Antiretroviral drug resistance in pregnant national HIV surveillance databases
advertisement

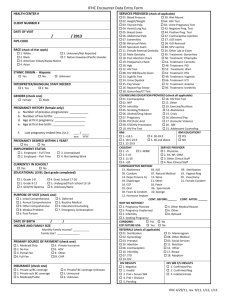
Antiretroviral drug resistance in pregnant women living with HIV in England & Wales: preliminary results from the matching of three national HIV surveillance databases Laura Byrne, Cuong Chau, Valerie Delpech, David Dunn, Pat Tookey, Anna Tostevin & Claire Thorne UCL Institute of Child Health Background Background • Drug resistance testing for all newly diagnosed patients recommended since 2005 and now for virtually all pregnant women prior to treatment • Genetic diversity has increased in the UK, the majority of heterosexual women have non-B subtype • Overall, TDR peaked in the UK in 2002, has fallen and now stabilised at 8-9% in recent years • Non-B subtypes associated with lower prevalence of TDR • The prevalence of TDR in pregnant women has not been estimated before in the UK Aims 1. Ascertain the proportion of women reported to the NSHPC who can be matched to ≥1 resistance test in UKDRD and factors associated with being matched 2. Describe the distribution of HIV-1 viral subtype in pregnant women 3. Describe the prevalence of TDR in women diagnosed during pregnancy who are naive to ART Methods LINKAGE BETWEEN THREE NATIONAL HIV SURVEILLANCE DATABASES National Study of HIV in Pregnancy & Childhood (NSHPC) collects data on pregnancies in all HIV-positive women and their infants Survey of Prevalent HIV infections Diagnosed (SOPHID) part of Public Health England’s HIV AIDS Reporting System (HARS) • Clinical and risk factor information on all adults seen for HIV care in NHS sites in England, Wales and Northern Ireland UK HIV Drug Resistance Database (UKHDRD) held at MRC CTU at UCL • Collects the majority of resistance tests performed as part of routine clinical care in the UK Methods DATA LINKAGE Hierarchical matching algorithm: combinations of identifiers • SOPHID to UKHDRD – • – e.g. patient number, site of care, soundex, region, date of birth SOPHID to NSHPC e.g. sex, date of birth, partial postcode, country of birth and date of HIV diagnosis 80% of resistance tests matched to a SOPHID record Nearly 90% of women in NSHPC matched to a SOPHID record Methods SUBTYPE & RESISTANCE TESTS HIV viral subtype determined using the REGA HIV-1 subtyping tool v3.0 TDR: presence of ≥1 mutations from the WHO 2009 surveillance list POPULATION HIV+ women with ≤ 1 reported pregnancy due to deliver or delivering 2000-2013 reported by Sep 2014 in England & Wales STATISTICAL ANALYSES Fisher’s exact / chi square for comparison of proportions Logistic regression models for factors assoc. with matched resistance test Results POPULATION CHARACTERISTICS 10, 115 women diagnosed before delivery with delivery date (or EDD) 20002013, reported by Sep 2014 14,416 pregnancies Median age at conception 30 years (IQR 26 to 34) 78.0% Black African, 1.3% likely infected through IDU Median year HIV diagnosis 2004 (range 1982 to 2013) 49.9% women matched to at ≥1 resistance test 58.2% matched if year of diagnosis > 2005 63.5% of women with a RT classified as naïve on the 1st test Results FACTORS ASSOCIATED WITH ≥1 MATCHED RESISTANCE TEST Multivariable analysis aOR 95% CI 1 pregnancy reported 1.0 - 2 pregnancies reported 1.65 1.49 - 1.83 ≥3 pregnancies reported 1.98 1.70 – 2.31 Woman diagnosed with HIV 2010-2013 1.0 Woman diagnosed with HIV 1985-1995 0.75 0.56 – 0.99 Woman diagnosed with HIV 1996-2000 0.56 0.45 – 0.69 Woman diagnosed with HIV 2001-2005 0.63 0.53 – 0.75 Woman diagnosed with HIV 2006-2009 0.94 0.80 – 1.11 Results FACTORS ASSOCIATED WITH ≥1 MATCHED RESISTANCE TEST Multivariable analysis aOR 95% CI Woman’s ethnicity – Black African 1.0 - Woman’s ethnicity - White 0.95 0.72 – 1.26 Woman’s ethnicity - other 1.1 0.85 – 1.44 Woman born in UK/Ireland 1.0 - Woman born in rest of Europe 0.83 0.64 – 1.07 Woman born in Africa 0.75 0.66 – 0.86 Woman born elsewhere 0.80 0.65 – 0.98 Results FACTORS ASSOCIATED WITH ≥1 MATCHED RESISTANCE TEST Multivariable analysis aOR 95% CI First pregnancy reported from London 1.0 - First pregnancy reported from rest of England 0.66 0.61 – 0.72 Year of first pregnancy reported 2009-2013 1.0 - Year of first pregnancy reported 2000-2003 0.55 0.47 – 0.63 Year of first pregnancy reported 2004-2008 0.88 0.79 – 0.98 Results VIRAL SUBTYPE Woman’s region of birth (n=4929) HIV-1 subtype C UK / Ireland (654) Europe (193) Africa (3,761) Elsewhere (321) TOTAL 32.9% 13.5% 52.9% 20.3% 46.6% CRF02_AG 8.1% 7.2% 14.5% 5.3% 13.1% A 6.8% 16.6% 11.6% 3.4% 10.6% B 37.3% 33.2% 1.1% 46.1% 10.1% Other recombinant forms 7.8% 10.9% 7.1% 21.5% 8.3% G 3.7% 10.9% 5.6% 2.2% 5.3% D 2.8% 1.0% 4.5% 1.3% 4.1% Other pure 0.5% 5.7% 1.3% 0% 0.7% Unclassified / complex 0.2% 1.0% 0.8% 0% 0.7% p<0.01 Results TDR IN WOMEN DIAGNOSED DURING PREGNANCY1 Woman’s year of diagnosis (n=1302) TDR by drug class 20002003 20042005 20062007 20082009 20102011 20122013 Total P value2 Any resistance 3.4% 7.3% 2.4% 5.2% 5.4% 10.1% 5.2% <0.01 Any NRTI resistance 1.1% 2.6% 0.8% 2.1% 2.0% 4.5% 1.9% 0.18 Any NNRTI resistance 1.1% 3.9% 1.3% 1.7% 4.4% 6.3% 2.8% 0.02 Any PI resistance 1.1% 1.7% 0.8% 1.7% 0.5% 1.8% 1.2% 0.65 Number of women with a RT 88 234 375 291 203 111 1302 1 Woman diagnosed during the index pregnancy, classified as “ART naïve” on resistance test request, with resistance test date within pregnancy. 2 Fisher’s exact test between years (test-for-trend not significant). Conclusions • 50% women in the NSHPC have been matched to ≥1 resistance test in the UKDRD • Factors assoc. with being matched: – – – – – • ≥1 pregnancy reported diagnosed after 2005 born in UK/Ireland or Europe vs. Africa or elsewhere First pregnancy reported from London vs. rest of England First pregnancy reported in later time period Matching between SOPHID & NSHPC is reliant on partial postcode, therefore more mobile populations may be less well matched Conclusions • Nearly 50% subtype C infection, only 10% subtype B, underlining viral diversity in HIV+ people in the UK and the association with risk type and region of birth • Overall prevalence of 5.2% in pregnant women in keeping with previous estimates of TDR in heterosexual popn in the UK • Most common TDR drug class was NNRTIs followed by NRTIs, and prevalence of TDR to PIs was very low • Numbers of women diagnosed during pregnancy have steadily dropped since a peak in 2004-2007. However, suggestion that the prevalence of TDR in pregnant women may have increased in the most recent time period Acknowledgments NSHPC Ethics MREC/04/2/009 NSHPC Current funding Public Health England The National Screening Committee Additional funding LB currently holds MRC Clinical Research Training Fellowship NSHPC Current team Principal investigator: Pat Tookey Data manager & statistician: Helen Peters Researchers: Kate Francis, Angela Jackson, Laura Byrne Administrative assistant: Icina Shakes Additional support: Claire Thorne, Catherine Peckham, Mario Cortina-Borja www.ucl.ac.uk/nshpc Acknowledgements Shema Tariq & Clare French, former PhD students at NSHPC who helped set-up the matching between SOPHID & NSHPC with Cuong Chau and colleagues at PHE