CULTURALLY NUANCED TEACHING Published by the Faculty Development Office SUMMER 2012
TEACHING CONTINUED FROM PAGE 4
“The UC Davis Schools of Health certainly have focused individually on interdisciplinary education and an interest in improving educational processes, but this workshop provides one of the first opportunities to offer this curriculum throughout the Schools of Health. In particular, we are excited that we will be able to improve knowledge at both the educator and student levels,” Bakerjian said.
The curriculum will help elevate awareness of “implicit bias” (also known as “unconscious bias”), described in the
October-November 2010 edition of the
Faculty Newsletter (click the “newsletter” tab at http://www.ucdmc.ucdavis.edu/ facultydev/).
“Because of implicit bias, the tendency is for faculty to project student failure onto students – that is, focus on student deficits rather than student assets, and think in terms of how the students’ cognitive skills or knowledge must change, rather than how attitudes and beliefs affect students’ learning,” Hass said. “Science and medical education curricula are traditionally content-driven and skillsbased. While content will continue to be an important aspect of curriculum, our faculty development workshops will concentrate on bringing those unconscious biases to the surface and shifting faculty focus toward culturally nuanced learning and teaching in the context of that curriculum.”
The initial phase of workshop development is a needs assessment to identify approaches by which faculty members can improve support, education, retention and graduation rates of culturally diverse and disadvantaged students in the
FNP/PA program, the School of Medicine, and the School of Nursing. The needs assessment, discussions with collaborators from the Schools of Health, and models used by other educational programs will influence the content and structure of the training sessions.
The workshops, participation in which will be free of charge, likely will be conducted in a discussion and case-based setting.
“Participants will be expected to
‘go forth’ and share with others in their departments what they’ve learned, so we’re looking for broad cross-representation from Schools of Health faculty,” explained
Devin Rifkin, CCRP, the program’s project coordinator in the Department of Family and Community Medicine. “In addition to the workshops, we plan to conduct focus groups with current students who may be at risk of withdrawal or dismissal as a result of academic or clinical difficulties they are encountering. Our hope is to identify trends and patterns related to the difficulties they are having.”
Rifkin said that the strategies developed through the curriculum will be useful in enhancing student support services for culturally diverse and disadvantaged students.
“These services will be delivered both in the classroom and through online platforms,” Rifkin added. “The paramount goal is to enhance the knowledge and skills of faculty in working with culturally diverse and disadvantaged students.”
Although the HRSA grant does not include a specific research component,
Bakerjian and her colleagues will conduct evaluations of faculty and student knowledge before and after the interventions.
“That information will inform how we move forward with this program,” Bakerjian explained. “We will disseminate our outcomes and processes along the way, internally to our faculty colleagues and externally through professional conferences.”
Bakerjian welcomes broad faculty participation in planning and enrollment in the workshops, the first of which likely will be presented during the coming fall quarter.
“We hope that faculty who are either experts in this area or want to know more about how to improve the educational process for culturally diverse and underserved students will participate in the workshops,” she said.
“We really encourage wide participation, and we would love to hear from you.”
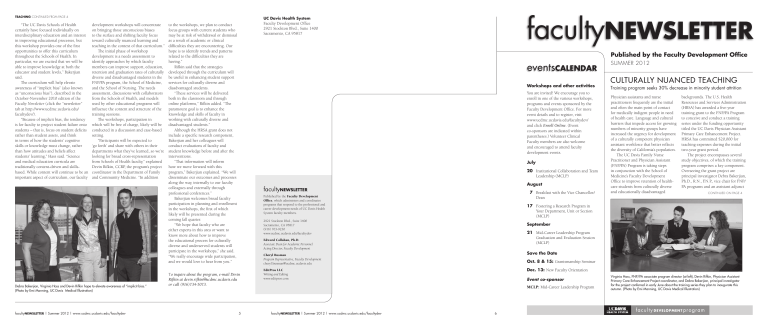
Debra Bakerjian, Virginia Hass and Devin Rifkin hope to elevate awareness of “implicit bias.”
(Photo by Emi Manning, UC Davis Medical Illustration)
T o inquire about the program, e-mail Devin
Rifkin at devin.rifkin@ucdmc.ucdavis.edu or call (916)734-5073.
faculty NEWSLETTER | Summer 2012 | www.ucdmc.ucdavis.edu/facultydev 5
UC Davis Health System
Faculty Development Office
2921 Stockton Blvd., Suite 1400
Sacramento, CA 95817 faculty
NEWSLETTER
Published by the Faculty Development
Office , which administers and coordinates programs that respond to the professional and career development needs of UC Davis Health
System faculty members.
2921 Stockton Blvd., Suite 1400
Sacramento, CA 95817
(916) 703-9230 www.ucdmc.ucdavis.edu/facultydev
Edward Callahan, Ph.D.
Associate Dean for Academic Personnel
Acting Director, Faculty Development
Cheryl Busman
Program Representative, Faculty Development cheryl.busman@ucdmc.ucdavis.edu
EditPros LLC
Writing and Editing www.editpros.com
faculty NEWSLETTER | Summer 2012 | www.ucdmc.ucdavis.edu/facultydev 6
Workshops and other activities
You are invited! We encourage you to enroll in one of the various workshops, programs and events sponsored by the
Faculty Development Office. For more event details and to register, visit www.ucdmc.ucdavis.edu/facultydev/ and click Enroll Online . (Event co-sponsors are indicated within parentheses.) Volunteer Clinical
Faculty members are also welcome and encouraged to attend faculty development events.
July
20 Institutional Collaboration and Team
Leadership (MCLP)
August
7 Breakfast with the Vice Chancellor/
Dean
17 Fostering a Research Program in
Your Department, Unit or Section
(MCLP)
September
21 Mid-Career Leadership Program
Graduation and Evaluation Session
(MCLP)
Save the Date
Oct. 8 & 15: Grantsmanship Seminar
Dec. 13: New Faculty Orientation
Event co-sponsor
MCLP: Mid-Career Leadership Program
Published by the Faculty Development Office
SUMMER 2012
CULTURALLY NUANCED TEACHING
Training program seeks 30% decrease in minority student attrition
Physician assistants and nurse practitioners frequently are the initial and often the main point of contact for medically indigent people in need of health care. Language and cultural barriers that impede access for growing numbers of minority groups have increased the urgency for development of a culturally competent physician assistant workforce that better reflects the diversity of California’s population.
The UC Davis Family Nurse
Practitioner and Physician Assistant
(FNP/PA) Program is taking steps in conjunction with the School of
Medicine’s Faculty Development
Office to improve retention of healthcare students from culturally diverse and educationally disadvantaged backgrounds. The U.S. Health
Resources and Services Administration
(HRSA) has awarded a five-year training grant to the FNP/PA Program to conceive and conduct a training series under the funding opportunity titled the UC Davis Physician Assistant
Primary Care Enhancement Project.
HRSA has committed $20,000 for teaching expenses during the initial two-year grant period.
The project encompasses several study objectives, of which the training program comprises a key component.
Overseeing the grant project are principal investigator Debra Bakerjian,
Ph.D., R.N., F.N.P., vice chair for FNP/
PA programs and an assistant adjunct
CONTINUED ON PAGE 4
Virginia Hass, FNP/PA associate program director (at left), Devin Rifkin, Physician Assistant
Primary Care Enhancement Project coordinator, and Debra Bakerjian, principal investigator for the project conferred in early June about the training series they plan to inaugurate this autumn. (Photo by Emi Manning, UC Davis Medical Illustration)
office
VISIT
RADIOLOGIST FRANK BROWN OFFERS
50-YEAR PERSPECTIVE FOR RESIDENTS
Among UC Davis Health System volunteer clinical faculty members, neuroradiologist
Frank Brown has an unequaled legacy of support. His involvement predates the opening of the School of Medicine and the
UC Davis Medical Center.
An enduring pillar of community support, Brown at age 81 remains involved in clinical work and teaching on the Sacramento campus, despite severe continual pain and fine-motor impairment he has endured for 15 years. And he has willingly worked as a volunteer for UC Davis without pay throughout the past 45 years.
When Brown obtained his M.D. degree at Stanford University in 1955, he envisioned a career in academic internal medicine. While serving his internship at UCLA’s teaching hospital, however, he came to an important realization.
“I found that a lot of my diagnoses were made in the radiology department instead of in the internal medicine clinic and wards,” Brown said. He consequently served a one-year residency in radiology at Stanford University Hospital, working with fluoroscopy and primitive X-ray imagery.
Brown, who had met and married his wife, Susan, while in medical school, served two years in the U.S. Air Force in the radiobiology department at the
Air Force School of Aviation Medicine at
Randolph Air Force Base in San Antonio.
After his discharge, he completed a second residency in radiology at UCLA and became an assistant professor in the department. But radiologist Russell
McFall, a former UCLA radiology resident who had joined Radiological Associates of Sacramento (RAS), recruited Brown to join RAS as a diagnostic radiologist. Brown worked for RAS, specializing in cerebral angiography and CT and MRI scanning, from 1962 until his retirement in 1995.
Brown befriended the School of
Medicine’s founding dean, John Tupper, and served as a consultant during the formative years of the school. Brown subsequently volunteered as a chest radiographer for UC Davis, and began working with residents and interns. When the UC Davis Department of Radiology obtained its first MRI unit in the 1980s,
Brown relieved radiologist Arthur Dublin of some of the MRI imagery reading workload. Raymond S. Dougherty,
M.D., clinical professor and chair of the
Department of Radiology, regards Brown as a role model for young physicians.
“Dr. Brown brings a much-needed perspective to the education of our medical students and residents. He really enjoys giving back to the medical profession and community,” Dougherty said.
Brown landed on the other side of a CT scanner, unfortunately, in 1997. During a vacation in Maui, Brown was boogieboarding on a beach when he flipped and slammed into the sand head first, causing a central cord spinal injury at C6-7.
“I was temporarily quadriplegic. In a few hours some gross motor function came back,” said Brown, who regained the ability to walk with a cane after six months of rehabilitation. “Since then I have had severe symptoms of crippling pain, paresthesia in all my extremities, and I have lost my fine motion.”
Within a year of the accident, Brown resumed volunteering at UC Davis.
These days, he works with medical students, interns and residents in clinical evaluations.
“I ask them to tell me what they observe, how they think that fits together with clinical information that they’ve gathered, and I ask for their diagnosis and the treatment they would use. That’s the way I like to teach,” Brown said.
Brown lives alone now in the house into which he and Susan had moved 50 years ago to raise their family. Susan died in 2009 of died of chronic pulmonary disease. Brown has remained busy not only at UC Davis, but also in leading prayer groups through the Episcopal
Church for inmates at Folsom Prison.
“Keeping occupied is a key to coping with neurological pain,” he explained.
Arthur Dublin, professor of radiology and Medical Director of the UC Davis
Imaging Center in Rocklin, offers high praise for Brown.
“Frank says he is very blessed and honored to be able to donate his time and skills in teaching our residents at UC
Davis Medical Center,” Dublin said. “I think we are the ones who are blessed by his generosity.” faculty NEWSLETTER | Summer 2012 | www.ucdmc.ucdavis.edu/facultydev 2 faculty
ROUNDS
A WELCOME TO NEW
FACULTY COLLEAGUES
Apesoa-Varano Khaderi
Each edition of the Faculty Newsletter introduces several faculty colleagues who recently joined the UC Davis
Health System community. Watch for more new clinical and research staff members in the next issue.
Ester Apesoa-Varano conducts studies in geriatrics
Sociologist Ester Carolina Apesoa-
Varano, Ph.D., a founding member of the Betty Irene Moore School of Nursing faculty, is conducting studies in geriatrics intended to lead to advancements in health care for older people. Apesoa-
Varano, an assistant professor, is investigating health-care professions and organizational structures with a focus on the role of nurses, health disparities and underserved populations, and teamwork models and interprofessional collaborations in health care.
She recently completed a year as a scholar in the prestigious Building
Interdisciplinary Research Careers in
Women’s Health (BIRCWH) program, an initiative of the National Institutes of
Health. She mentors Nursing Science and
Health-Care Leadership Graduate Group students to develop the skills necessary to lead complex health systems.
S. Khizer Khaderi specializes in optic nerve disorders
S. Khizer Khaderi, M.D., M.P.H., an assistant professor of ophthalmology, is a clinical and surgical neuroophthalmologist who specializes in genetic diseases of the optic nerve, retinal ganglion cell expression, and visual psychophysics.
He has been granted four patents for processes by which to promote retinogeniculo-cortical pathway development.
Khaderi’s research studies include comparing magnocellular ganglion cell function in collegiate athletes and nonathletes. He is in the process of creating a sports vision lab at UC Davis Eye
Center that will specialize in traumatic brain injury and visual training and rehabilitation. Khaderi says it will be the first such facility on the West Coast.
Other new colleagues n
Biostatistician Heejung Bang,
Ph.D., an associate professor in the
Department of Public Health Sciences’
Division of Biostatistics, has expertise in epidemiology and methodology for clinical trials. She is researching statistical methods for observational studies and clinical trials, medical cost and cost-effectiveness analysis, and disease prediction modeling.
She recently investigated the role of epidemiology and biostatistics in health news reporting, and is co-investigator of a study of patient counseling as a means to reduce inappropriate diagnostic testing. Earlier this year, the American
Diabetes Association adopted a diabetes risk test for patients that Bang and her colleagues developed.
n
Hugh B. Black, M.D., an associate clinical professor of pulmonary and critical care medicine and an associate faculty member in the
Bioethics Program, maintains a general pulmonary clinic and is medical director of the Neurosurgical Intensive
Care Unit. His practice encompasses management of critically ill patients who require medical management integrated with complex cardiothoracic, thoracic and otolaryngological procedures, as well as management of patients who have severe neurological injury requiring medical management integrated with neurological therapy or neurosurgical procedures. He is conducting research in ways to improve the quality of ICU and critical care quality, along with critical care curriculum development.
n
Cardiologist Thomas W. R. Smith,
M.D., an assistant clinical professor of internal medicine, is the director of the adult echocardiography laboratory. He conducts a general cardiology practice with an emphasis on cardiovascular imaging, including
CT, MRI and echocardiography. Smith, who is board-certified in internal medicine, cardiovascular medicine, echocardiography and cardiovascular computed tomography, is researching cardiovascular imaging focusing on structural heart disease with an emphasis of planning and image guidance for percutaneous structural heart procedures.
n
Yanhong Zhang, M.D., who is board-certified in anatomic and clinical pathology, specializes in breast and pulmonary pathology. In her translational research on breast cancer, she is concentrating on validation of a novel gene as a potential tissue biomarker that may guide diagnosis and treatment in breast cancer. She is an assistant professor of pathology and laboratory medicine, and a member of the College of American Pathologists, and the United States and Canadian
Academy of Pathology.
faculty NEWSLETTER | Summer 2012 | www.ucdmc.ucdavis.edu/facultydev 3 view
POINT
BY LYDIA P. HOWELL AND
AMPARO VILLABLANCA
PROMOTING CAREER-
FLEXIBILITY POLICIES
Lydia Howell
HAS PROMISING RESULTS
Amparo Villablanca
Awareness of UC Davis Health System career flexibility policies has risen among faculty members, while barriers that discouraged their use have declined during the past year. These and other encouraging findings have emerged since the spring of
2010, when we initiated a four-year NIHfunded research study and intervention program titled “Women’s Careers in
Biomedical Sciences: Family-Friendly
Policies and Career Flexibility.”
The project focuses on the effectiveness of the School of Medicine’s family leave policies and practices. Our interventions have included workshops, presentations in grand rounds, publication of a brochure and faculty development articles, and an ongoing faculty survey, all of which have elevated awareness of flexibility policies.
The survey component of our study encompasses male and female faculty members in the schools of Medicine and
Veterinary Medicine, and in the College of Biological Sciences. We compared awareness, usage and satisfaction increases evident in our most recent results against our baseline survey, which showed that faculty awareness and use of these policies in 2010 had been disappointingly low.
Our most recent survey revealed that awareness of flexibility policies demonstrably increased during the past year, including those for child-bearing leaves; reduction of hours or modification of duties to accommodate life changes; tenure-clock extension; and deferral of reviews. Perceived barriers to use
(including overburdening colleagues, and inability to stop work on funded projects) also improved, and we found broad support for the flexibility policies among faculty in all generations.
Some of our findings reveal a need for more focused intervention. Young male and older female faculty members emerged as groups at risk for work-life conflict and resulting career dissatisfaction.
Development of new policies may be required to respond to their needs. We also note cognitive dissonance between desire to use policies and concerns about doing so. Flexible career policies are tools that are commonly used in other industries to attract and retain talent, and have the potential to be equally effective in academic medicine. Such policies must be accompanied by awareness and a supportive culture that encourages their use, so that we may have greater success in faculty recruitment, retention and career advancement.
We urge faculty members to ask their department chairs, managers and the office of academic personnel about leave policies. We plan to continue activities to make our school a welcoming environment for all members of the faculty. Visit http://www.ucdmc.ucdavis.
edu/academicpersonnel/academicleaves/ index.html to view the policies. Please attend one of our future workshops, and participate in our forthcoming surveys.
Amparo C. Villablanca is professor and Lazda Endowed Chair in Women’s
Cardiovascular Medicine; director of the Women’s Cardiovascular Medicine
Program; and associate director of the
Women’s Center for Health.
Lydia P. Howell is professor and chair of the Department of Pathology and
Laboratory Medicine.
TEACHING CONTINUED FROM PAGE 1 professor in the Betty Irene Moore
School of Nursing; and Virginia
Hass, R.N., D.N.P., F.N.P.-C,
P.A.-C, the FNP/PA associate program director, who will head the faculty education aim of the grant.
The training curriculum is being designed to help faculty members refine skills and strategies for retention of minority and disadvantaged students, among whom the attrition rate is disproportionally greater than the student body at large.
The principal objective of the training program is attainment of a 30 percent decrease in student attrition attributable to academic reasons. That correlates to two other Physician Assistant Primary
Care Enhancement Project objectives:
• Impel development of an underserved primary-care rotation to increase the number of FNP/PA students who explore careers in medically underserved communities.
• Stimulate a 30 percent increase in the proportion of FNP/
PA graduates who obtain employment in medically underserved communities.
Bakerjian and Hass are encouraging faculty members not only to participate in the training workshops, but also help develop them.
Planning work is proceeding in consultation with faculty members from the UC Davis School of Education and the Department of Chicana/Chicano Studies. Bakerjian observes that the curriculum will be intended to bolster the cultural competence of faculty members not only in the FNP/PA program, but in all other Schools of Health programs as well.
CONTINUED ON PAGE 5 faculty NEWSLETTER | Summer 2012 | www.ucdmc.ucdavis.edu/facultydev 4
office
VISIT
RADIOLOGIST FRANK BROWN OFFERS
50-YEAR PERSPECTIVE FOR RESIDENTS
Among UC Davis Health System volunteer clinical faculty members, neuroradiologist
Frank Brown has an unequaled legacy of support. His involvement predates the opening of the School of Medicine and the
UC Davis Medical Center.
An enduring pillar of community support, Brown at age 81 remains involved in clinical work and teaching on the Sacramento campus, despite severe continual pain and fine-motor impairment he has endured for 15 years. And he has willingly worked as a volunteer for UC Davis without pay throughout the past 45 years.
When Brown obtained his M.D. degree at Stanford University in 1955, he envisioned a career in academic internal medicine. While serving his internship at UCLA’s teaching hospital, however, he came to an important realization.
“I found that a lot of my diagnoses were made in the radiology department instead of in the internal medicine clinic and wards,” Brown said. He consequently served a one-year residency in radiology at Stanford University Hospital, working with fluoroscopy and primitive X-ray imagery.
Brown, who had met and married his wife, Susan, while in medical school, served two years in the U.S. Air Force in the radiobiology department at the
Air Force School of Aviation Medicine at
Randolph Air Force Base in San Antonio.
After his discharge, he completed a second residency in radiology at UCLA and became an assistant professor in the department. But radiologist Russell
McFall, a former UCLA radiology resident who had joined Radiological Associates of Sacramento (RAS), recruited Brown to join RAS as a diagnostic radiologist. Brown worked for RAS, specializing in cerebral angiography and CT and MRI scanning, from 1962 until his retirement in 1995.
Brown befriended the School of
Medicine’s founding dean, John Tupper, and served as a consultant during the formative years of the school. Brown subsequently volunteered as a chest radiographer for UC Davis, and began working with residents and interns. When the UC Davis Department of Radiology obtained its first MRI unit in the 1980s,
Brown relieved radiologist Arthur Dublin of some of the MRI imagery reading workload. Raymond S. Dougherty,
M.D., clinical professor and chair of the
Department of Radiology, regards Brown as a role model for young physicians.
“Dr. Brown brings a much-needed perspective to the education of our medical students and residents. He really enjoys giving back to the medical profession and community,” Dougherty said.
Brown landed on the other side of a CT scanner, unfortunately, in 1997. During a vacation in Maui, Brown was boogieboarding on a beach when he flipped and slammed into the sand head first, causing a central cord spinal injury at C6-7.
“I was temporarily quadriplegic. In a few hours some gross motor function came back,” said Brown, who regained the ability to walk with a cane after six months of rehabilitation. “Since then I have had severe symptoms of crippling pain, paresthesia in all my extremities, and I have lost my fine motion.”
Within a year of the accident, Brown resumed volunteering at UC Davis.
These days, he works with medical students, interns and residents in clinical evaluations.
“I ask them to tell me what they observe, how they think that fits together with clinical information that they’ve gathered, and I ask for their diagnosis and the treatment they would use. That’s the way I like to teach,” Brown said.
Brown lives alone now in the house into which he and Susan had moved 50 years ago to raise their family. Susan died in 2009 of died of chronic pulmonary disease. Brown has remained busy not only at UC Davis, but also in leading prayer groups through the Episcopal
Church for inmates at Folsom Prison.
“Keeping occupied is a key to coping with neurological pain,” he explained.
Arthur Dublin, professor of radiology and Medical Director of the UC Davis
Imaging Center in Rocklin, offers high praise for Brown.
“Frank says he is very blessed and honored to be able to donate his time and skills in teaching our residents at UC
Davis Medical Center,” Dublin said. “I think we are the ones who are blessed by his generosity.” faculty NEWSLETTER | Summer 2012 | www.ucdmc.ucdavis.edu/facultydev 2 faculty
ROUNDS
A WELCOME TO NEW
FACULTY COLLEAGUES
Apesoa-Varano Khaderi
Each edition of the Faculty Newsletter introduces several faculty colleagues who recently joined the UC Davis
Health System community. Watch for more new clinical and research staff members in the next issue.
Ester Apesoa-Varano conducts studies in geriatrics
Sociologist Ester Carolina Apesoa-
Varano, Ph.D., a founding member of the Betty Irene Moore School of Nursing faculty, is conducting studies in geriatrics intended to lead to advancements in health care for older people. Apesoa-
Varano, an assistant professor, is investigating health-care professions and organizational structures with a focus on the role of nurses, health disparities and underserved populations, and teamwork models and interprofessional collaborations in health care.
She recently completed a year as a scholar in the prestigious Building
Interdisciplinary Research Careers in
Women’s Health (BIRCWH) program, an initiative of the National Institutes of
Health. She mentors Nursing Science and
Health-Care Leadership Graduate Group students to develop the skills necessary to lead complex health systems.
S. Khizer Khaderi specializes in optic nerve disorders
S. Khizer Khaderi, M.D., M.P.H., an assistant professor of ophthalmology, is a clinical and surgical neuroophthalmologist who specializes in genetic diseases of the optic nerve, retinal ganglion cell expression, and visual psychophysics.
He has been granted four patents for processes by which to promote retinogeniculo-cortical pathway development.
Khaderi’s research studies include comparing magnocellular ganglion cell function in collegiate athletes and nonathletes. He is in the process of creating a sports vision lab at UC Davis Eye
Center that will specialize in traumatic brain injury and visual training and rehabilitation. Khaderi says it will be the first such facility on the West Coast.
Other new colleagues n
Biostatistician Heejung Bang,
Ph.D., an associate professor in the
Department of Public Health Sciences’
Division of Biostatistics, has expertise in epidemiology and methodology for clinical trials. She is researching statistical methods for observational studies and clinical trials, medical cost and cost-effectiveness analysis, and disease prediction modeling.
She recently investigated the role of epidemiology and biostatistics in health news reporting, and is co-investigator of a study of patient counseling as a means to reduce inappropriate diagnostic testing. Earlier this year, the American
Diabetes Association adopted a diabetes risk test for patients that Bang and her colleagues developed.
n
Hugh B. Black, M.D., an associate clinical professor of pulmonary and critical care medicine and an associate faculty member in the
Bioethics Program, maintains a general pulmonary clinic and is medical director of the Neurosurgical Intensive
Care Unit. His practice encompasses management of critically ill patients who require medical management integrated with complex cardiothoracic, thoracic and otolaryngological procedures, as well as management of patients who have severe neurological injury requiring medical management integrated with neurological therapy or neurosurgical procedures. He is conducting research in ways to improve the quality of ICU and critical care quality, along with critical care curriculum development.
n
Cardiologist Thomas W. R. Smith,
M.D., an assistant clinical professor of internal medicine, is the director of the adult echocardiography laboratory. He conducts a general cardiology practice with an emphasis on cardiovascular imaging, including
CT, MRI and echocardiography. Smith, who is board-certified in internal medicine, cardiovascular medicine, echocardiography and cardiovascular computed tomography, is researching cardiovascular imaging focusing on structural heart disease with an emphasis of planning and image guidance for percutaneous structural heart procedures.
n
Yanhong Zhang, M.D., who is board-certified in anatomic and clinical pathology, specializes in breast and pulmonary pathology. In her translational research on breast cancer, she is concentrating on validation of a novel gene as a potential tissue biomarker that may guide diagnosis and treatment in breast cancer. She is an assistant professor of pathology and laboratory medicine, and a member of the College of American Pathologists, and the United States and Canadian
Academy of Pathology.
faculty NEWSLETTER | Summer 2012 | www.ucdmc.ucdavis.edu/facultydev 3 view
POINT
BY LYDIA P. HOWELL AND
AMPARO VILLABLANCA
PROMOTING CAREER-
FLEXIBILITY POLICIES
Lydia Howell
HAS PROMISING RESULTS
Amparo Villablanca
Awareness of UC Davis Health System career flexibility policies has risen among faculty members, while barriers that discouraged their use have declined during the past year. These and other encouraging findings have emerged since the spring of
2010, when we initiated a four-year NIHfunded research study and intervention program titled “Women’s Careers in
Biomedical Sciences: Family-Friendly
Policies and Career Flexibility.”
The project focuses on the effectiveness of the School of Medicine’s family leave policies and practices. Our interventions have included workshops, presentations in grand rounds, publication of a brochure and faculty development articles, and an ongoing faculty survey, all of which have elevated awareness of flexibility policies.
The survey component of our study encompasses male and female faculty members in the schools of Medicine and
Veterinary Medicine, and in the College of Biological Sciences. We compared awareness, usage and satisfaction increases evident in our most recent results against our baseline survey, which showed that faculty awareness and use of these policies in 2010 had been disappointingly low.
Our most recent survey revealed that awareness of flexibility policies demonstrably increased during the past year, including those for child-bearing leaves; reduction of hours or modification of duties to accommodate life changes; tenure-clock extension; and deferral of reviews. Perceived barriers to use
(including overburdening colleagues, and inability to stop work on funded projects) also improved, and we found broad support for the flexibility policies among faculty in all generations.
Some of our findings reveal a need for more focused intervention. Young male and older female faculty members emerged as groups at risk for work-life conflict and resulting career dissatisfaction.
Development of new policies may be required to respond to their needs. We also note cognitive dissonance between desire to use policies and concerns about doing so. Flexible career policies are tools that are commonly used in other industries to attract and retain talent, and have the potential to be equally effective in academic medicine. Such policies must be accompanied by awareness and a supportive culture that encourages their use, so that we may have greater success in faculty recruitment, retention and career advancement.
We urge faculty members to ask their department chairs, managers and the office of academic personnel about leave policies. We plan to continue activities to make our school a welcoming environment for all members of the faculty. Visit http://www.ucdmc.ucdavis.
edu/academicpersonnel/academicleaves/ index.html to view the policies. Please attend one of our future workshops, and participate in our forthcoming surveys.
Amparo C. Villablanca is professor and Lazda Endowed Chair in Women’s
Cardiovascular Medicine; director of the Women’s Cardiovascular Medicine
Program; and associate director of the
Women’s Center for Health.
Lydia P. Howell is professor and chair of the Department of Pathology and
Laboratory Medicine.
TEACHING CONTINUED FROM PAGE 1 professor in the Betty Irene Moore
School of Nursing; and Virginia
Hass, R.N., D.N.P., F.N.P.-C,
P.A.-C, the FNP/PA associate program director, who will head the faculty education aim of the grant.
The training curriculum is being designed to help faculty members refine skills and strategies for retention of minority and disadvantaged students, among whom the attrition rate is disproportionally greater than the student body at large.
The principal objective of the training program is attainment of a 30 percent decrease in student attrition attributable to academic reasons. That correlates to two other Physician Assistant Primary
Care Enhancement Project objectives:
• Impel development of an underserved primary-care rotation to increase the number of FNP/PA students who explore careers in medically underserved communities.
• Stimulate a 30 percent increase in the proportion of FNP/
PA graduates who obtain employment in medically underserved communities.
Bakerjian and Hass are encouraging faculty members not only to participate in the training workshops, but also help develop them.
Planning work is proceeding in consultation with faculty members from the UC Davis School of Education and the Department of Chicana/Chicano Studies. Bakerjian observes that the curriculum will be intended to bolster the cultural competence of faculty members not only in the FNP/PA program, but in all other Schools of Health programs as well.
CONTINUED ON PAGE 5 faculty NEWSLETTER | Summer 2012 | www.ucdmc.ucdavis.edu/facultydev 4
office
VISIT
RADIOLOGIST FRANK BROWN OFFERS
50-YEAR PERSPECTIVE FOR RESIDENTS
Among UC Davis Health System volunteer clinical faculty members, neuroradiologist
Frank Brown has an unequaled legacy of support. His involvement predates the opening of the School of Medicine and the
UC Davis Medical Center.
An enduring pillar of community support, Brown at age 81 remains involved in clinical work and teaching on the Sacramento campus, despite severe continual pain and fine-motor impairment he has endured for 15 years. And he has willingly worked as a volunteer for UC Davis without pay throughout the past 45 years.
When Brown obtained his M.D. degree at Stanford University in 1955, he envisioned a career in academic internal medicine. While serving his internship at UCLA’s teaching hospital, however, he came to an important realization.
“I found that a lot of my diagnoses were made in the radiology department instead of in the internal medicine clinic and wards,” Brown said. He consequently served a one-year residency in radiology at Stanford University Hospital, working with fluoroscopy and primitive X-ray imagery.
Brown, who had met and married his wife, Susan, while in medical school, served two years in the U.S. Air Force in the radiobiology department at the
Air Force School of Aviation Medicine at
Randolph Air Force Base in San Antonio.
After his discharge, he completed a second residency in radiology at UCLA and became an assistant professor in the department. But radiologist Russell
McFall, a former UCLA radiology resident who had joined Radiological Associates of Sacramento (RAS), recruited Brown to join RAS as a diagnostic radiologist. Brown worked for RAS, specializing in cerebral angiography and CT and MRI scanning, from 1962 until his retirement in 1995.
Brown befriended the School of
Medicine’s founding dean, John Tupper, and served as a consultant during the formative years of the school. Brown subsequently volunteered as a chest radiographer for UC Davis, and began working with residents and interns. When the UC Davis Department of Radiology obtained its first MRI unit in the 1980s,
Brown relieved radiologist Arthur Dublin of some of the MRI imagery reading workload. Raymond S. Dougherty,
M.D., clinical professor and chair of the
Department of Radiology, regards Brown as a role model for young physicians.
“Dr. Brown brings a much-needed perspective to the education of our medical students and residents. He really enjoys giving back to the medical profession and community,” Dougherty said.
Brown landed on the other side of a CT scanner, unfortunately, in 1997. During a vacation in Maui, Brown was boogieboarding on a beach when he flipped and slammed into the sand head first, causing a central cord spinal injury at C6-7.
“I was temporarily quadriplegic. In a few hours some gross motor function came back,” said Brown, who regained the ability to walk with a cane after six months of rehabilitation. “Since then I have had severe symptoms of crippling pain, paresthesia in all my extremities, and I have lost my fine motion.”
Within a year of the accident, Brown resumed volunteering at UC Davis.
These days, he works with medical students, interns and residents in clinical evaluations.
“I ask them to tell me what they observe, how they think that fits together with clinical information that they’ve gathered, and I ask for their diagnosis and the treatment they would use. That’s the way I like to teach,” Brown said.
Brown lives alone now in the house into which he and Susan had moved 50 years ago to raise their family. Susan died in 2009 of died of chronic pulmonary disease. Brown has remained busy not only at UC Davis, but also in leading prayer groups through the Episcopal
Church for inmates at Folsom Prison.
“Keeping occupied is a key to coping with neurological pain,” he explained.
Arthur Dublin, professor of radiology and Medical Director of the UC Davis
Imaging Center in Rocklin, offers high praise for Brown.
“Frank says he is very blessed and honored to be able to donate his time and skills in teaching our residents at UC
Davis Medical Center,” Dublin said. “I think we are the ones who are blessed by his generosity.” faculty NEWSLETTER | Summer 2012 | www.ucdmc.ucdavis.edu/facultydev 2 faculty
ROUNDS
A WELCOME TO NEW
FACULTY COLLEAGUES
Apesoa-Varano Khaderi
Each edition of the Faculty Newsletter introduces several faculty colleagues who recently joined the UC Davis
Health System community. Watch for more new clinical and research staff members in the next issue.
Ester Apesoa-Varano conducts studies in geriatrics
Sociologist Ester Carolina Apesoa-
Varano, Ph.D., a founding member of the Betty Irene Moore School of Nursing faculty, is conducting studies in geriatrics intended to lead to advancements in health care for older people. Apesoa-
Varano, an assistant professor, is investigating health-care professions and organizational structures with a focus on the role of nurses, health disparities and underserved populations, and teamwork models and interprofessional collaborations in health care.
She recently completed a year as a scholar in the prestigious Building
Interdisciplinary Research Careers in
Women’s Health (BIRCWH) program, an initiative of the National Institutes of
Health. She mentors Nursing Science and
Health-Care Leadership Graduate Group students to develop the skills necessary to lead complex health systems.
S. Khizer Khaderi specializes in optic nerve disorders
S. Khizer Khaderi, M.D., M.P.H., an assistant professor of ophthalmology, is a clinical and surgical neuroophthalmologist who specializes in genetic diseases of the optic nerve, retinal ganglion cell expression, and visual psychophysics.
He has been granted four patents for processes by which to promote retinogeniculo-cortical pathway development.
Khaderi’s research studies include comparing magnocellular ganglion cell function in collegiate athletes and nonathletes. He is in the process of creating a sports vision lab at UC Davis Eye
Center that will specialize in traumatic brain injury and visual training and rehabilitation. Khaderi says it will be the first such facility on the West Coast.
Other new colleagues n
Biostatistician Heejung Bang,
Ph.D., an associate professor in the
Department of Public Health Sciences’
Division of Biostatistics, has expertise in epidemiology and methodology for clinical trials. She is researching statistical methods for observational studies and clinical trials, medical cost and cost-effectiveness analysis, and disease prediction modeling.
She recently investigated the role of epidemiology and biostatistics in health news reporting, and is co-investigator of a study of patient counseling as a means to reduce inappropriate diagnostic testing. Earlier this year, the American
Diabetes Association adopted a diabetes risk test for patients that Bang and her colleagues developed.
n
Hugh B. Black, M.D., an associate clinical professor of pulmonary and critical care medicine and an associate faculty member in the
Bioethics Program, maintains a general pulmonary clinic and is medical director of the Neurosurgical Intensive
Care Unit. His practice encompasses management of critically ill patients who require medical management integrated with complex cardiothoracic, thoracic and otolaryngological procedures, as well as management of patients who have severe neurological injury requiring medical management integrated with neurological therapy or neurosurgical procedures. He is conducting research in ways to improve the quality of ICU and critical care quality, along with critical care curriculum development.
n
Cardiologist Thomas W. R. Smith,
M.D., an assistant clinical professor of internal medicine, is the director of the adult echocardiography laboratory. He conducts a general cardiology practice with an emphasis on cardiovascular imaging, including
CT, MRI and echocardiography. Smith, who is board-certified in internal medicine, cardiovascular medicine, echocardiography and cardiovascular computed tomography, is researching cardiovascular imaging focusing on structural heart disease with an emphasis of planning and image guidance for percutaneous structural heart procedures.
n
Yanhong Zhang, M.D., who is board-certified in anatomic and clinical pathology, specializes in breast and pulmonary pathology. In her translational research on breast cancer, she is concentrating on validation of a novel gene as a potential tissue biomarker that may guide diagnosis and treatment in breast cancer. She is an assistant professor of pathology and laboratory medicine, and a member of the College of American Pathologists, and the United States and Canadian
Academy of Pathology.
faculty NEWSLETTER | Summer 2012 | www.ucdmc.ucdavis.edu/facultydev 3 view
POINT
BY LYDIA P. HOWELL AND
AMPARO VILLABLANCA
PROMOTING CAREER-
FLEXIBILITY POLICIES
Lydia Howell
HAS PROMISING RESULTS
Amparo Villablanca
Awareness of UC Davis Health System career flexibility policies has risen among faculty members, while barriers that discouraged their use have declined during the past year. These and other encouraging findings have emerged since the spring of
2010, when we initiated a four-year NIHfunded research study and intervention program titled “Women’s Careers in
Biomedical Sciences: Family-Friendly
Policies and Career Flexibility.”
The project focuses on the effectiveness of the School of Medicine’s family leave policies and practices. Our interventions have included workshops, presentations in grand rounds, publication of a brochure and faculty development articles, and an ongoing faculty survey, all of which have elevated awareness of flexibility policies.
The survey component of our study encompasses male and female faculty members in the schools of Medicine and
Veterinary Medicine, and in the College of Biological Sciences. We compared awareness, usage and satisfaction increases evident in our most recent results against our baseline survey, which showed that faculty awareness and use of these policies in 2010 had been disappointingly low.
Our most recent survey revealed that awareness of flexibility policies demonstrably increased during the past year, including those for child-bearing leaves; reduction of hours or modification of duties to accommodate life changes; tenure-clock extension; and deferral of reviews. Perceived barriers to use
(including overburdening colleagues, and inability to stop work on funded projects) also improved, and we found broad support for the flexibility policies among faculty in all generations.
Some of our findings reveal a need for more focused intervention. Young male and older female faculty members emerged as groups at risk for work-life conflict and resulting career dissatisfaction.
Development of new policies may be required to respond to their needs. We also note cognitive dissonance between desire to use policies and concerns about doing so. Flexible career policies are tools that are commonly used in other industries to attract and retain talent, and have the potential to be equally effective in academic medicine. Such policies must be accompanied by awareness and a supportive culture that encourages their use, so that we may have greater success in faculty recruitment, retention and career advancement.
We urge faculty members to ask their department chairs, managers and the office of academic personnel about leave policies. We plan to continue activities to make our school a welcoming environment for all members of the faculty. Visit http://www.ucdmc.ucdavis.
edu/academicpersonnel/academicleaves/ index.html to view the policies. Please attend one of our future workshops, and participate in our forthcoming surveys.
Amparo C. Villablanca is professor and Lazda Endowed Chair in Women’s
Cardiovascular Medicine; director of the Women’s Cardiovascular Medicine
Program; and associate director of the
Women’s Center for Health.
Lydia P. Howell is professor and chair of the Department of Pathology and
Laboratory Medicine.
TEACHING CONTINUED FROM PAGE 1 professor in the Betty Irene Moore
School of Nursing; and Virginia
Hass, R.N., D.N.P., F.N.P.-C,
P.A.-C, the FNP/PA associate program director, who will head the faculty education aim of the grant.
The training curriculum is being designed to help faculty members refine skills and strategies for retention of minority and disadvantaged students, among whom the attrition rate is disproportionally greater than the student body at large.
The principal objective of the training program is attainment of a 30 percent decrease in student attrition attributable to academic reasons. That correlates to two other Physician Assistant Primary
Care Enhancement Project objectives:
• Impel development of an underserved primary-care rotation to increase the number of FNP/PA students who explore careers in medically underserved communities.
• Stimulate a 30 percent increase in the proportion of FNP/
PA graduates who obtain employment in medically underserved communities.
Bakerjian and Hass are encouraging faculty members not only to participate in the training workshops, but also help develop them.
Planning work is proceeding in consultation with faculty members from the UC Davis School of Education and the Department of Chicana/Chicano Studies. Bakerjian observes that the curriculum will be intended to bolster the cultural competence of faculty members not only in the FNP/PA program, but in all other Schools of Health programs as well.
CONTINUED ON PAGE 5 faculty NEWSLETTER | Summer 2012 | www.ucdmc.ucdavis.edu/facultydev 4
TEACHING CONTINUED FROM PAGE 4
“The UC Davis Schools of Health certainly have focused individually on interdisciplinary education and an interest in improving educational processes, but this workshop provides one of the first opportunities to offer this curriculum throughout the Schools of Health. In particular, we are excited that we will be able to improve knowledge at both the educator and student levels,” Bakerjian said.
The curriculum will help elevate awareness of “implicit bias” (also known as “unconscious bias”), described in the
October-November 2010 edition of the
Faculty Newsletter (click the “newsletter” tab at http://www.ucdmc.ucdavis.edu/ facultydev/).
“Because of implicit bias, the tendency is for faculty to project student failure onto students – that is, focus on student deficits rather than student assets, and think in terms of how the students’ cognitive skills or knowledge must change, rather than how attitudes and beliefs affect students’ learning,” Hass said. “Science and medical education curricula are traditionally content-driven and skillsbased. While content will continue to be an important aspect of curriculum, our faculty development workshops will concentrate on bringing those unconscious biases to the surface and shifting faculty focus toward culturally nuanced learning and teaching in the context of that curriculum.”
The initial phase of workshop development is a needs assessment to identify approaches by which faculty members can improve support, education, retention and graduation rates of culturally diverse and disadvantaged students in the
FNP/PA program, the School of Medicine, and the School of Nursing. The needs assessment, discussions with collaborators from the Schools of Health, and models used by other educational programs will influence the content and structure of the training sessions.
The workshops, participation in which will be free of charge, likely will be conducted in a discussion and case-based setting.
“Participants will be expected to
‘go forth’ and share with others in their departments what they’ve learned, so we’re looking for broad cross-representation from Schools of Health faculty,” explained
Devin Rifkin, CCRP, the program’s project coordinator in the Department of Family and Community Medicine. “In addition to the workshops, we plan to conduct focus groups with current students who may be at risk of withdrawal or dismissal as a result of academic or clinical difficulties they are encountering. Our hope is to identify trends and patterns related to the difficulties they are having.”
Rifkin said that the strategies developed through the curriculum will be useful in enhancing student support services for culturally diverse and disadvantaged students.
“These services will be delivered both in the classroom and through online platforms,” Rifkin added. “The paramount goal is to enhance the knowledge and skills of faculty in working with culturally diverse and disadvantaged students.”
Although the HRSA grant does not include a specific research component,
Bakerjian and her colleagues will conduct evaluations of faculty and student knowledge before and after the interventions.
“That information will inform how we move forward with this program,” Bakerjian explained. “We will disseminate our outcomes and processes along the way, internally to our faculty colleagues and externally through professional conferences.”
Bakerjian welcomes broad faculty participation in planning and enrollment in the workshops, the first of which likely will be presented during the coming fall quarter.
“We hope that faculty who are either experts in this area or want to know more about how to improve the educational process for culturally diverse and underserved students will participate in the workshops,” she said.
“We really encourage wide participation, and we would love to hear from you.”
Debra Bakerjian, Virginia Hass and Devin Rifkin hope to elevate awareness of “implicit bias.”
(Photo by Emi Manning, UC Davis Medical Illustration)
T o inquire about the program, e-mail Devin
Rifkin at devin.rifkin@ucdmc.ucdavis.edu or call (916)734-5073.
faculty NEWSLETTER | Summer 2012 | www.ucdmc.ucdavis.edu/facultydev 5
UC Davis Health System
Faculty Development Office
2921 Stockton Blvd., Suite 1400
Sacramento, CA 95817 faculty
NEWSLETTER
Published by the Faculty Development
Office , which administers and coordinates programs that respond to the professional and career development needs of UC Davis Health
System faculty members.
2921 Stockton Blvd., Suite 1400
Sacramento, CA 95817
(916) 703-9230 www.ucdmc.ucdavis.edu/facultydev
Edward Callahan, Ph.D.
Associate Dean for Academic Personnel
Acting Director, Faculty Development
Cheryl Busman
Program Representative, Faculty Development cheryl.busman@ucdmc.ucdavis.edu
EditPros LLC
Writing and Editing www.editpros.com
faculty NEWSLETTER | Summer 2012 | www.ucdmc.ucdavis.edu/facultydev 6
Workshops and other activities
You are invited! We encourage you to enroll in one of the various workshops, programs and events sponsored by the
Faculty Development Office. For more event details and to register, visit www.ucdmc.ucdavis.edu/facultydev/ and click Enroll Online . (Event co-sponsors are indicated within parentheses.) Volunteer Clinical
Faculty members are also welcome and encouraged to attend faculty development events.
July
20 Institutional Collaboration and Team
Leadership (MCLP)
August
7 Breakfast with the Vice Chancellor/
Dean
17 Fostering a Research Program in
Your Department, Unit or Section
(MCLP)
September
21 Mid-Career Leadership Program
Graduation and Evaluation Session
(MCLP)
Save the Date
Oct. 8 & 15: Grantsmanship Seminar
Dec. 13: New Faculty Orientation
Event co-sponsor
MCLP: Mid-Career Leadership Program
Published by the Faculty Development Office
SUMMER 2012
CULTURALLY NUANCED TEACHING
Training program seeks 30% decrease in minority student attrition
Physician assistants and nurse practitioners frequently are the initial and often the main point of contact for medically indigent people in need of health care. Language and cultural barriers that impede access for growing numbers of minority groups have increased the urgency for development of a culturally competent physician assistant workforce that better reflects the diversity of California’s population.
The UC Davis Family Nurse
Practitioner and Physician Assistant
(FNP/PA) Program is taking steps in conjunction with the School of
Medicine’s Faculty Development
Office to improve retention of healthcare students from culturally diverse and educationally disadvantaged backgrounds. The U.S. Health
Resources and Services Administration
(HRSA) has awarded a five-year training grant to the FNP/PA Program to conceive and conduct a training series under the funding opportunity titled the UC Davis Physician Assistant
Primary Care Enhancement Project.
HRSA has committed $20,000 for teaching expenses during the initial two-year grant period.
The project encompasses several study objectives, of which the training program comprises a key component.
Overseeing the grant project are principal investigator Debra Bakerjian,
Ph.D., R.N., F.N.P., vice chair for FNP/
PA programs and an assistant adjunct
CONTINUED ON PAGE 4
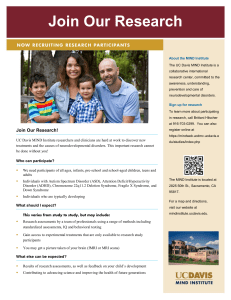
Virginia Hass, FNP/PA associate program director (at left), Devin Rifkin, Physician Assistant
Primary Care Enhancement Project coordinator, and Debra Bakerjian, principal investigator for the project conferred in early June about the training series they plan to inaugurate this autumn. (Photo by Emi Manning, UC Davis Medical Illustration)
TEACHING CONTINUED FROM PAGE 4
“The UC Davis Schools of Health certainly have focused individually on interdisciplinary education and an interest in improving educational processes, but this workshop provides one of the first opportunities to offer this curriculum throughout the Schools of Health. In particular, we are excited that we will be able to improve knowledge at both the educator and student levels,” Bakerjian said.
The curriculum will help elevate awareness of “implicit bias” (also known as “unconscious bias”), described in the
October-November 2010 edition of the
Faculty Newsletter (click the “newsletter” tab at http://www.ucdmc.ucdavis.edu/ facultydev/).
“Because of implicit bias, the tendency is for faculty to project student failure onto students – that is, focus on student deficits rather than student assets, and think in terms of how the students’ cognitive skills or knowledge must change, rather than how attitudes and beliefs affect students’ learning,” Hass said. “Science and medical education curricula are traditionally content-driven and skillsbased. While content will continue to be an important aspect of curriculum, our faculty development workshops will concentrate on bringing those unconscious biases to the surface and shifting faculty focus toward culturally nuanced learning and teaching in the context of that curriculum.”
The initial phase of workshop development is a needs assessment to identify approaches by which faculty members can improve support, education, retention and graduation rates of culturally diverse and disadvantaged students in the
FNP/PA program, the School of Medicine, and the School of Nursing. The needs assessment, discussions with collaborators from the Schools of Health, and models used by other educational programs will influence the content and structure of the training sessions.
The workshops, participation in which will be free of charge, likely will be conducted in a discussion and case-based setting.
“Participants will be expected to
‘go forth’ and share with others in their departments what they’ve learned, so we’re looking for broad cross-representation from Schools of Health faculty,” explained
Devin Rifkin, CCRP, the program’s project coordinator in the Department of Family and Community Medicine. “In addition to the workshops, we plan to conduct focus groups with current students who may be at risk of withdrawal or dismissal as a result of academic or clinical difficulties they are encountering. Our hope is to identify trends and patterns related to the difficulties they are having.”
Rifkin said that the strategies developed through the curriculum will be useful in enhancing student support services for culturally diverse and disadvantaged students.
“These services will be delivered both in the classroom and through online platforms,” Rifkin added. “The paramount goal is to enhance the knowledge and skills of faculty in working with culturally diverse and disadvantaged students.”
Although the HRSA grant does not include a specific research component,
Bakerjian and her colleagues will conduct evaluations of faculty and student knowledge before and after the interventions.
“That information will inform how we move forward with this program,” Bakerjian explained. “We will disseminate our outcomes and processes along the way, internally to our faculty colleagues and externally through professional conferences.”
Bakerjian welcomes broad faculty participation in planning and enrollment in the workshops, the first of which likely will be presented during the coming fall quarter.
“We hope that faculty who are either experts in this area or want to know more about how to improve the educational process for culturally diverse and underserved students will participate in the workshops,” she said.
“We really encourage wide participation, and we would love to hear from you.”
Debra Bakerjian, Virginia Hass and Devin Rifkin hope to elevate awareness of “implicit bias.”
(Photo by Emi Manning, UC Davis Medical Illustration)
T o inquire about the program, e-mail Devin
Rifkin at devin.rifkin@ucdmc.ucdavis.edu or call (916)734-5073.
faculty NEWSLETTER | Summer 2012 | www.ucdmc.ucdavis.edu/facultydev 5
UC Davis Health System
Faculty Development Office
2921 Stockton Blvd., Suite 1400
Sacramento, CA 95817 faculty
NEWSLETTER
Published by the Faculty Development
Office , which administers and coordinates programs that respond to the professional and career development needs of UC Davis Health
System faculty members.
2921 Stockton Blvd., Suite 1400
Sacramento, CA 95817
(916) 703-9230 www.ucdmc.ucdavis.edu/facultydev
Edward Callahan, Ph.D.
Associate Dean for Academic Personnel
Acting Director, Faculty Development
Cheryl Busman
Program Representative, Faculty Development cheryl.busman@ucdmc.ucdavis.edu
EditPros LLC
Writing and Editing www.editpros.com
faculty NEWSLETTER | Summer 2012 | www.ucdmc.ucdavis.edu/facultydev 6
Workshops and other activities
You are invited! We encourage you to enroll in one of the various workshops, programs and events sponsored by the
Faculty Development Office. For more event details and to register, visit www.ucdmc.ucdavis.edu/facultydev/ and click Enroll Online . (Event co-sponsors are indicated within parentheses.) Volunteer Clinical
Faculty members are also welcome and encouraged to attend faculty development events.
July
20 Institutional Collaboration and Team
Leadership (MCLP)
August
7 Breakfast with the Vice Chancellor/
Dean
17 Fostering a Research Program in
Your Department, Unit or Section
(MCLP)
September
21 Mid-Career Leadership Program
Graduation and Evaluation Session
(MCLP)
Save the Date
Oct. 8 & 15: Grantsmanship Seminar
Dec. 13: New Faculty Orientation
Event co-sponsor
MCLP: Mid-Career Leadership Program
Published by the Faculty Development Office
SUMMER 2012
CULTURALLY NUANCED TEACHING
Training program seeks 30% decrease in minority student attrition
Physician assistants and nurse practitioners frequently are the initial and often the main point of contact for medically indigent people in need of health care. Language and cultural barriers that impede access for growing numbers of minority groups have increased the urgency for development of a culturally competent physician assistant workforce that better reflects the diversity of California’s population.
The UC Davis Family Nurse
Practitioner and Physician Assistant
(FNP/PA) Program is taking steps in conjunction with the School of
Medicine’s Faculty Development
Office to improve retention of healthcare students from culturally diverse and educationally disadvantaged backgrounds. The U.S. Health
Resources and Services Administration
(HRSA) has awarded a five-year training grant to the FNP/PA Program to conceive and conduct a training series under the funding opportunity titled the UC Davis Physician Assistant
Primary Care Enhancement Project.
HRSA has committed $20,000 for teaching expenses during the initial two-year grant period.
The project encompasses several study objectives, of which the training program comprises a key component.
Overseeing the grant project are principal investigator Debra Bakerjian,
Ph.D., R.N., F.N.P., vice chair for FNP/
PA programs and an assistant adjunct
CONTINUED ON PAGE 4
Virginia Hass, FNP/PA associate program director (at left), Devin Rifkin, Physician Assistant
Primary Care Enhancement Project coordinator, and Debra Bakerjian, principal investigator for the project conferred in early June about the training series they plan to inaugurate this autumn. (Photo by Emi Manning, UC Davis Medical Illustration)