium, Baltimore, May 2009 23 BEAM DIRECTION NEAR-TANGENT TO A SKIN:TISSUE INTERFACE • The greatest inhomogeneity is that which exists at the interface between the patient and the surrounding air • iff the h beam b direction d is near-tangent to a skin:tissue k interface, the dose distribution can be very sensitive to patient motion or misalignment translation rotation Michael Goitein, AAPM Symposium, Baltimore, May 2009 24 CALCULATION & DISPLAY OF UNCERTAINTY • Compute 3 dose distributions nominal dose at a pixel computed using nominal values of all variables lower bound dose at a pixel computed using the value of each variable that would tend to yield the lowest dose (but use the computed “upper bound” value, if lower) upper bound b d dose at a pixel computed using the value of each variable that would tend to yield the highest dose (but use the computed “lower bound” value, if higher) Michael Goitein, AAPM Symposium, Baltimore, May 2009 25 A MAJOR CONSEQUENCE OF UNCERTAINTY • larger-than-desired safety margins Michael Goitein, AAPM Symposium, Baltimore, May 2009 26 GEOMETRIC DESIGN, DOSE CALCULATION & UNCERTAINTY • image-based geometric design past present future use of imaging image g registration g time variations (4D) • dosimetric design (manual) broad- & pencil-beams Monte Carlo • uncertainty computation, and allowance for the uncertainties Michael Goitein, AAPM Symposium, Baltimore, May 2009 27 TREATMENT PLANNING • image-based geometric design • dosimetric design (manual) • uncertainty • intensity-modulated proton therapy (IMPT) • algorithmic l ith i plan l design d i - optimization and robustness Michael Goitein, AAPM Symposium, Baltimore, May 2009 28 OPTIMIZATION • Why is the subject of optimization important? 1. In IMPT, which presently requires pencil-beam scanning, there are so many variables that one needs a computer algorithm to set them perhaps 10,000 pencil beams or more, times the 3 variables of intensity, depth of penetration and transverse size for each pencil beam 2 Even in uniform 2. uniform-beam beam irradiation, irradiation the choice of penetration (which can vary over the field, is difficult and can benefit from computer-based solutions (e.g. field-patching) • Optimization requires a search algorithm to find the optimal set of variables, and a score function. Generally: a solution to the search problem is not hard to find, though it may be computationally demanding a clinically li i ll meaningful i f l score function f ti iis extremely t l diffi difficult lt to t fi find d • In proton therapy, however due to the almost two orders of magnitude more variables, the search problem becomes even more demanding the score function is further complicated due to uncertainties in the penetration of each pencil beam Michael Goitein, AAPM Symposium, Baltimore, May 2009 29 ROBUST OPTIMIZATION • One simply has to deal with uncertainties. • A robust plan is one which is not too negatively affected b th by the unavoidable id bl or iirreducible d ibl uncertainties. t i ti • There are two ways of achieving robustness: find the p plan which has the least-bad “worst case” the worst case is the (unphysical) dose distribution for which, for a given level of uncertainty in the treatment variables A Lomax, PSI in each voxel within the PTV the dose is set to the lowest possible dose; and see, also: Shalev et al. Treatment in each voxel within an OAR the dose is planning using images of regret. M dD Med Dosim. i 1988 1988;13(2):57-61. 13(2) 57 61 set to the highest possible dose. 0 find the plan which on average has the best score – when averaging over all sources of uncertainty Unkelbach J and Oelfke U Phys. Med. Biol. 49 (2004) 4005–29 these approaches have demonstrated very Unkelbach et al. Accounting for range uncertainties... promising results Phys. Med. Biol. 52 (2007) 2755–2773 Michael Goitein, AAPM Symposium, Baltimore, May 2009 30 IMPT, OPTIMIZATION AND ROBUSTNESS • IMPT past present future understanding d t di off th the problem bl development of solutions • OPTIMIZATION search h techniques h i dose-based optimization biological optimization • ROBUST PLANNING Michael Goitein, AAPM Symposium, Baltimore, May 2009 31 Synopsis 1. Physics interactions of p protons with matter treatment planning 2. Technology beam generation generation, shaping and delivery patient handling integration 3 Radiobiology 3. RBE modelling and treatment strategy 4 Clinical Application 4. clinical experience clinical trials Michael Goitein, AAPM Symposium, Baltimore, May 2009 32 GENERAL STATUS OF THE TECHNOLGY OF PROTON THERAPY • There is a misapprehension that, since proton therapy has been developed over about half a century, the technology is mature. • It is not. g y because: • This is largely the early experience was in research environments in which less-than-efficient procedures were tolerated the current commercial offerings g largely g y copied p the existing g technologies (with the addition of gantries) IMPT is a very recently-recognized possibility and has not had time to be satisfactorily commercially developed • But, don’t be too alarmed, because: proton therapy is currently being delivered with the existing technology to the benefit of large numbers of patients the developments are needed to allow protons to reach their full potential, and to be used in a clinically streamlined fashion. Michael Goitein, AAPM Symposium, Baltimore, May 2009 33 BEAM GENERATION • The technology of currently-used proton accelerators is prett pretty well ell de developed eloped synchrotrons cyclotrons both are adequate and reasonably reliable – except that: • There is still an intensity problem - reflected in: low beam intensity at low energies (cyclotrons) too large pencil beam sizes (caused also by other factors) • Cost remains a factor (we’re still waiting for true marketplace competition 15 years after MGH signed the first commercial contract for a proton facility) Michael Goitein, AAPM Symposium, Baltimore, May 2009 34 NEW TECHNOLOGIES FOR PROTON GENERATION • Good luck • but, beware! remember b th the fate f t off d-T d T generators t iin neutron therapy • and, and don don’tt compromise performance – e.g. eg lowering the maximum energy failure to support IMPT etc. etc Michael Goitein, AAPM Symposium, Baltimore, May 2009 35 BEAM SHAPING: SCATTERED BEAMS • The technology has been very fully developed primarily by Andy Koehler, Bernie Gottschalk, and colleagues at the Harvard Cyclotron Laboratory • Current commercial systems y p primarily y use the “historic” technology, including double-scattering - with a few enhancements, e.g. automatically y selectable range g modulator wheels beam gating to vary the depth of the SOBP • The depth characteristics are fairly satisfactory, using the currentt range modulator d l t ttechnology h l except for low energies for which the Bragg peaks are too narrow to stack easily and a better method of spreading them (e.g. (e g ridge filters) is needed Michael Goitein, AAPM Symposium, Baltimore, May 2009 36 BEAM SHAPING: SCATTERED BEAM PENUMBRA • But, beam penumbra in the current scattered beam implementations is very inadequate (worse than Cobalt-60 Cobalt 60 in many cases) • For scattered beams, the historically achieved penumbrae were OK due to their long throw, but in the current gantry implementations the penumbra is far from satisfactory. satisfactory This is because they use double-scattering with ith a relati relatively el short throw (SAD) range modulator first scatterer compensator full dose region second scatterer protons large effective source size (a few cm) scattered d bbeam technology h l patient compensated range modulator aperture tumor (i.e. target volume) Michael Goitein, AAPM Symposium, Baltimore, May 2009 37 BEAM SHAPING: SCANNED BEAMS and intensity-modulated y proton therapy p py ((IMPT)) • IMPT requires the use of a pencil beam of protons whose Bragg peak is scanned throughout the target volume while its energy (penetration) and intensity are varied at will. gantry “nozzle” can rotate t t around patient control system scanning magnets Michael Goitein, AAPM Symposium, Baltimore, May 2009 38 BEAM SHAPING: SCANNED BEAMS and intensity-modulated y proton therapy p py ((IMPT)) • IMPT requires the use of a pencil beam of protons whose Bragg peak is scanned throughout the target volume while its energy (penetration) ( t ti ) and d iintensity t it are varied. i d • The only significant experience with IMPT to date has been at the Paul Scherrer Institute (PSI) in Switzerland where they developed, and have used since 1996, a prototype so-called spot-scanning gantry • PSI are now building a second gantry featuring isocentric rotation and faster scanning (due to start treating in 2010) • Commercial scanning systems are just now in their infancy. IMPT technology Michael Goitein, AAPM Symposium, Baltimore, May 2009 39 BEAM SHAPING: SCANNED BEAM PENUMBRA • In scanned beams, the beam penumbra is set by the diameter of the pencil beam near the end of range. • This has two components: scattering in the patient about which technology can do nothing pencil beam size in the absence of the patient which is entirely due to the technology • If one wants to at least match, at a depth of 10cm, typical linac penumbrae of about 7mm (80-20%), the pencil beam size at isocenter in the absence of the patient (i.e. due to the technology) needs to be no more than about: ≈ 3.5 mm – i.e. a fwhm of no more than ≈ 8 mm • Current implementations fall short of this important goal. goal Michael Goitein, AAPM Symposium, Baltimore, May 2009 40 INTERPLAY EFFECT • The main downside of beam scanning is that, if there is motion of the patient and/or the tumor, so-called interplay effects ff t can lead l d to t up-and-down d d d dose variations i ti within ithi th the ttargett (dose mottle). Phillips M et al. Effects of respiratory motion on dose uniformity with a charged particle scanning method. Phys Med Biol. 1992 Jan;37(1):223-34 Bortfeld T et al. Effects of intra–fraction motion on IMRT dose delivery… Phys Med Biol 47:2203–2220. scan scan cell ll cell has received ~5 times intended dose scan cell ll Dose mottle is not just theoretical It has been theoretical. observed at about the 14% (SD) level in an animal experiment y at PSI,, caused merely by ~2mm movements of the mouse intestine irradiated in a scanned 10 mm pencil beam! cell has received ~0 times intended dose Gueulette G l et al. l IJROBP 2005;62:838-845 Michael Goitein, AAPM Symposium, Baltimore, May 2009 41 CURRENT SOLUTION(S) TO THE INTERPLAY PROBLEM • First, reduce the amount of motion to the extent possible • Then, static respiratory gating abdominal compression tumor tracking repaint the field many times. But… 1 scan 2 scans 3 scans 5 scans 10 scans Grözinger et al. Simulations to design an online motion compensation system for scanned particle beams Phys. Phys Med. Med Biol. Biol 51 (2006) 3517 3517–3531 3531 and thesis: http://elib.tu-darmstadt.de/diss/000407/ Michael Goitein, AAPM Symposium, Baltimore, May 2009 42 BEAM SHAPING • In depth scattered beams scanned beams • Laterally ll ((penumbra) b ) scattered beams scanned beams 30 Michael Goitein, AAPM Symposium, Baltimore, May 2009 43 IMMOBILIZATION AND MOTION MANAGEMENT • Proton therapy has, from its very beginning, emphasized accuracy of beam placement (relative to the target volume) and tight margins where possible and indicated. • This is for two reasons: compensators need to be in accurate registration with the inhomogeneities and beam shapes they are intended to compensate for in order to avoid an unintended distribution of dose a main goal of proton therapy is to minimize the volume of normal tissue outside the target volume which receives a high dose • This has resulted in a number of developments which have found wide application Michael Goitein, AAPM Symposium, Baltimore, May 2009 44 PLANNING, IMMOBILIZATION AND LOCALIZATION patient #1 at HCL (1974) patient #2 at HCL (1974) planning based on smearing tomography planning based on radiographs alignment on radiographs Michael Goitein, AAPMbased Symposium, Baltimore, May 2009 45 IMMOBILIZATION AND LOCALIZATION (contd.) Verhey et al. Precise positioning of patients for radiation therapy. Int J Radiat Oncol Biol Phys. 1982; 8:289-294 Michael Goitein, AAPM Symposium, Baltimore, May 2009 46 GATING & TARGET TRACKING (intra- & inter- fraction) respiratory gating (NIRS, Japan) implanted gold seeds rectal probe & waterfilled balloon Shipley et al. Proton radiation as boost therapy for localized prostatic carcinoma. JAMA 1979; 241:1912 Minohara et al. Respiratory gated irradiation system for heavy-ion radiotherapy. Int J Radiat Oncol Biol Phys 47(4):1097–1103;2000 PSI high-mag. h h image of anterior eye with the position of the pupil being outlined. ocular tumor tracking though real time video tracking of anterior eye position (HCL, PSI) picture courtesy J Vervey, PSI Michael Goitein, AAPM Symposium, Baltimore, May 2009 47 PATIENT SUPPORT ASSEMBLY HCL 6-degree of freedom patient supporter (Wagner) Commercial i l 6 degree d of freedom patient couch (IBA) Orsay-Curie O C i 6 degree of freedom patient couch (Mazal) The additional degrees of freedom are required to adjust for small rotational misalignments of the patient. Michael Goitein, AAPM Symposium, Baltimore, May 2009 48 THROUGHPUT • Currently it generally takes too long, and is too hard, to set up and treat a patient. this is hard on the patient this is hard on the staff tends to reduce accuracy it can degrade quality, and it reduces throughput and hence increases costs • One partial solution is to perform the patient setup outside the treatment room and bring him or her into the treatment room when i b it becomes available il bl without, ih iin principle, the need for further localization, à la PSI. • But, this does not get at the root of the problem which is: inadequate systems engineering – and inadequate specification of the needs Michael Goitein, AAPM Symposium, Baltimore, May 2009 49 INTEGRATION • Integration and Workflow are concepts which are more talked about than put into practice. Michael Goitein, AAPM Symposium, Baltimore, May 2009 50 PATIENT HANDLING AND INTEGRATION • patient handling immobilization and motion management patient support assembly throughput • integration workflow 40 Michael Goitein, AAPM Symposium, Baltimore, May 2009 51 Synopsis 1. Physics interactions of p protons with matter treatment planning 2. Technology beam generation generation, shaping and delivery patient handling integration 3 Radiobiology 3. RBE modelling and treatment strategy 4 Clinical Application 4. clinical experience clinical trials Michael Goitein, AAPM Symposium, Baltimore, May 2009 52 RBE = 1.10 isn’t all that bad... 1.22 2 1.10 Paganetti et al. IJORB 53: 407 (2002) 2 Michael Goitein, AAPM Symposium, Baltimore, May 2009 53 DOSE 100% bio-effective dose physical dose DEPTH Michael Goitein, AAPM Symposium, Baltimore, May 2009 54 But, proton RBE needs (some) refinement RBE 1.0 1 3 DOSE 2 100% bio-effective dose physical dose 4 RBE 1.10 in center of SOBP RBE in entrance region a bit less (? 5%) than at SOBP center? 6 7 RBE rises across SOBP ?? order of 1% / cm “blip” near end of SOBP ? 5 - 10% 5 elongation g of range ~ 1-2 mm. RBE depends on dose per fraction RBE depends on tissue type & endpoint DEPTH Michael Goitein, AAPM Symposium, Baltimore, May 2009 55 MODELLING AND TREATMENT STRATEGY reduced d d tumor dose in the region in which the tumor is close to the brainstem increased brainstem dose accepted in the small region in which it is close to the tumor Michael Goitein, AAPM Symposium, Baltimore, May 2009 56 MODELLING TUMOR CONTROL PROBABILITY (TCP) The development of p y models biophysical suggested that, for example, a partial boost to a tumor may increase the TCP dose minimum dose partial boost 50% volume 80% volume 90% volume 100% volume 35 TCP 30 increase (%) 25 =2 50 20 boost dose 15 10 5 ttargett volume distance Goitein et al. Proceedings of the 19th LH Gray Michael Goitein, Conference (Brit. J. Radiol.). 1997: 25-39 0 0 5 10 15 20 Boost Dose (%) AAPM Symposium, Baltimore, May 2009 57 BUT (as seen in IMRT and with interplay effects)… BEWARE DOSE MOTTLE! dose dose mottle average dose amplitude p target volume distance TCP (actual dose distribution < TCP (average tumor dose) for a dose mottle of ±7.5% TCP ≈ - 4 % for a dose mottle of ±10% TCP ≈ - 6.5 65% Brahme A. Acta Radiol Oncol 23: 379-391 (1984) Michael Goitein, AAPM Symposium, Baltimore, May 2009 58 MODELLING NORMAL TISSUE COMPLICATION PROBABILITY (NTCP) serial structure radiatio on radiattion parallel structure 0.6 0.6 0.5 a = 10 0.5 1.0 NTCP 0.4 a=2 0.4 0.3 0.3 0.9 0.2 0.2 1.0 0.8 0.1 09 0.9 0.1 0.7 0 0.8 0.7 0 0 0.2 0.4 0.6 relative volume 0.8 1 0 0.2 0.4 0.6 0.8 relative volume Modelling supported the idea that organs could tolerate a higher dose if it was only delivered to part of the organ. Michael Goitein, AAPM Symposium, Baltimore, May 2009 59 RADIOBIOLOGY: dose-volume effects • There are many important but unanswered questions • Some of the unsolved issues are: the answers to which are relevant for all radiations, but particularly to particles with which one is attempting to spare normal tissues particularly effectively “bath-or-shower dilemma” (is it better to deliver a lower dose to a larger volume of normal tissue, or a higher dose to a smaller volume?) vs. how does functional damage to an organ or tissue depend on the relative (or absolute) volume irradiated to high dose? how does functional damage to an organ or tissue depend on the (lower) dose delivered to the rest of the volume? how does the radiation damage of an organ or tissue depend on the radiation experience of nearby tissues and organs? • We need to resurrect whole-organ and whole-organism radiobiology • When we know the answers to some of these questions, we will need new biophysical models so we can use computers to optimize treatments dose, d, to a relative volume, v lower dose, d’, to rest of volume dose, d’’, to surrounding volume Michael Goitein, AAPM Symposium, Baltimore, May 2009 60 RBE, MODELLING AND TREATMENT STRATEGY • RBE • Radiation response of tissues data modelling treatment strategies Michael Goitein, AAPM Symposium, Baltimore, May 2009 61 Synopsis 1. Physics interactions of p protons with matter treatment planning 2. Technology beam generation generation, shaping and delivery patient handling integration 3 Radiobiology 3. RBE modelling and treatment strategy 4 Clinical Application 4. clinical experience clinical trials Michael Goitein, AAPM Symposium, Baltimore, May 2009 62 CLINICAL EXPERIENCE • Some 61,000 patients have been treated with proton beam therapy as of Feb Feb. 2009 2009. • The largest single group is comprised of ~17,000 patients with ocular melanomas. p http://ptcog.web.psi.ch/patient_statistics.html • There have been only a limited number of clinical trials off proton beam b therapy, h and d only l two randomized d d clinical trials of protons vs. conventional radiotherapy. • The experience to date should perhaps be read as a confirmation that the theoretical arguments for proton beam therapy have been upheld in the limited number off situations in which h h they h have h been b tested. d Goitein & Goitein. Swedish protons. Acta Oncol. 2005;44(8):793-7 Michael Goitein, AAPM Symposium, Baltimore, May 2009 63 Chondrosarcoma - local l l control t l 1 08 0.8 Local Control Choroidal melanoma - local control 0.6 0.4 0.2 0 0 5 10 15 Time (years) 100 Paranasal sinus tumors 33 squamous cell carcinomas, 30 carcinomas with neuroendocrine differentiation 20 adenoid cystic carcinomas 13 soft tissue sarcomas, and 6 adenocarcinomas. The median dose was 71.6 CGE. Percent (%) 80 60 40 local control Local control 20 regional control Regional control Freedom from distant metastasis freedom from distant metastases 0 0 1 Michael Goitein, AAPM 2 3 4 5 Follow-UpBaltimore, Time (years) Symposium, 6 7 May 2009 8 64 THE RATIONALE FOR JUDGING THE CLINICAL SUPERIORITY OF PROTONS VIS-À-VIS VIS À VIS X-RAYS X RAYS For the same dose to the target volume, protons deliver a l lower physical h i l dose d to the h uninvolved i l d normall tissues i than h do high-energy X-rays. There is very y little difference in tissue response p p per unit dose between protons of therapeutic energies as compared with high-energy X-rays, so that the only relevant ee a td differences e e ces a are ep physical. ys ca There is no medical reason to irradiate any tissue judged not to contain malignant cells. Radiation damages normal tissues and the severity of that damage increases with increasing dose. Suit H, et al. Should positive phase III clinical trial data be required before proton beam therapy is more widely adopted? No. No Radiother Oncol. Oncol 2008;86:148153 Each of these 4 statements is established experimentally beyond reasonable doubt Michael Goitein, AAPM Symposium, Baltimore, May 2009 65 RANDOMIZED CLINICAL TRIALS • There are two fundamental principles which govern whether a randomized clinical trial (RCT) is ethically appropriate: The arms of the study must be in equipoise. That is to say, the arms must be judged to be substantially equivalent from a patient’s patient s point of view view. When a doctor agrees to take care of a patient, he or she is entering into an unwritten contract with the patient to use his or her best efforts and judgment on behalf of that patient. There can be no unspoken reservation that societal interests may take priority over those of the patient, and the patient may expect to be fully informed regarding any facts that he or she might deem relevant. These principles principles, together with the previous 4 statements, statements mean that many otherwise desirable RCTs can not be performed for ethical reasons - equipoise can not truthfully be said to obtain for them. Michael Goitein, AAPM Symposium, Baltimore, May 2009 66 CLINICAL TRIALS (contd.) • It is a great pity that almost no case-controlled clinical l l studies d h have b been planned l d or performed. f d • It would seem that, in the absence of an ability in many cases to conduct randomized clinical trials, carefully designed prospective casecontrolled comparisons between proton centers and institutions lacking a proton capacity would be desirable. • clinical trials randomized case-controlled t ll d Michael Goitein, AAPM Symposium, Baltimore, May 2009 67 RECENT TEXTS • Gottschalk B (2004) “Passive Beam Spreading in Proton Radiation Therap ” http://huhepl.harvard.edu/~gottschalk/ Therapy” http //h hepl har ard ed / gottschalk/ File named “pbs.pdf” can be extracted from BGdocs.zip See, also, PowerPoint lectures in BGtalks.zip • ICRU report 78 “Prescribing, Recording and Reporting Proton Beam Therapy” Oxford U. Press. Journal of the ICRU 7(2); 2007 • T.F. Delaney and H.M. Kooy (eds) “Proton and Charged Particle Radiotherapy” Lippincott Williams Radiotherapy and Wilkins, 2007 • M. Goitein “Radiation Oncology: A Physicist’s-Eye View” Springer, 2007 Michael Goitein, AAPM Symposium, Baltimore, May 2009 68 TECHNOLOGY SUMMARY changes with time current sources of protons broad- & pencilbeam algorithms future sources of protons Monte Carlo dose calculation scattered beam technology RBE value(s) scanned beam technology & IMPT tissue response: data IMPT: understanding scattered beam: depth characteristics tissue response: models IMPT: solutions scanned beam: depth characteristics treatment strategies based on biology optimization: search techniques scattered beam: lateral penumbra optimization: dose-based scanned beam: lateral penumbra use of imaging optimization: biology-based immobilization & motion management image registration robust optimization patient support systems INTERACTIONS OF PROTONS proton penetration Coulomb scattering nuclear interactions dosimetry inhomog-eneities TREATMENT PLANNING throughput, g & integration workflow RADIOBIOLOGY uncertainties: calcn. and allowance for CLINICAL TRIALS randomized protons vs. X-rays case-controlled protons vs. X-rays Michael Goitein, AAPM Symposium, Baltimore, May 2009 69 CONCLUSIONS • Much has been done. • Much remains to be done. • It is important that what has been learned in the p past be incorporated p into the clinical work of the future - and not simply regarded as being of purely historical interest and hardly worth learning about. about Michael Goitein, AAPM Symposium, Baltimore, May 2009 70 finis Michael Goitein, AAPM Symposium, Baltimore, May 2009 71