Medical Assistance Bulletin Recommends Monthly Screening of Employees and Contractors
advertisement

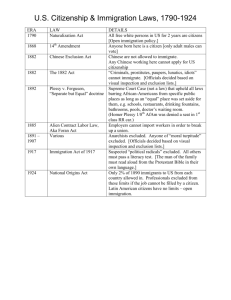
September 21, 2011 Practice Group: Health Care Medical Assistance Bulletin Recommends Monthly Screening of Employees and Contractors On August 15, 2011, the Pennsylvania Department of Public Welfare (“DPW”), Office of Medical Assistance Programs (“OMAP”) issued Medical Assistance Bulletin (“MAB”) 99-11-05, applicable to all Medical Assistance providers. The MAB reminds providers of the necessity of screening employees and contractors for exclusion from participation in Federal health care programs1 in order to avoid billing for services provided directly or indirectly through excluded persons.2 The prohibition on payment for services provided directly or indirectly by individuals or entities who have been excluded from a Federal health care program has been in place for more than a decade. From 1999-2001, OMAP issued monthly updates to its Medicheck list, which identified individuals and entities who were terminated or precluded from participation in the Medical Assistance Program. Then at the beginning of 2002, OMAP made the list available via the Internet. Other than the monthly issuance of the Medicheck list, this is the first MAB dedicated to the issue of compliance with the prohibition on payment for services provided directly or indirectly by excluded persons. This may signal an intent to step up enforcement on this issue, or may indicate that OMAP has identified recent problems with this area of compliance. The MAB sets forth steps for administration of the screening requirement: 1. Develop written policies and procedures to implement background checks for excluded individuals and entities. Medical Assistance providers who operate a compliance program should already have a policy and procedure to ensure that services billed to Medical Assistance (or any Federal health care program, including Medicare and all state Medicaid programs) are not provided through excluded persons. The policy needs to be realistic in light of the provider’s operations because after the policy is established, the government will expect it to be followed. The provider is expected to educate employees about the policy and adhere to it, even if the policy requires more than is legally required. For that reason, providers should tailor the policy to their circumstances, considering size of the operation, resources, and level of risk. For example, a provider who relies heavily on part-time staff and independent contractors could have a higher risk of improper billing than a provider who employs primarily full-time staff who have no other commitments because the provider should 1 “Federal health care program” means any “plan or program that provides health benefits, whether directly, through insurance, or otherwise, which is funded directly, in whole or in part, by the United States Government (other than the [federal employee] health insurance program under Chapter 89 of title 5, United States Code…); or any State health care program.” 42 U.S.C. §1320a-7b(f). These programs include Medicare, Medicaid, a State Children’s Health Insurance Program, Tricare, Maternal and Child Health block grant programs and Social Services block grant programs. 2 Federal law provides that payment may not be made “with respect to any amount expended for an item or service … furnished—(A) under the [State Medicaid Plan] by any individual or entity during any period when the individual or entity is excluded [from a Federal health care program], [or] (B) at the medical direction or on the prescription of a physician, during the period when such physician is excluded from participation [from a Federal health care program] and when the person furnishing such item or service knew or had reason to know of the exclusion (after a reasonable time period and after reasonable notice has been furnished to the person).” 42 U.S.C. §1396b(i)(2). Medical Assistance Bulletin Recommends Monthly Screening of Employees and Contractors have better information on full-time employees and more control regarding their work activities. Likewise, a provider with more frequent turnover may be at higher risk than a provider with a stable workforce. Providers should require employees to provide notice of an exclusion, or an investigation that could lead to exclusion, as a condition of employment through an employee code of conduct form or employment contract. With respect to entities under contract to the provider, providers should include a clause in the contract to require the entity to inform the provider of an exclusion or pending investigation or other action that could lead to exclusion of the entity or any employee or sub-contractor of the entity. 2. Use all three databases that are available for screening of excluded individuals or entities. The United States Department of Health and Human Services, Office of Inspector General (“OIG”) maintains the federal health care program exclusions database, which can be found at the link on the homepage of the OIG: http://www.oig.hhs.gov/. The second federal database, maintained by the General Services Administration, is broader than federal health care programs. It identifies individuals and entities that are debarred or suspended from obtaining federal contracts and certain subcontracts or subawards and are excluded from participating in certain federal financial assistance programs or activities. The link to this database is at https://www.epls.gov/. The third database is DPW’s Medicheck list, found at: http://www.dpw.state.pa.us/learnaboutdpw/fraudandabuse/medicheckprecludedproviderslist/index. htm. The Medicheck list includes all individuals and entities precluded from Pennsylvania’s Medical Assistance program by any means, including OMAP termination of the agreement. Providers should be aware that it is not only medical professionals and care providers that need to be screened under these databases. The prohibition against use of Medical Assistance funds to pay for services rendered or ordered by excluded individuals or entities extends to a prohibition against use of such funds to pay the salaries for management or administrative personnel. For providers who submit cost reports, the inclusion of any wages, salaries or other payment in the cost report to develop the rates paid to that provider would automatically make those individuals receiving such wages, salaries or payments subject to the screening process. 3. Regularly check the federal and state databases. In OMAP’s view, providers should visit the databases frequently, not just at the time of hire or initial contracting. OMAP proposes screening “on an ongoing monthly basis.” Monthly screening is not required by law. However, providers are liable if they “knew or should have known” of the individual’s or entity’s excluded status. It is likely that OMAP will hold providers to this monthly standard since it is in the MAB, and OMAP takes the position that providers are required to comply with these bulletins through their provider agreements. Providers are held to a “knew or had reason to know” standard with respect to these exclusions. OMAP also could argue that providers who check at less frequent intervals or only at initiation of the contract or employment still “had reason to know” of the exclusion sooner by checking the database more frequently. 4. Audit and document compliance with the established policy. OMAP suggests periodic audits of exclusion screening practices to ensure that regular review of the databases is occurring and that claims are not submitted for services of excluded individuals or entities. As with anything related to government compliance, every step of the process should be documented, including initial and ongoing reviews of the databases; education of employees on the screening process; communications with independent contractors, suppliers, medical staff and other doctors ordering services for patients about the screening policy and obligations to report exclusions; and the actual compliance audits, findings and follow-up. 2 Medical Assistance Bulletin Recommends Monthly Screening of Employees and Contractors 5. Report any discovered exclusion of an employee, contractor or ordering physician to DPW’s Bureau of Program Integrity. As soon as it is discovered that an employee, independent contractor, supplier or ordering physician is excluded, an immediate internal review of the impact of the exclusion should be performed to determine what, if any, liability may be connected to the exclusion. The following questions should be asked, at a minimum: · How long has the individual or entity been excluded? · Has the provider billed for any services provided by the excluded individual or entity, or provided based on the order or prescription of an excluded physician? If so what is the extent of the billing? · Has the provider provided un-billed services through an excluded individual or entity or on an order from an excluded physician? If any services were billed that relate to the excluded individual or entity, a report will need to be made to the DPW’s Bureau of Program Integrity.3 The provider should also attempt to determine how the exclusion escaped the regular database review. DPW suggests making the report immediately through its online MA Provider Compliance Hotline Response Form, by mail or by fax. While overpayments need to be reported, it is prudent to consult legal counsel and take a measured assessment of the extent of the noncompliance, based on the advice and guidance of counsel, before reporting to DPW. For example, if it is determined that an excluded individual was not identified because there was a break in adherence to screening policies and procedures for a period of time, the provider should discuss with counsel whether an expanded compliance review should occur. DPW’s issuance of a detailed MAB on this issue likely means that this is a problem compliance area from OMAP’s perspective. The intensified federal and state efforts to recover improperly billed funds, and to prevent improper billing at the outset, may also have served as an impetus for this MAB. Regardless, providers should evaluate their current policies and practices on exclusion screening in light of the recommendations of the MAB. The MAB may be found by entering the number 99-11-05 at this link: http://services.dpw.state.pa.us/olddpw/bulletinsearch.aspx. Author: Ruth E. Granfors ruth.granfors@klgates.com +1.717.231.5835 3 Self-reporting of billing errors has always been encouraged, but the Fraud Enforcement and Recovery Act of 2009 and the Patient Protection and Affordable Care Act, Pub. Law 111-148, require reporting and repayment of any overpayment within 60 days of discovering the overpayment. See prior K&L Gates alert: Liability for Failure to Disclose and Return “Identified” Overpayments, May 2010. 3 Medical Assistance Bulletin Recommends Monthly Screening of Employees and Contractors 4