Factors Affecting Penetration of Ciprofloxacin in Lower Extremity Clinical and Translational Research 623707
advertisement
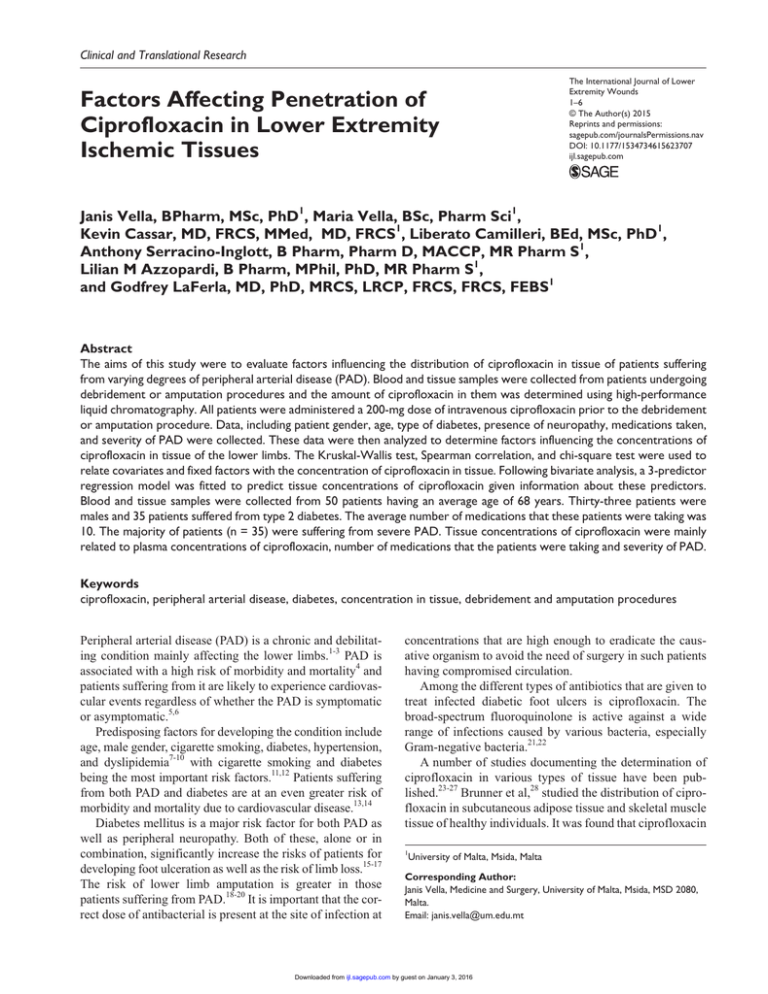
623707 research-article2015 IJLXXX10.1177/1534734615623707The International Journal of Lower Extremity WoundsVella et al. Clinical and Translational Research Factors Affecting Penetration of Ciprofloxacin in Lower Extremity Ischemic Tissues The International Journal of Lower Extremity Wounds 1­–6 © The Author(s) 2015 Reprints and permissions: sagepub.com/journalsPermissions.nav DOI: 10.1177/1534734615623707 ijl.sagepub.com Janis Vella, BPharm, MSc, PhD1, Maria Vella, BSc, Pharm Sci1, Kevin Cassar, MD, FRCS, MMed, MD, FRCS1, Liberato Camilleri, BEd, MSc, PhD1, Anthony Serracino-Inglott, B Pharm, Pharm D, MACCP, MR Pharm S1, Lilian M Azzopardi, B Pharm, MPhil, PhD, MR Pharm S1, and Godfrey LaFerla, MD, PhD, MRCS, LRCP, FRCS, FRCS, FEBS1 Abstract The aims of this study were to evaluate factors influencing the distribution of ciprofloxacin in tissue of patients suffering from varying degrees of peripheral arterial disease (PAD). Blood and tissue samples were collected from patients undergoing debridement or amputation procedures and the amount of ciprofloxacin in them was determined using high-performance liquid chromatography. All patients were administered a 200-mg dose of intravenous ciprofloxacin prior to the debridement or amputation procedure. Data, including patient gender, age, type of diabetes, presence of neuropathy, medications taken, and severity of PAD were collected. These data were then analyzed to determine factors influencing the concentrations of ciprofloxacin in tissue of the lower limbs. The Kruskal-Wallis test, Spearman correlation, and chi-square test were used to relate covariates and fixed factors with the concentration of ciprofloxacin in tissue. Following bivariate analysis, a 3-predictor regression model was fitted to predict tissue concentrations of ciprofloxacin given information about these predictors. Blood and tissue samples were collected from 50 patients having an average age of 68 years. Thirty-three patients were males and 35 patients suffered from type 2 diabetes. The average number of medications that these patients were taking was 10. The majority of patients (n = 35) were suffering from severe PAD. Tissue concentrations of ciprofloxacin were mainly related to plasma concentrations of ciprofloxacin, number of medications that the patients were taking and severity of PAD. Keywords ciprofloxacin, peripheral arterial disease, diabetes, concentration in tissue, debridement and amputation procedures Peripheral arterial disease (PAD) is a chronic and debilitating condition mainly affecting the lower limbs.1-3 PAD is associated with a high risk of morbidity and mortality4 and patients suffering from it are likely to experience cardiovascular events regardless of whether the PAD is symptomatic or asymptomatic.5,6 Predisposing factors for developing the condition include age, male gender, cigarette smoking, diabetes, hypertension, and dyslipidemia7-10 with cigarette smoking and diabetes being the most important risk factors.11,12 Patients suffering from both PAD and diabetes are at an even greater risk of morbidity and mortality due to cardiovascular disease.13,14 Diabetes mellitus is a major risk factor for both PAD as well as peripheral neuropathy. Both of these, alone or in combination, significantly increase the risks of patients for developing foot ulceration as well as the risk of limb loss.15-17 The risk of lower limb amputation is greater in those patients suffering from PAD.18-20 It is important that the correct dose of antibacterial is present at the site of infection at concentrations that are high enough to eradicate the causative organism to avoid the need of surgery in such patients having compromised circulation. Among the different types of antibiotics that are given to treat infected diabetic foot ulcers is ciprofloxacin. The broad-spectrum fluoroquinolone is active against a wide range of infections caused by various bacteria, especially Gram-negative bacteria.21,22 A number of studies documenting the determination of ciprofloxacin in various types of tissue have been published.23-27 Brunner et al,28 studied the distribution of ciprofloxacin in subcutaneous adipose tissue and skeletal muscle tissue of healthy individuals. It was found that ciprofloxacin 1 University of Malta, Msida, Malta Corresponding Author: Janis Vella, Medicine and Surgery, University of Malta, Msida, MSD 2080, Malta. Email: janis.vella@um.edu.mt Downloaded from ijl.sagepub.com by guest on January 3, 2016 2 The International Journal of Lower Extremity Wounds concentrations attained in the tissue were sub-inhibitory despite adequate concentrations present in blood.28 In another study, the same authors stated that there were differences in the pharmacokinetics at the tissue target site when 2 bioequivalent dosage forms of ciprofloxacin were administered to healthy volunteers.29 Licitra et al30 measured ciprofloxacin concentrations in different tissue, including tissue from the leg and foot. Penetration of ciprofloxacin into the infected tissue was reported to be excellent.30 In another study performed on healthy volunteers, Joukhadar et al31 reported that local warming of the skin resulted in more ciprofloxacin reaching the lower limbs due to increased vasodilation indicating that the drug probably has a greater penetration in tissue that is inflamed than healthy tissue. This is not consistent with findings made by Müller et al32 who studied the penetration of ciprofloxacin in infected diabetic foot ulcers. The authors claimed that there was no significant difference between the concentrations of ciprofloxacin in healthy and inflamed tissue.32 The sample size in these studies, however, was small. Inlight of this it was decided to measure ciprofloxacin concentrations in the tissue of patients with infected foot ulcers who are suffering from varying degrees of PAD where tissue penetration of anti-infective agents might be predicted to be less due to the presence of the condition. There have been similar studies documenting the determination of other anti-infective agents in the tissue of patients suffering from PAD.33,34 However, the distribution of ciprofloxacin in patients suffering from diabetic foot ulcers with varying degrees of PAD is not known and is being investigated in this study. The aims of the study were to determine concentrations of ciprofloxacin in plasma and tissue of patients suffering from varying degrees of PAD. The study also aimed to identify factors influencing the distribution of ciprofloxacin in the tissue. Patients and Methods Degree of Peripheral Arterial Disease The presence or absence and the severity of PAD were assessed in the clinical setting. The ankle brachial pressure index (ABPI) and the spectral waveform at the ankle were recorded. Patients having triphasic waveforms with an ABPI of 0.91 to 1.29 were considered to have no PAD. Those having biphasic waveforms and/or an ABPI of 0.51 to 0.90 were suffering from mild to moderate PAD. Patients suffering from severe PAD were those having monophasic waveforms and an ABPI lying between 0.00 and 0.50. Drug Administration A 200-mg intravenous dose of ciprofloxacin was administered to the patient 30 minutes prior to the surgical intervention via infusion, which lasted about 20 minutes. Blood and Tissue Sampling A blood sample ranging between 3 to 5 mL was taken by the anesthetist present during the debridement or amputation procedure. The sample was collected about 30 minutes after the administration of ciprofloxacin. Blood was collected peripherally from the region of the cubital fossa and stored in a red-top Vaccutainer. Following collection, the blood was allowed to clot, the tube centrifuged and the upper serum level decanted and stored at −20°C until analysis. Tissue samples were taken from the wound by the surgeon carrying out the debridement or amputation procedure. The average amputation or debridement procedure took between 15 to 30 minutes to be complete. Each sample was rinsed with sterile saline solution and stored in sterile plastic containers at −20°C until analysis. Patients Analytical Method Ethics approval was obtained from the University Research and Ethics Committee of the University of Malta. Informed consent was obtained from patients participating in the study. Inclusion criteria included patients undergoing a debridement of a foot ulcer or amputation procedure who were receiving intravenous ciprofloxacin. Exclusion criteria included pregnancy or lactation and those who were younger than 18 years. Patients who did not give any consent to participate in the study as well as those suffering from ascites were excluded from the study. A patient profile form was used to record the patients’ gender, age, weight, type of diabetes, and presence of neuropathy. The smoking status, types of comorbidities, number of medications taken, and creatinine clearance were also recorded on this form. The concentration of ciprofloxacin was determined from each patient sample. Ciprofloxacin concentrations were determined in patient plasma using a previously developed and validated method involving high-performance liquid chromatography (HPLC).35 The concentration of ciprofloxacin in tissue was determined using a developed and validated method, which is similar to that used to determine the antibiotic in plasma. Five hundred milligrams of patient subcutaneous tissue was accurately weighed and homogenized. Protein precipitation was carried out to separate the antibiotic and analysis was carried out on a Varian HPLC unit using the same chromatographic conditions as those used to determine ciprofloxacin in patient plasma. Downloaded from ijl.sagepub.com by guest on January 3, 2016 3 Vella et al. Data Analysis Table 1. Most Common Patient Comorbidities (N = 50). Data about PAD severity, the concentrations of ciprofloxacin in plasma and tissue and that collected from the patient profile form were processed using SPSS statistics 22. Data were analyzed for linear regressions and also for descriptive statistics. The Kruskal-Wallis test, Spearman correlation, and chi-square test were used to correlate covariates and fixed factors with the concentration of ciprofloxacin in tissue. Parameters which could affect the concentration of ciprofloxacin in patient tissue were determined by means of the parsimonious model. The parameters that were considered for the model were age, gender, weight, HbA1c levels, creatinine clearance, number of medications that the patient was taking, smoking status, the type of diabetes that the patient was suffering from, and presence or absence of neuropathy. Other parameters which were considered were the type of wound and severity of PAD. Backward elimination was then carried out to exclude factors which were considered to be insignificant due to the large P value attained and a 3-parameter regression model was developed. From the patient samples included in the study, results from 10 of these patients were randomly selected to test the developed regression model. Data from the most significant 3 predictors were inputted to work out the expected tissue concentration using this model. The calculated value for ciprofloxacin tissue concentration obtained from the regression model was then compared with the already calculated ciprofloxacin tissue concentration (which was previously determined by HPLC). Comorbidity Results Patient Characteristics Blood and tissue samples from a total of 50 patients were used in the study. Thirty-three of these patients were male and 17 female. The patients’ age ranged from 28 to 92 years with a mean age of 68 years. The patients’ weight ranged from 59 to 165 kg with a mean weight of 80 kg. The majority of patients (n = 38) had never smoked. Eight patients were nonsmokers but had smoked in the previous 10 years. Four patients were current smokers. The average number of medications that each patient was taking was 10 (range 1-18 different types of medication per patient). The most common comorbidity that these patients were suffering from was diabetes (n = 49). Table 1 shows the most common comorbidities in this group of patients. Fourteen patients were suffering from type 1 diabetes and 35 patients were suffering from type 2 diabetes. Only 1 patient did not suffer from diabetes. Out of those suffering from diabetes, 3 were on diet alone while 32 were on oral hypoglycemic agents. Twenty-six patients were using insulin while 13 patients were controlling diabetes using both oral hypoglycemic agents and insulin. Diabetes mellitus Hypertension Ischemic heart disease Congestive heart failure Renal impairment Hypercholesterolemia Hyperlipidemia Hypothyroidism Prostatic hyperplasia Cataracts Gout Anxiety and depression No. of Patients Suffering 49 40 29 16 9 7 5 4 3 3 2 2 The average HbA1c level for this population of patients was 8% (range 5% to 14%) and the majority of patients (n = 44) were suffering from neuropathy. In this population of patients, the mean creatinine clearance, which was measured on admission was 68 mL/min (range 10-177 mL/min). Thirty patients had no renal impairment, 13 patients had mild renal impairment, 3 patients had significant renal impairment while 4 patients suffered from severe renal impairment. The majority of patients (n = 39) underwent surgery involving a toe amputation, 5 underwent surgery involving trans-metatarsal amputation, and 6 patients underwent debridement of a foot ulcer. Only 3 patients had nil or borderline PAD. The rest of the patients were suffering from mild to moderate (n = 12) and severe PAD (n = 35). None of the patients in this group were suffering from chronic venous insufficiency. A positive correlation was seen between the presence and severity of PAD and gender (P = .05). One male patient and 2 female patients had nil/borderline PAD. There were more male patients (n = 12) than female patients (n = 1) suffering from mild/moderate PAD and 20 male patients and 14 female patients were suffering from severe PAD. One patient had nil/borderline PAD and did not suffer from diabetes. The largest number of patients (n = 23) suffering from severe PAD had type 2 diabetes. Eleven and 3 patients suffering from type 1 diabetes had severe PAD and mild/moderate PAD, respectively. Concentration of Ciprofloxacin Patient plasma ciprofloxacin concentrations were higher than those present in tissue. The average concentration of ciprofloxacin in plasma was that of 2.14 µg/mL (range 0.008.00 µg/mL) and that in tissue was 0.28 µg/mL (range 0.002.06 µg/mL). Downloaded from ijl.sagepub.com by guest on January 3, 2016 4 The International Journal of Lower Extremity Wounds Table 2. Testing the Regression Model. Patient Code 3. 7. 12. 15. 21. 25. 26. 28. 40. 43. No. of Medications Conc. of Ciprofloxacin in Plasma (µg/mL) 10 13 7 9 9 10 3 7 7 12 2.07 1.78 3.41 1.95 0.99 1.95 1.60 3.96 2.80 0.10 Severity of PAD Conc. of Ciprofloxacin in Tissue Calculated by Model (µg/mL) Conc. of Ciprofloxacin in Tissue Determined by HPLC (µg/mL) Severe Severe Severe Severe Severe Severe Severe Mild/moderate Mild/moderate Mild/moderate 0.12 0.11 0.11 0.12 0.14 0.11 0.18 0.32 0.34 0.34 0.13 0.13 0.11 0.11 0.11 0.11 0.18 0.37 0.35 0.33 Abbreviations: Conc., concentration; HPLC, high-performance liquid chromatography; PAD, peripheral arterial disease. Pharmacokinetic Models Testing the Regression Model The parsimonious model for ciprofloxacin tissue concentration includes 3 predictors: serum ciprofloxacin concentration, number of medications administered to patients, and the severity of PAD. Peripheral arterial disease severity was the best predictor, followed by the number of medications and the concentration in patient plasma. The coefficient for the concentration in plasma (0.0175) indicates that for every 1 unit increase in plasma ciprofloxacin concentration the concentration in tissue is expected to increase by 0.0175 units. The coefficient for the number of medications (−0.0093) indicates that for every 1 unit increase in the number of medications the concentration in tissue is expected to decrease by 0.0093 units. The regression coefficient for nil/borderline PAD (1.3416) indicates that the concentration in tissue for this category is expected to be 1.3416 units higher compared with the group of patients suffering from severe PAD. The coefficient for mild to moderate PAD (0.215) indicates that the concentration of ciprofloxacin in tissue in this category is 0.215 units higher than in the one for severe PAD given that other effects are kept constant. The regression model relating concentration in tissue to PAD severity, plasma ciprofloxacin concentration and number of medications is Table 2 shows that the values calculated by HPLC analysis were comparable to those estimated by the regression model and differences were not significant. The average results for the concentration of ciprofloxacin in tissue calculated by the regression model and by HPLC were 0.125 µg/mL (±0.007), 0.12 µg/mL (±0.014), 0.11 µg/mL (±0.000), 0.115 µg/mL (±0.007), 0.125 µg/mL (±0.021), 0.11 µg/mL (±0.000), 0.18 µg/mL (±0.000), 0.345 µg/mL (±0.035), 0.345 µg/mL (±0.007), and 0.335 µg/mL (±0.007). Expected Ctissue = 0.2366 + 1.3416 ( PAD1 ) + 0.215 ( PAD 2 ) − 0.0093 ( Meds ) + 0.0175Cplasma where Ctissue= tissue concentration (µg/g), PAD1 = 1 for patients with nil/borderline PAD, PAD1 = 0 for patients with mild/moderate or severe PAD, PAD2 = 1 for patients with mild/moderate PAD, PAD2 = 0 for patients with nil/ borderline and severe PAD, Meds = number of medications taken and Cplasma = plasma concentration (µg/g). Discussion The concentration of ciprofloxacin in the subcutaneous tissue of this group of patients is related to the concentration of ciprofloxacin in plasma, the number of medications that the patients are taking and also on the severity of PAD. In a similar study conducted by Zammit et al34 using gentamicin as the anti-infective agent of interest, gentamicin tissue concentrations were found to mostly depend on gender and degree of PAD severity. Ciprofloxacin plasma concentrations were found to be higher in the plasma than in tissue at the time of sampling. These findings agree with those made in previous pharmacokinetic studies where ciprofloxacin plasma concentrations were higher than those in tissue after 30 to 60 minutes from administration.28,29,32 Ciprofloxacin tissue concentrations were found to be lower in patients suffering from more severe forms of PAD. These expected results indicate that poor peripheral perfusion in patients suffering from more severe forms of the disease was probably the reason why ciprofloxacin concentrations were lower at the site of interest. In cases where inadequate concentrations of anti-infective agents are reached in the affected area, dose adjustment would be necessary to help achieve concentrations which are above Downloaded from ijl.sagepub.com by guest on January 3, 2016 5 Vella et al. the minimum inhibitory concentration for most bacteria causing the infection. Patients taking a greater number of medications to treat their comorbidities were found to have lower ciprofloxacin tissue concentrations. It is unlikely that drug interactions due to enzyme metabolism and competitive inhibition affect concentrations of ciprofloxacin present in tissue. Ciprofloxacin itself is mostly excreted unchanged with about 10% to 20% of the administered dose being metabolized.36(p79),37 Ciprofloxacin is an inhibitor of CYP1A2 and therefore affects the metabolism of other drugs being metabolized by that same enzyme.38 A reason that could justify the relationship between tissue concentrations of ciprofloxacin and the number of medications that these patients were taking could be due to comorbidities present. On observing the comorbidities present in this group of patients, it could be noted that the most common ones were diabetes, hypertension, ischemic heart disease, and congestive heart failure. These 4 conditions are often related to vascular rarefaction.39-43 Rarefaction can be a consequence of vascular remodeling and is related to peripheral resistance and to vessel inflammation and damage. This peripheral resistance can stem from vascular dysfunction and this can be with or without structural changes.43 Rarefaction could therefore be a possible reason why tissue concentrations of ciprofloxacin were found to be lower in patients taking a greater number of medications to treat comorbidities. The predicted values of tissue concentrations estimated using the parsimonious regression model were very similar to those obtained using HPLC. This indicates that the model is effective in predicting what concentration of ciprofloxacin is likely to reach the affected tissue. Keeping the factors making part of the regression model in mind, will help predict whether the concentration of ciprofloxacin in tissue lies above the minimum inhibitory concentration for the bacteria causing the infection. The developed model can be effectively applied in a clinical setting to determine the concentration of ciprofloxacin at the site of interest. By knowing the number of medications that the patient is on to treat existing comorbidities, the concentration of ciprofloxacin in the patient’s plasma and the degree of severity of any PAD present, the concentration of ciprofloxacin in the tissue can be determined. This might help the clinician determine how much of the drug is reaching the affected area and if this concentration is enough for successful treatment of the infection. This would enable administration of the appropriate dose of antibiotic to ensure that the tissue thus possibly reducing the need for surgical interventions. Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Funding The author(s) received no financial support for the research, authorship, and/or publication of this article. References 1. Shankar A, Li J, Nieto FJ, Klein BE, Klein R. Association between C-reactive protein level and peripheral arterial disease among US adults without cardiovascular disease, diabetes, or hypertension. Am Heart J. 2007;154:495-501. 2. Aronow WS. Peripheral arterial disease in women. Maturitas. 2009;64:204-211. 3. Aronow WS. Peripheral arterial disease in the elderly. Clin Interv Aging. 2007;2:645-654. 4. Carvounis CP, Nikas N. Prevalence of peripheral arterial disease in subjects at moderate cardiovascular risk: Greek results of the PANDORA study. Hellenic J Cardiol. 2014;55:294-304. 5. Yang XM, Sun K, Zhang WL, Wu HY, Zhang HM, Hui RT. Prevalence and risk factors for peripheral arterial disease with hypertension among Han Chinese. J Vasc Surg. 2007;46:296-302. 6. Sanna G, Alesso D, Mediati M, et al. Prevalence of peripheral arterial disease in subjects with moderate cardiovascular risk: Italian results from the PANDORA study. Data from PANDORA (prevalence of peripheral arterial disease in subjects with moderate CVD risk, with no overt vascular diseases nor diabetes mellitus. BMC Cardiovasc Disord. 2011;11:59. 7. Rabia K, Khoo EM. Peripheral arterial disease in general and diabetic population. Med J Malaysia. 2007;62:182-186. 8. Cho SW, Kim BG, Kim DH, Kim BO, Byun YS, Rhee KJ. Prediction of coronary artery disease in patients with lower extremity peripheral artery disease. Int Heart J. 2015;56:209212. 9. Al-Qaisi M, Nott DM, King DH, Kaddoura S. Ankle brachial pressure index (ABPI): an update for practitioners. Vasc Health Risk Manag. 2009;5:833-841. 10.Valdivielso P, Ariza MJ, de la Vega-Román C, et al. Association of the -250G/A promoter polymorphism of the hepatic lipase gene with the risk of peripheral arterial disease in type 2 diabetic patients. J Diabetes Complications. 2008;22:273-277. 11.Strandness DE, Eidt JF. Peripheral vascular disease. Circulation. 2000;102:46-51. 12. Valdivielso P, Ramírez-Bollero J, Pérez-López C. Peripheral arterial disease, type 2 diabetes and postprandial lipidaemia: is there a link? World J Diabetes. 2014;5:577-585. 13. Jude EB, Elefheriadou I, Tentolouris N. Peripheral arterial disease in diabetes—a review. Diabet Med. 2010;27:4-14. 14. Jude EB, Oyibo S, Chalmers N, Boulton AJ. Peripheral arterial disease in diabetic and nondiabetic patients: a comparison of severity and outcome. Diabetes Care. 2001;24:1433-1437. 15. Bittel DC, Bittel AJ, Tuttle LJ, et al. Adipose tissue content, muscle performance and physical function in obese adults with type 2 diabetes mellitus and peripheral neuropathy. J Diabetes Complications. 2015;29:250-257. 16.Merecz A, Markiewicz L, Sliwinska A, et al. Analysis of oxidative DNA damage and its repair in Polish patients with diabetes mellitus type 2: role in pathogenesis of diabetic neuropathy. Adv Med Sci. 2015;60:220-230. Downloaded from ijl.sagepub.com by guest on January 3, 2016 6 The International Journal of Lower Extremity Wounds 17. Papanas N, Maltezos E. The diabetic foot: a global threat and a huge challenge for Greece. Hippokratia. 2009;13:199-204. 18.Huh JH, Choi EH, Lim JS, Lee MY, Chung CH, Shin JY. Serum cystatin C levels are associated with asymptomatic peripheral arterial disease in type 2 diabetes mellitus without overt neuropathy. Diabetes Res Clin Pract. 2015;108:258-264. 19.Faghihimani E, Darakhshandeh A, Feizi A, Amini M. Evaluation of peripheral arterial disease in prediabetes. Int J Prev Med. 2014;5:1099-1105. 20. Rabia K, Khoo EM. Prevalence of peripheral arterial disease in patients with diabetes mellitus in a primary care setting. Med J Malaysia. 2007;62:130-133. 21. Mostafavi A, Enami J, Varshosaz J, Davies NM, Rezazadeh M. Development of a prolonged-release gastroretentive tablet formulation of ciprofloxacin hydrochloride: pharmacokinetic characterisation in healthy human volunteers. Int J Pharm. 2011;409:128-136. 22. Andersson MI, Mac Gown AP. Development of the quinolones. J Antimicrob Chemother. 2003;51(suppl 1):1-11. 23. Haraguchi S, Hioki M, Yamashita K, et al. Ciprofloxacin penetration into the pulmonary parenchyma in Japanese patients. Surg Today. 2007;37:282-284. 24. Choi J, Mamun MI, Abd El-Aty AM, et al. Inert matrix and Na4EDTA improve the supercritical fluid extraction efficienty of fluroroquinolones for HPLC determination in pig tissues. Talanta. 2009;78:348-357. 25. Granelli K, Elgerud C, Lundström A, Ohlsson A, Sjöberg P. Rapid multi-residue analysis of antibiotics in muscle by liquid-chromatography-tandem mass spectrometry. Anal Chim Acta. 2009;637:87-91. 26. Rao VV, Rambhau D, Ramesh Rao B, Srinivasu P. Circadian variation in urinary excretion of ciprofloxacin after a singledose oral administration at 1000 and 2200 hours in human subjects. Antimicrob Agents Chemother. 1997;41:1802-1804. 27. Bousova K, Senyuva H, Mittendorf K. Quantitative multiresidue method for determination antibiotics in chicken meat using turbulent flow chromatography coupled to liquid chromatography-tandem mass spectrometry. J Chromatogr A. 2013;1274:19-27. 28. Brunner M, Hollenstein U, Delacher S, et al. Distribution and antimicrobial activity of ciprofloxacin in human soft tissues. Antimicrob Agents Chemother. 1999;43:1307-1309. 29.Brunner M, Staβ H, Möller J, et al. Target site concentrations of ciprofloxacin after single intravenous and oral doses. Antimicrob Agents Chemother. 2002;46:3724-3730. 30. Licitra CM, Brooks RG, Sieger BE. Clinical efficacy and levels of ciprofloxacin in tissue in patients with soft tissue infection. Antimicrob Agents Chemother. 1987;31:805-807. 31. Joukhadar C, Dehghanyar P, Traunmüller F, et al. Increase of microcirculatory blood flow enhances penetration of ciprofloxacin into soft tissue. Antimicrob Agents Chemother. 2005;49:4149-4153. 32. Müller M, Brunner M, Hollenstein U, et al. Penetration of ciprofloxacin into the interstitial space of inflamed foot lesions in non- insulin-dependent diabetes mellitus patients. Antimicrob Agents Chemother. 1999;43:2056-2058. 33. Stein GE, Schoolet S, Peloquin CA, Missavage A, Havlichek DH. Linezolid tissue penetration and serum activity against strains of methicillin-resistant Staphylococcus auerus with reduced vancomycin susceptibility in diabetic patients with foot infections. J Antimicrob Chemother. 2007;60:819-823. 34. Zammit MC, Fiorentino L, Cassar K, Azzopardi LM, LaFerla G. Factors affecting gentamicin penetration in lower extremity ischemic tissues with ulcers. Int J Low Extrem Wounds. 2011;10:130-137. 35. Vella J, Busuttil F, Sammut Bartolo N, Sammut C, Ferrito V, Serracino-Inglott A. A simple HPLC-UV method for the determination of ciprofloxacin in human plasma. J Chromatogr B Analyt Technol Biomed Life Sci. 2015;989:80-85. 36. Wilson AP, Grüneberg RN. Ciprofloxacin: 10 Years of Clinical Experience. Oxford, England: Maxim Medical; 1997. 37.Anadón A, Martínez-Larrañga MR, Iturbe J, et al. Pharmacokinetics and residues of ciprofloxacin and its metabolites in broiler chickens. Res Vet Sci. 2001;71:101-109. 38.Zhang L, Wei M, Zhao C, Qi H. Determination of the inhibitory potential of 6 fluoroquinolones on CYP1A2 and CYP2C9 in human liver microsomes. Acta Pharmacol Sin. 2008;29:1507-1514. 39. Gilbert RE. Endothelial loss and repair in the vascular complications of diabetes. Circ J. 2013;77:849-856. 40.Gonzalez- Quesada C, Cavalera M, Biernacka A, et al. Thrombospondin-1 induction in the diabetic myocardium stabilizes the cardiac matrix, while promoting vascular rarefaction through angiopoietin-2 upregulation. Circ Res. 2013;113:1331-1344. 41.Nusz DJ, White DC, Dai Q, Pippen AM, Thompson MA, Walton GB. Vascular rarefaction in peripheral skeletal muscle after experimental heart failure. Am J Physiol Heart Circ Physiol. 2003;285:1554-1562. 42. Hoenig MR, Bianchi C, Rosenzweig A, Sellke FW. The cardiac microvasculature in hypertension, cardiac hypertrophy and diastolic heart failure. Curr Vasc Pharmacol. 2008;6:292-300. 43. Pladys P, Sennlaub F, Brault S, Checchin D, Lahaie I, Lê NL. Microvascular rarefactioin and decreased angiogenesis in rats with fetal programming of hypertension associated with exposure to a low- protein diet in utero. Am J Physiol Regul Integr Comp Physiol. 2005;289:1580-1588. Downloaded from ijl.sagepub.com by guest on January 3, 2016