Document 13519230
advertisement
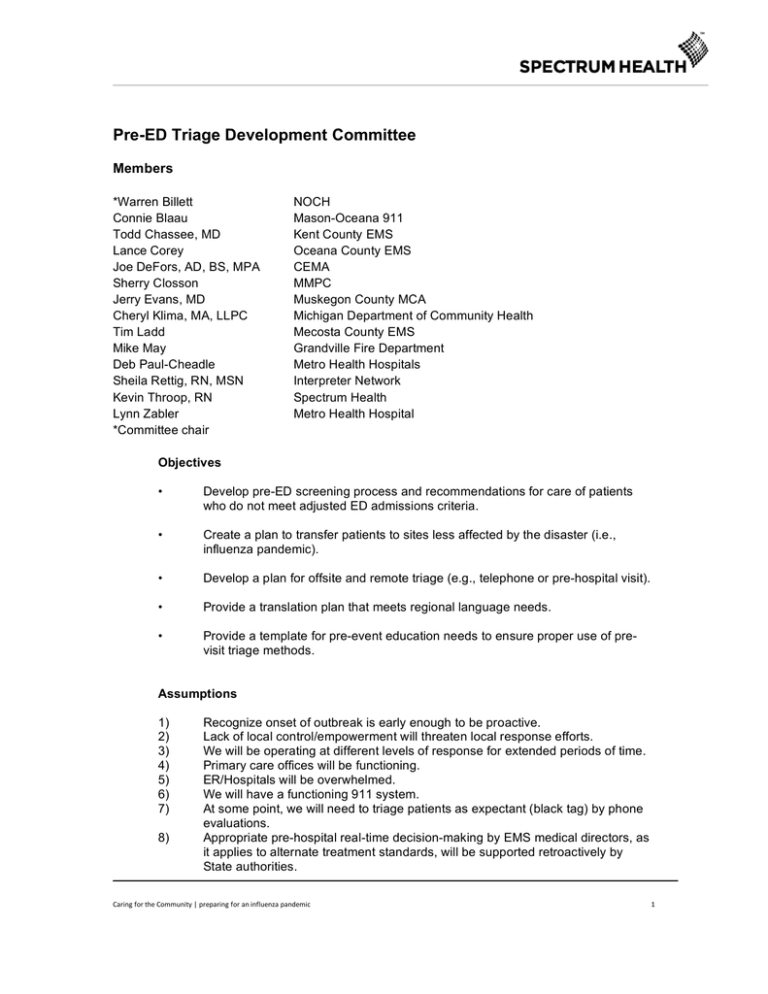
Pre-ED Triage Development Committee Members *Warren Billett Connie Blaau Todd Chassee, MD Lance Corey Joe DeFors, AD, BS, MPA Sherry Closson Jerry Evans, MD Cheryl Klima, MA, LLPC Tim Ladd Mike May Deb Paul-Cheadle Sheila Rettig, RN, MSN Kevin Throop, RN Lynn Zabler *Committee chair NOCH Mason-Oceana 911 Kent County EMS Oceana County EMS CEMA MMPC Muskegon County MCA Michigan Department of Community Health Mecosta County EMS Grandville Fire Department Metro Health Hospitals Interpreter Network Spectrum Health Metro Health Hospital Objectives • Develop pre-ED screening process and recommendations for care of patients who do not meet adjusted ED admissions criteria. • Create a plan to transfer patients to sites less affected by the disaster (i.e., influenza pandemic). • Develop a plan for offsite and remote triage (e.g., telephone or pre-hospital visit). • Provide a translation plan that meets regional language needs. • Provide a template for pre-event education needs to ensure proper use of previsit triage methods. Assumptions 1) 2) 3) 4) 5) 6) 7) 8) Recognize onset of outbreak is early enough to be proactive. Lack of local control/empowerment will threaten local response efforts. We will be operating at different levels of response for extended periods of time. Primary care offices will be functioning. ER/Hospitals will be overwhelmed. We will have a functioning 911 system. At some point, we will need to triage patients as expectant (black tag) by phone evaluations. Appropriate pre-hospital real-time decision-making by EMS medical directors, as it applies to alternate treatment standards, will be supported retroactively by State authorities. Caring for the Community | preparing for an influenza pandemic 1 Background The task of this committee was to develop guidelines that will direct the “medical community’s” response during times of pandemic outbreak. The term “medical community” was interpreted in the broadest sense possible to include any provider or clinic or source of medical information in the community. The goal is to provide information and care in the community setting to minimize the demand on the First Response, Emergency Medical Services (EMS) and hospital systems. This can be accomplished through early education of the public as to what they can expect from a health care system that is going to be taxed by an overwhelming number of patients requiring unavailable human assets, equipment and space. Health care providers all want to believe that, given the opportunity, all patients would receive the best possible care. In the beginning, the committee struggled with the fact that not all patients in a pandemic would receive optimal care. The committee agreed that guidelines must be developed to help identify those individuals that will benefit the most from the limited assets. More directly stated, in the time of a pandemic it will be necessary to make decisions that will ultimately determine who may live or die. The following were members of the committee: Sherry Closson MMPC Connie Blaauw – 12-year veteran Dispatcher for Mason-Oceana 911. Previous experience includes seven years managing a residential Alternative Immediate Service facility for clients with mental and physical disabilities. Warren Billett EMT-P/IC – Manager EMS Department of North Ottawa Community Health System; Chair, Region 6 Bio-Defense Network Coalition. Dr. Todd Chassee – Medical Director Kent County EMS, Assistant Professor in the Emergency Medicine Program Michigan State College of Human Medicine, Emergency Physician Spectrum Health Butterworth Hospital. Lance Corey Oceana County EMS Joe DeFors, AD, BS, MPA – Co-founder and principal officer of Comprehensive Emergency Management Associates, a full service emergency planning, training and exercise firm. Joe works in a variety of capacities on projects and holds the position of corporate finance officer. Joe is retired from the Lansing Fire Department where he was a Firefighter/Paramedic. Dr. Jerry Evans Muskegon County MCA Cheryl A. Klima, MA, – Bioterrorism Coordinator, MDCH-EMS and Trauma Systems Section, experience in disaster mental health and emergency preparedness. Tim Ladd – Director of Mecosta County Emergency Medical Service. Tim has a Bachelor Degree in Health Care Administration and has been a paramedic since 1991. Michael May – Lieutenant, Grandville Fire Department, Grandville, MI. Mike has 28 years of EMS experience and is currently responsible for managing Grandville’s EMS program. He is also involved in local planning and sits on the governing board of the Kent County Medical Control Authority. Caring for the Community | preparing for an influenza pandemic 2 Sheila Rettig, RN, MSN – President/CEO Interpreter Network, LLC, Master’s-prepared nurse entrepreneur experienced in cultural community issues. Interpreter Network is a service that unites language and culture in health care, legal, business and education arenas. Kevin Throop – Supervisor of Emergency services at Spectrum Health's Butterworth campus. Lynn Zabler, RN, FCN, RN – Twenty years experience as Trauma Nurse Specialist, ED Supervisor, and House Supervisor, 12 years experience in Outpatient nursing, Oncology, and Day Surgery. Has worked extensively in a management capacity. Most recently working in Employee Health/Safety/ Disaster Preparedness. Certifications include: Trauma Nurse Specialist, PALS, ACLS, Pediatric Trauma Nurse Specialist, Faith Community Nurse, RISEN, Oncology, and multiple other certifications throughout the years. Process Utilizing the above assumptions, it became apparent that there would need to be a graduated response depending on the situation in any given region. Many sources were reviewed and information assessed. Although several models were found, many of them lacked clinical guidelines for making these critical decisions and none of them addressed the increase of stress on the healthcare system at the community level. Based on work done by Dr. Mark Hall, a matrix was developed with five levels of response. Guidelines were written for dispatch centers, pre-hospital providers (first responders and EMS) and transporting agencies for both flu-like illnesses and non-flu-like illnesses. The ethics and legal committees were consulted when making the decisions on this matrix. Education of the public and providers is essential to minimize the stress on the medical care system. This must be kept as simple and objective as possible. Education must be done prior to onset of significant spread of influenza. Medical equipment and personnel will need to be rationed based on the local situation and availability. Resources must be used to benefit the most people to provide the greatest number of positive outcomes. Objectives Report This committee developed a pre-ED triage and treatment matrix to be utilized by pre-hospital personnel for determining disposition of patients in a pandemic situation. This matrix utilizes standards of care during a pandemic that reduces the stress on hospitals and EMS systems in an overwhelming medical crisis. The triage and treatment matrix can be utilized at any pre-hospital triage site to include Neighborhood Emergency Help Centers, physician offices, nursing homes, medi-centers, ambulatory care sites, dispatch centers, etc. The committee worked with Interpreter Network to develop internet-based educational videos in multiple languages. The committee strongly encourages further development of educational videos. The committee developed a template for education on the triage and treatment matrix (Figure 1). Caring for the Community | preparing for an influenza pandemic 3 Figure 1 This matrix takes into account the progression of the pandemic in relationship to the impact that it is having on the local medical community and allows the local medical community the flexibility to adapt to the needs of the system. In Figure 2, Level A through Level E represents the impact the outbreak may have on the local medical community. At Level A, the local community would begin awareness education for the medical community as well as for the public. This would begin an awareness that should this pandemic reach the local area, changes in the way medical services are delivered may/will change. However, at this level, there has not been an increase of patients in the medical system and therefore there would be no change in how healthcare is delivered. The education for the public would include media and internet-based video messages targeted to specific groups (ethnicities). More on the actual communications will be covered later in this report. Caring for the Community | preparing for an influenza pandemic 4 Figure 2 Caring for the Community | preparing for an influenza pandemic 5 For each level detailed in Figure 2, in Figure 3 shows changes in the expected response from different parts of the system (Dispatch, Treatment or Transport) as we move from Level A to Level E. Figure 3 Caring for the Community | preparing for an influenza pandemic 6 Then, within each of the three areas, we took into account that not only will the medical community need to address the patients afflicted with the pandemic illness, we will need to continue caring for the patients that we would routinely be seeing as well. In Figure 4 we accommodate patients with non-flu-like complaints. Figure 4 Caring for the Community | preparing for an influenza pandemic 7 In Figure 5 we are looking at the transition from Level A and Level B. This turning point triggers awareness, signaling that it’s time to begin looking at each agency’s response planning, staffing, and asset/resource availability. Because there is no increase in patient care there are no changes in the response. Figure 5 Caring for the Community | preparing for an influenza pandemic 8 In Figure 6, we now have seen a significant increase in the numbers of patients and we need to begin to limit the response of the medical system in order to provide the greatest amount of care for the largest number of patients. Figure 6 Caring for the Community | preparing for an influenza pandemic 9 Figure 7 Caring for the Community | preparing for an influenza pandemic 10 In the Dispatch area we are no longer responding to priority 3 calls. Figure 8 Caring for the Community | preparing for an influenza pandemic 11 Figure 9 Caring for the Community | preparing for an influenza pandemic 12 Figure 10 Caring for the Community | preparing for an influenza pandemic 13 Figure 11 Caring for the Community | preparing for an influenza pandemic 14 Figure 12 Caring for the Community | preparing for an influenza pandemic 15 Figure 13 Caring for the Community | preparing for an influenza pandemic 16 TRANSLATION PLAN OBJECTIVE Provide a translation plan that meets regional language needs. Provide a template for pre-event education to ensure proper use of pre-visit triage methods. There are three essential components to providing effective communication to Limited English Proficient (LEP) population and cultural groups. 1) ACCESS – How will LEP populations access information? 2) ACKNOWLEDGEMENT – How will LEP populations understand a clear and correct message? 3) ACCEPTANCE – What factors can influence levels of acceptance of a state plan, to support implementation and success? It is important to understand communication trends in LEP cultural groups. The results of an informal study among several cultural groups in West Michigan revealed that there are two categories to study. 1) Communication patterns with a high frequency use are: a. Messages from school age children and family b. Neighbors c. Community meeting places d. Community leaders/Spiritual leaders PROBLEM: Information many times is incorrect or at least flawed. 2) Communication patterns with a low frequency use are: a. TV b. Newspaper c. Radio d. Written notices PROBLEM: Commonly used standard media sources are primarily communicated in English and do not address emergency messaging for multiple languages. Low literacy levels limit effectiveness, even when messages are provided in native languages. SUGGESTED SOLUTIONS 1) Create a universal symbol for ALL people to become familiar with and recognize alternate care sites or information. Caring for the Community | preparing for an influenza pandemic 17 2) Create access to information via video conferencing/internet sources for multiple languages and for Deaf and Hard of Hearing. 3) Identify potential champions within various cultural groups to support state recommendations. 4) Education preparedness for pre-triage situations. Caring for the Community | preparing for an influenza pandemic 18