Humira
advertisement
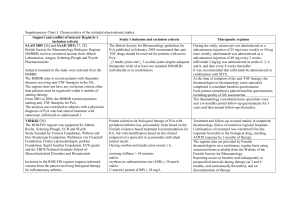
Humira® Active ingredient: Adalimumab Marketing authorisation holder: Abbott Laboratories Ltd Availability: National Health Service and Private Sector Variations: Sarcoidosis was added to the undesirable effects list. A cumulative review of this adverse event was carried out from the MAH clinical trial database (from 27 April 2010). In clinical trials, 5 patients reported 6 events of sarcoidosis. One patient was following treatment with adalimumab in a randomised controlled trial but no reports were received from the comparator group. 4 of these cases were considered as serious. Only 1 event was deemed possibly related to adalimumab. A cumulative review of such adverse event and related terms was carried out from the MAH post marketing safety databases (from 15 April 2010). This summed to 151 reports of possible sarcoidosis; out of which 129 were medically confirmed. From the medically confirmed cases: - 87 were not accepted as they reported erythema nodosum, pulmonary granuloma or granuloma without a specific diagnosis or evidence of sarcoidosis, - 3 events were not related to adalimumab, - 2 events were received from blinded clinical trial where the patient did not receive adalimumab or the study remained blinded, - 24 reports described at least 1serious event and 13 described as non-serious events. From the latter reports describing both non-serious and serious events, 22 had no apparent confounding factors or alternative aetiologies whilst 8 had potential confounding factors such as evidence of prior sarcoidosis which reappeared or worsened with adalimumab therapy. Due to the difficulty in confirming the diagnosis of sarcoidosis and the fact that aetiology is not known, the causal relationship of sarcoidosis with the administration of adalimumab is hard to confirm. In view of the medically confirmed events without confounding factors or alternative aetiologies and evidence that TNF-α is involved in sarcoidosis, it is not possible to reject this causal relationship. It is classified as a rare adverse effect (0.02 events per 100 patient years). This is based on the occurrence of sarcoidosis from clinical studies as it represents the most conservative approach. Data from a multi-centre open-label study which investigated long term (at least an additional 108 weeks) safety and efficacy of adalimumab treatment in moderate to severe chronic plaque psoriasis. These participants had completed Phase 2 and 3 of the preceding clinical trials. Two hundred and thirty-three patients who achieved Psoriasis Area and Severity Index (PASI) 75 at week 16 and week 33 were administered continuous adalimumab therapy for 52 weeks in Psoriasis Study I (REVEAL) and in the open-label extension trial. After an additional 108 weeks of open-label therapy (total of 160 weeks): - PASI 75 and Physician Global Assessment (PGA) of clear or minimal response rates in these patients were 74.7% and 59% respectively. - PASI 75 and PGA of clear or minimal response rates were 69.6% and 55.7% in analysis of nonresponder patients. These patients have dropped out of the study for adverse effects or lack of efficacy or whose dose-escalated. Overall, 347 stable responders took part in a withdrawal and retreatment evaluation in the open label extension study. During the withdrawal period, patients re-experienced symptoms of psoriasis over time with a median-time to relapse (decline to PGA “moderate” or “worse”) of approximately 5 months. However none of these patients experienced rebound during withdrawal period. 76.5% (218/285) of patients who were enrolled in the retreatment period had a response of PFA “clear” or “minimal” after 16 weeks of retreatment. It is irrespective of whether they relapsed during the withdrawal period. A comparable safety profile was noted during retreatment as prior to withdrawal. The occurrence of immunogenicity was low (approximately 2%). There was no correlation with occurrence of undesirable events and presence of antibodies. Minimal decrease in efficacy was observed in association with the presence of antibodies. In withdrawal and retreatment study, the rate of antibodies to adalimumab after retreatment (11 of 482 subjects, 2.3%) was comparable to the rate observed prior to withdrawal (11 of 590 subjects, 1.9%). Patients who participated in this study were undergoing long term monotherapy treatment with adalimumab. Section 4.8 of the SmPC was also updated with the malignancies rates observed in clinical trials. The indication of adalimumab 40mg/0.8ml solution for injection for paediatric use was extended to include treatment of active polyarticular juvenile idiopathic arthritis (JIA) in paediatric subjects from 4 to 12 years. The recommended dosage regimen is 24mg/m2 body surface area to a maximum single dose of 40mg administered every other week via subcutaneous injection. The volume for injection is based on the patient’s weight and height. The pharmacodynamic and pharmacokinetic sections of the SmPC were updated with data obtained from the clinical trial in JIA patients. A multicentre, randomised double blind parallel group clinical trial was carried out to evaluate the safety and efficacy of adalimumab in paediatrics suffering from polyarticular juvenile idiopathic arthritis (171 participants aged 4 -17 years old). In the open-label lead in phase, the participants were assigned either in methotrexate (MTX) treated or nonMTX treated. Patients assigned to the latter group were either naïve to or had been withdrawn from methotrexate at least 2 weeks prior to study drug administration. These participants remained on stable doses of NSAIDs and/or prednisone (<0.2mg/kg/day or 10mg/day maximum). All patients received 24mg/m2 up to a maximum of 40mg adalimumab every other week for a duration of 16 weeks. In the double blind phase, participants were eligible if at week 16 they had a Paediatric ACR 30 response. These were administered either adalimumab 24mg/m2 up to a maximum of 40mg or placebo every other week for an additional 32 weeks or until disease flare. These patients were then enrolled into the open label extension phase. Amongst those who responded at week 16 (144), the Paediatric ACR 30/50/70/90 responses were maintained for up to 6 years in the OLE phase in patients who received adalimumab throughout the study. 19 subjects were treated for 6 years or longer. Overall responses were generally better. Fewer patients developed antibodies when treated with the combination of adalimumab and methotrexate compared to Humira® alone. Taking these results into consideration, Humira® is recommended for use in combination with MTX and for use as monotherapy in patients for whom MTX use is not appropriate. Reference: European Medicines Agency. Humira. [online]. 2011May 19 [cited 2011 Sep 8]; Available from: URL: http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/000481/human_med_000822.jsp&murl=menus/medicine s/medicines.jsp&mid=WC0b01ac058001d124