Charting a New Course for Nursing Documentation Nov. 16, 2015 Update
advertisement

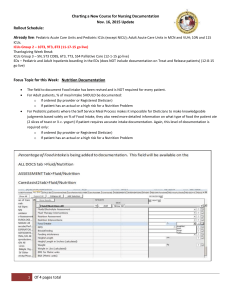
Charting a New Course for Nursing Documentation Nov. 16, 2015 Update Rollout Schedule: Already live: Pediatric Acute Care Units and Pediatric ICUs (except NICU); Adult Acute Care Units in MCN and VUH; 10N and 11S ICUs. ICUs Group 2 – 10T3, 9T3, 8T3 (11-17-15 go live) Thanksgiving Week Break ICUs Group 3 – 5N, 5T3 COBS, 6T3, 7T3, S54 Palliative Care (12-1-15 go live) EDs – Pediatric and Adult Inpatients boarding in the EDs (does NOT include documentation on Treat and Release patients) (12-8-15 go live) Focus Topic for this Week: Nutrition Documentation The field to document Food Intake has been revised and is NOT required for every patient. % of meal Intake SHOULD be documented: o If ordered (by provider or Registered Dietician) o If patient has an actual or a high risk for a Nutrition Problem Pediatric patients with orders for Calorie Counts will need to write on calorie count sheet specific details regarding exactly what was eaten because the Self Service Meal Process makes it impossible for Dieticians to make knowledgeable judgments about caloric intake based solely on % of Food Intake. A calorie count sheet will be provided for this purpose. For adult patients, calorie count sheets are NOT used and caloric intake is based solely on documentation of % of food intake. 1 Of 4 pages total One of the key documentation fields that drives ongoing Nutrition Screening (after the initial screen done on admission based on response to Nursing Admission History questions) is the Braden sub score for Nutritional Status. If you hover over the Nutrition (Braden) result, it shows the definitions to document correctly. Unfortunately, a recent small sampling of documentation shows that our Nutrition Braden sub-scores vary significantly from the national averages indicating we may not be accurately estimating Nutritional Status. To score this result as adequate, the patient should be consuming 75% of nutritional products provided by Dietary (includes meal trays, snacks, tube feedings, and other nutritional supplements but NOT TPN/Lipids). To score as excellent, the patient should be consuming most (95%) provided nourishments. If the patient’s intake is less than 75%, their intake is probably inadequate and if less than 50%, it is very poor. Please use these guidelines when assessing Braden Nutrition Status. Dieticians follow these sub scales to determine when additional nutrition is needed. Issue, Concern, Request: 1. Need to be able to document family presence at bedside. 2. If patient has an arrhythmia and the return to Normal Sinus Rhythm, 3. Having airway suctioning under artificial airway interventions is not working. 2 Of 4 pages total Change: 1. In Psychosocial Assessment, there is a new result “Family Presence”. 2. In Cardiac Assessment, EKG Rhythm, “return to NSR” added to dropdown list. 3. Suctioning was added back to Respiratory Interventions drop down. 1. 2. 3 Of 4 pages total 3. For access to FAQs, Training Information, and other Resources: http://www.mc.vanderbilt.edu/root/vumc.php?site=sss2&doc=47409 4 Of 4 pages total