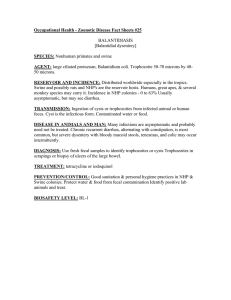
Occupational Health - Zoonotic Disease Fact Sheet #26 SPECIES: AGENT: RESERVOIR AND INCIDENCE:
advertisement
Occupational Health - Zoonotic Disease Fact Sheet #26 AMEBIASIS [Amebic Dysentery, Amebiosis] SPECIES: Nonhuman primates primary laboratory risk AGENT: Entamoeba histolytica. RESERVOIR AND INCIDENCE: The reservoir of E. histolytica is man. The infections is present worldwide but is most prevalent and severe in tropical areas, where rates may exceed 40% under conditions of crowding, poor sanitation, and poor nutrition. It is estimated that there are about 50 million case of invasive amebiasis and 40,000100,000 deaths annually worldwide. In temperate areas, however, amebiasis tends to be asymptomatic or a mild, chronic infection that often remains undiagnosed. In the USA, seropositive rates up to 2-5% have been reported in some populations. Reported incidence of 0-31% in the feces of clinically normal Rhesus monkeys, 2-67% in Chimps, and up to 30% in other NHP. TRANSMISSION: Transmission may be by ingestion of infective cysts, contaminated water or food, by flies, or fomites. Resistant cysts or more fragile trophozoites CYSTS are the INFECTIOUS form found in the stool of asymptomatic carriers or patients with mild disease. The cysts remain viable, if moist and cool for 12 days. They remain viable for 30 days in water. Laboratory animal personnel are usually infected from fecal matter transferred to the skin or clothing. DISEASE IN ANIMALS: In dogs, infection by E. histolytica is generally asymptomatic and frequently localized in the cecum. Occasionally, it can invade tissues and cause acute or chronic amebiasis. Rhesus monkeys are generally resistant and usually experience asymptomatic infection, but chronic, mild colitis can occur. In chimpanzees, the infection can persist for a long time, in most cases subclinically, but sometimes it invades the tissues causing ulcerative colitis and hepatic abscesses. New World monkeys are considered more susceptible to the disease than Asian or African monkeys. Wild rats can also harbor E. histolytica; the protozoan can be found in the large intestine as a commensal or it can invade the mucosa and cause amebic dysentery. DISEASE IN HUMANS: Mild to moderate colitis: recurrent diarrhea and abdominal cramps, sometimes alternating with constipation; mucus may be present; blood is usually absent. Severe colitis: semiformed to liquid stools streaked with blood and mucus, fever, colic, prostration. In fulminant cases, ileus, perforation, peritonitis, and hemorrhage occur. Hepatic amebiasis: fever, hepatomegaly, pain, localized tenderness. DIAGNOSIS: Use fresh fecal specimen to identify cysts or trophozoites. Sedimentation. Must measure to distinguish from other nonpathogenic amoebae. Indirect HI For hepatic amebiasis, ultrasonography can locate the cyst and fine needle aspiration is performed to find the organism. TREATMENT: May require the concurrent or sequential use of several drugs. The tissue amebicides dehydroemetine and emetine act on organisms in the bowel wall and in other tissue but not in gut lumen. Chloroquine is active principally against amebas in the liver. The luminal amebicides diloxanide furoate, iodoquinol, and paromomycin act on organisms in the bowel lumen but are ineffective against amebas in the bowel wall or other tissue. Metronidazole is unique in that it is effective both in the lumen and in the wall and in other tissue. However, when used alone, it only cures 50% of the cases. PREVENTION/CONTROL: Strict sanitation & personal hygiene, protective clothing and gloves. Fecal screening of NHP. Protect water supply from fecal contamination. Usual chlorine levels don't destroy cysts. *10ppm chlorine residual necessary to destroy cysts Heat to 50oC (122oF) kills cysts. Adequate cooking to destroy cysts. Protect food from fly contamination. BIOSAFETY LEVEL: BL-1