{QTtext}{timescale:100}{font:Verdana}{size:20}{backColor:0,0,0} {textColor:65280,65280,65280}{width:320}{justify:center}
advertisement
{QTtext}{timescale:100}{font:Verdana}{size:20}{backColor:0,0,0}
{textColor:65280,65280,65280}{width:320}{justify:center}
{plain}
[00:00:00.506]
( Background noise )
[00:00:07.176]
>> Good afternoon, everyone.
[00:00:08.436]
Thanks for turning out on such
a beautiful early spring day.
[00:00:14.896]
We know this reflects your heart-felt
devotion to scientific inquiry.
[00:00:19.966]
And also that some of you were required
to be here, but that's just a small thing.
[00:00:23.686]
My name is Pat Thomas, and I teach health
and medical journalism to Graduate Students
[00:00:28.896]
at the Grady College of Journalism
and Mass Communication.
[00:00:32.026]
And this is the fourth year in a row that
I've been fortunate enough to be able
[00:00:36.046]
to co-organization and co-sponsor Voices
From the Vanguard series in collaboration
[00:00:41.966]
with Dan Colley and the Center For
Emerging Global and Tropical Diseases.
[00:00:46.736]
You know, we have really felt that the purpose
of this series was to bring the world to you,
[00:00:51.666]
I mean, here we are in Athens, Georgia,
and we have been able to bring speakers
[00:00:55.856]
from California, New York Washington,
Boston, even Geneva, Switzerland.
[00:01:01.516]
But you know, there's a lot of the world
that exists in Athens, Georgia as well.
[00:01:06.616]
And although we've never before features
UGA professor, which was a first.
[00:01:12.516]
And as you can imagine since Dan Colley is the
co-organizer of this series it was really hard
[00:01:17.636]
to get him to agree to also be a featured
speaker, but I'm really glad that he did.
[00:01:21.316]
And I'm going to now -- just one
more note I'd like to mention.
[00:01:25.306]
After Dan's no doubt fabulous talk we'll be
moving next door to Dellstanian Hall (Phonetic)
[00:01:32.026]
where as one of my students
says we have the best food
[00:01:35.586]
of any reception that you find on campus.
[00:01:38.246]
So come over, talk to the speaker,
hang out with us for a little while.
[00:01:43.156]
That's immediately following the talk.
[00:01:45.276]
So now I'm just going to welcome
another of my favorite people,
[00:01:48.106]
vice president for research David Lee,
who's going to introduce our speaker.
[00:01:52.586]
[00:01:54.356]
>> David Lee: Well, I made it up the stairs
with no mishap, so that's the good news.
[00:02:06.076]
Actually had to race back here
from Atlanta, had to give a talk
[00:02:09.016]
at the board of regents meeting today.
[00:02:11.726]
But it was important to me to be here.
[00:02:14.106]
Not just to introduce today's speaker,
Dan Colley, although I will do that,
[00:02:20.496]
but also because I really wanted to have
the chance to behalf of the university
[00:02:25.236]
to thank both Dan and Pat for organizing
what I think has been a wonderful series
[00:02:32.626]
over multiple years now.
[00:02:35.166]
It's important, this series, not only because
it exposes students to some of what -[00:02:43.236]
some of the cutting-edge work that's
going on in the area of global diseases,
[00:02:47.026]
infectious diseases, but I think
more importantly than that,
[00:02:52.356]
it really has been a great -- each of
those stories has been a great lesson
[00:02:57.876]
in what a single individual can do to change
the lives of a lot of people around the world,
[00:03:06.876]
given the vision, given the energy and so on.
[00:03:09.796]
And really much as anything, that's
what I've gotten out of these lectures.
[00:03:14.186]
And whether that's helping develop or taking
the lead in developing new malaria vaccine
[00:03:20.246]
as we heard about most recently, or
whether it was starting a foundation
[00:03:24.396]
that is making a difference in terms of
getting people to focus on neglected diseases.
[00:03:29.726]
I think there have been some really
wonderful stories here and I hope -[00:03:33.446]
I hope students have been able to enjoy that.
[00:03:35.876]
I can't think of a more important thing for
a university to do that to provide students
[00:03:41.706]
with those kinds of life examples.
[00:03:44.326]
Okay, so now I'm going to introduce
today's speaker, Dan Colley.
[00:03:48.996]
Dan is one of these guys who's managed
to make a living spending time in some
[00:03:55.506]
of the greatest places on Earth,
and I really hate him for that.
[00:04:00.626]
But maybe that's a consequence of
having grown up in Buffalo, New York.
[00:04:06.246]
Just felt the urge to get away.
[00:04:08.286]
And in fact, as soon as dad
hit 17 he headed south.
[00:04:12.626]
First stop was -- actually,
where was the first stop?
[00:04:18.456]
( Laughter )
[00:04:18.936]
>> Oh, Center College, how could I forget.
[00:04:21.046]
You have that in common with our president.
[00:04:23.106]
Got your -- Dan got his bachelor's
degree at Center College, Kentucky.
[00:04:29.156]
And then headed further south to
Tulane, where he obtained a Ph.D.
[00:04:34.726]
And I think there Dan really trained
as a fundamental immunologist.
[00:04:40.146]
He then made a mistake.
[00:04:42.916]
He headed back north, went
to Yale for a post-doc.
[00:04:47.396]
Didn't last two years up in
the bitter cold of New Haven.
[00:04:50.986]
Decided to make a terrible mistake,
[00:04:53.836]
and this time he headed south
and he didn't know when to stop.
[00:04:57.146]
So he ended up in Brazil.
[00:04:59.316]
And there he spent the better part of a
year, and Dan I might get this story wrong
[00:05:04.316]
because I haven't had a chance
to check it with you.
[00:05:06.116]
But I think you ended up working with some
of the Brazilian federal research entities
[00:05:12.596]
out in the field, so to speak,
working on tropical diseases.
[00:05:18.216]
And it's there where Dan's life-long
love of schistosomiasis really developed.
[00:05:26.386]
And as Pat Thomas would point out, it
was really a fundamental reinventing
[00:05:31.146]
of Dan Colley at this point.
[00:05:33.616]
From fundamental immunologist to
immunologist who was really concerned with how
[00:05:38.256]
to attack a tragic disease that takes a
huge toll on a very large number of people.
[00:05:44.516]
So Dan Colley Version 2, as Pat would
describe, then came back to the states and ended
[00:05:53.306]
up at Vanderbilt as an assistant professor.
[00:05:56.676]
Established his research program,
got NIH funding, did all the things
[00:06:03.106]
that a good professor should do,
working hard to attack this disease.
[00:06:09.406]
Somewhere along the way, and I'm not -maybe we'll clarify this this afternoon,
[00:06:14.536]
Dan decided to go to the Center
For Disease Control and Prevention,
[00:06:18.676]
and he spent nine years there directing
their parasitic diseases group.
[00:06:25.276]
At that point he decided that he wanted to
come back to the university to academia.
[00:06:30.926]
Fortunately, the University of Georgia had
a position, and it was to direct the Center
[00:06:36.736]
For Tropical and Emerging Global Diseases that
Rick Carlton had started a number of years ago.
[00:06:43.896]
So it's a great story.
[00:06:45.096]
We're going to hear a lot more about
it tonight, and I'm looking forward
[00:06:50.326]
to hearing Dan's first-hand stories of how
he got so interested in schistosomiasis.
[00:06:54.586]
Dan, it's a pleasure to produce you.
[00:06:58.516]
( Applause )
[00:07:04.966]
>> I'm supposed to put this on?
[00:07:09.166]
Let me get set up here.
[00:07:14.186]
Thank you very much, David.
[00:07:15.586]
Most of that was true.
[00:07:19.396]
My mother might not recognize some of it, but -[00:07:25.736]
I'd like to start by thanking
the organizers for inviting me.
[00:07:29.396]
( Laughter )
[00:07:31.976]
>> Now this is -- this is a real
honor to be able to speak at home.
[00:07:37.396]
I have no jet lack from doing this.
[00:07:40.356]
This is really great.
[00:07:42.796]
So I would like to first start by doing a little
advertisement about the Center For Tropical
[00:07:50.116]
and Emerging Global Diseases, which some
of you know about, many of you know about.
[00:07:56.916]
But some of you don't.
[00:07:57.996]
And this is the kind of thing that I do at
the start of seminars when I go someplace.
[00:08:03.546]
What we have here at UGA is a
center, an interdisciplinary center
[00:08:08.576]
that has 19 faculty members, or will
when Don Harden gets here in March.
[00:08:15.266]
And the mission is very clear.
[00:08:18.506]
It's to pursue cutting-edge research on
tropical and emerging global diseases
[00:08:23.106]
and train students in this field.
[00:08:25.186]
And we have a number of goals.
[00:08:27.956]
We want to become and remain a preeminent center
for research and education in parasitic diseases
[00:08:35.256]
and other global diseases, and turn research
into medical and public health interventions.
[00:08:42.116]
And to promote global research and
education here at UGA and in Georgia.
[00:08:48.196]
Now some of those goals are more
difficult to attain than others.
[00:08:52.146]
The middle one is really hard.
[00:08:55.246]
Turning research into medical and public
health interventions is a challenge.
[00:08:59.496]
It's a long-term goal.
[00:09:01.586]
But what we do in the center
will take us that way
[00:09:04.906]
if that's the perspective
that we want to put on it.
[00:09:08.966]
We also have a training mission.
[00:09:11.336]
We have five training grants.
[00:09:13.286]
One is a standard NIHT 32 training grant,
and three of them are NIH training grants,
[00:09:21.796]
but they're D 43s from the Fogarty International
Center to train people in other places,
[00:09:28.596]
bring them to UGA, train them where
they are, let them get their degrees
[00:09:33.056]
and things in their home countries.
[00:09:35.486]
And we have one in Argentina,
one in Brazil, an one in Kenya.
[00:09:39.546]
And then we have an Ellison Medical
Foundation training grant that is travelling.
[00:09:45.406]
It is to send our students overseas and to
bring students from overseas labs to ours.
[00:09:51.496]
And we have six different principle
investigators out of the 19
[00:09:55.676]
that have overseas research, in place research.
[00:10:00.406]
Everyone else has their work here.
[00:10:03.246]
But these six have work here and elsewhere.
[00:10:06.806]
And this is just a list of the people.
[00:10:10.116]
And I'm not going to belabor
this, but I think it's important
[00:10:12.816]
to say it really is interdisciplinary.
[00:10:16.356]
We have people in the center from eight
different departments, which are listed here,
[00:10:21.746]
and four different colleges and schools.
[00:10:25.046]
And we come at these diseases
from many different perspectives.
[00:10:30.136]
And I think that's the strength of the center.
[00:10:33.036]
We don't all collaborate one with another,
[00:10:35.626]
we collaborate when it's
convenient and when there's a need.
[00:10:39.236]
But we do know there's somebody down the
hall or across campus that we can draw
[00:10:43.936]
on to get a different perspective
on our own research.
[00:10:47.066]
And I think that's really important.
[00:10:49.356]
So these are the diseases that are studied.
[00:10:53.456]
We have malaria, African
trypanosomiasis, or sleeping sickness.
[00:10:59.706]
Toxoplasmosis, cryptosporidiosis,
cyclosporiasis, shagus disease (Phonetic),
[00:11:05.506]
leishmaniasis, Cysticercosis, schistosomiasis,
lymphatic filariasis, if -- and vector biology.
[00:11:14.776]
Now it's a big list of long names.
[00:11:17.356]
But these are all problems someplace.
[00:11:19.446]
And many of them are actually
still problems in the U.S..
[00:11:22.996]
Some of them are on the bio
defense priority pathogens list,
[00:11:26.666]
some of them are major global health
problems, some of them are focal problems.
[00:11:31.966]
But I'm here to tell you,
you don't want any of them.
[00:11:35.806]
These are not things that you want.
[00:11:38.346]
So these are the kinds of things that we study.
[00:11:41.696]
Now, enough of the ad, we're
going on to schistosomiasis.
[00:11:46.136]
Now, schistosomiasis, as
you could tell by the title,
[00:11:51.206]
is a worm infection that
200 million people have.
[00:11:54.956]
That's a lot of people.
[00:11:57.246]
Now most of them are in Sub-Saharan Africa.
[00:12:01.996]
Some of them, about a million,
are in Asia, maybe 2 million.
[00:12:07.486]
And under a million probably
in South America by now.
[00:12:11.966]
So this is largely a Sub-Saharan
African problem, but not only.
[00:12:16.346]
The worms actually live in the blood vessels.
[00:12:20.046]
So we've heard some lectures
and we'll hear some more
[00:12:23.496]
about soil transmitted helminths
(Phonetic) that live in the gut.
[00:12:27.076]
That's outside the body.
[00:12:29.026]
Come on, that's not a real worm.
[00:12:30.986]
These live inside your body,
in your blood vessels.
[00:12:35.556]
And they live there for a very long time.
[00:12:38.046]
And there's a male and a female,
and they mate, and they make eggs,
[00:12:41.266]
and therein lies most of
the problem we mentioned.
[00:12:45.146]
The global distribution depends on snails.
[00:12:49.596]
Certain snails.
[00:12:51.676]
Don't have the snails, you
don't have transmission.
[00:12:54.476]
But even to a great extent depends on
sanitation or the lack therefore thereof.
[00:12:59.966]
And that's a real problem.
[00:13:01.596]
Some day we won't have this
problem if we have sanitation.
[00:13:05.856]
It's a chronic infection, so these worms can
live in your blood vessels for up to 40 years.
[00:13:10.816]
You know, 40 years.
[00:13:13.766]
The mean life span is probably
more like 7 to 10,
[00:13:17.596]
but they can live for 40
years in your blood vessels.
[00:13:21.196]
[00:13:22.286]
Untreated, 5, maybe 10% of the people who
have it go on to very severe disease and die.
[00:13:30.866]
And they die of messing up your liver, mainly.
[00:13:34.316]
And the blood flow back through
the liver doesn't work,
[00:13:37.166]
and you end up with esophageal
varices, and you bleed out.
[00:13:42.246]
The other 90 to 95% have what's called subtle
morbidity, and we'll mention that in a minute.
[00:13:49.216]
So there's a good drug more
schistosomiasis, it's called Praziquantal.
[00:13:54.046]
It's available, it's not free, like some of the
drugs, to treat neglected tropical diseases,
[00:14:00.466]
but some groups are working on that.
[00:14:02.676]
And Praziquantal is a good drug.
[00:14:04.506]
It cures you.
[00:14:05.856]
The problem in the real world is people
get it again, an again, an again.
[00:14:11.586]
There's no vaccine.
[00:14:13.346]
So we're stuck only with a drug.
[00:14:16.896]
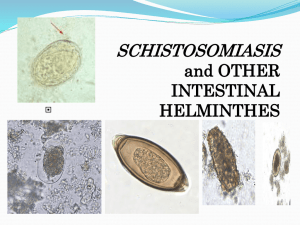
So this is the life cycle,
and it's also the evidence
[00:14:19.446]
for why I'm a scientist and not an artist.
[00:14:22.126]
But if you look at this, it's -- this
life cycle -- I can't -- let's see here.
[00:14:29.926]
See if I can get the pointer to work.
[00:14:31.476]
No, okay. The adult worms, the
pink and blue ones up there,
[00:14:35.456]
the males and the females,
live in the blood vessels.
[00:14:38.456]
And they make eggs.
[00:14:39.896]
And there are three main
species that infect people,
[00:14:42.626]
and those eggs are meant to portray those.
[00:14:46.236]
The eggs have to get out of the
body or there's no life cycle.
[00:14:51.306]
So the eggs get out of the
body in feces or urine,
[00:14:55.136]
depending on the strain,
the species of schistosomes.
[00:14:59.996]
When they hit the water, they have to get to
fresh water, inside, the little embryo hatches
[00:15:05.806]
out of the egg and swims
around looking for a snail.
[00:15:10.026]
Not any old snail, has to be -- not
that snail, a specific kind of snail.
[00:15:16.396]
Each one has a different set of snails.
[00:15:19.196]
Then we reproduce in there asexually.
[00:15:22.376]
So out of one of these mericia (Phonetic) going
[00:15:25.266]
into a snail you might get
10,000 of the next stage.
[00:15:28.906]
This is the mutilative stage.
[00:15:32.016]
So 10,000 of these little
wiggly guys come out over here
[00:15:35.826]
on the left, and they're looking for us.
[00:15:38.936]
They want to penetrate through our skin, we
don't know it, they have a bunch of enzymes
[00:15:43.766]
that help them get through the skin.
[00:15:45.506]
They come in and they migrate around, and
over about five or six weeks they mature
[00:15:50.996]
to adult worms, and you have
the whole thing over again.
[00:15:55.176]
So that's the life cycle.
[00:15:56.856]
And this is what it looks like in pictures.
[00:16:02.306]
So you have adult worms up there at the top.
[00:16:05.336]
They're making eggs over on the right-hand side.
[00:16:09.156]
What's down below I'll show you in a minute.
[00:16:11.476]
But the eggs get out.
[00:16:13.266]
They hatch.
[00:16:13.896]
The miracidium go out looking for a snail.
[00:16:16.306]
Turns into 10,000 of the infectious
stage, and around you go again.
[00:16:21.596]
[00:16:22.996]
So this is what the adult male
and female worms look like.
[00:16:27.106]
They're not very big.
[00:16:28.486]
They can't be very big, they're
in your blood vessels.
[00:16:31.586]
So they're maybe about a half an
inch long and like a piece of thread.
[00:16:36.976]
And there's male -- let's go back here -[00:16:40.206]
there's the male -- this
is technically a flat worm.
[00:16:44.056]
So this flat worm curves up, the male curves
up and forms a groove, and the female fits
[00:16:50.626]
in that groove, and they sit there in your
blood vessels and mate and eat for life.
[00:16:55.886]
40 years. Tough life, right?
[00:16:58.156]
You know, stupid worm.
[00:16:59.726]
Anyway, so the male and the female
form this sort of mating pair.
[00:17:07.006]
And these are just different pictures that
either I've taken or stolen from people ,
[00:17:12.166]
and they show the worm out and
they show the worm in the body.
[00:17:16.126]
And they show it down here in the
left-hand corner is a blood vessel.
[00:17:20.446]
So you can have a lot of these worms.
[00:17:24.676]
Most people don't.
[00:17:26.196]
Up in the left-hand corner is a
picture of 1659 worms that came
[00:17:32.316]
out of a Brazilian 18-year-old boy.
[00:17:34.956]
Because I counted them.
[00:17:36.216]
So I know.
[00:17:36.786]
And a medical student counted them back in 1970.
[00:17:40.726]
So that's a lot of worms.
[00:17:43.106]
Most people don't have that many worms, but we
don't really know how many most people have.
[00:17:49.396]
So this is the situation in
terms of morbidity and mortality.
[00:17:55.926]
Morbidity is when you get sick
and mortality is when you die.
[00:17:59.536]
200 million people infected in the world.
[00:18:02.406]
About 20 million of them, remember
I said 5 to 10%, so we'll say 10%,
[00:18:07.876]
have what's considered severe disease.
[00:18:10.736]
About 100 million have moderate morbidity, or
what's these days being called subtle morbidity.
[00:18:17.816]
Now I maintain that moderate morbidity
is something that someone else has.
[00:18:23.166]
Not you. We don't know how bad this
is, but we do know it's not good.
[00:18:28.046]
And it impedes learning capabilities,
it impedes growth, it has -[00:18:33.596]
you lose a lot of blood in
your urine, things like that.
[00:18:37.856]
And then maybe -- maybe as many as 80
million really don't have any consequences.
[00:18:44.216]
But we don't know how severe those might be.
[00:18:48.106]
If, you know, maybe there's a gradation there.
[00:18:50.926]
So this is what the culprit is.
[00:18:55.436]
So how do you get sick from schistosomiasis?
[00:18:57.456]
You get sick because some of those eggs that
the worm pair makes don't get out of the body.
[00:19:03.566]
They get swept by the blood to your liver.
[00:19:07.226]
And they impact in the liver,
because they're too big to go
[00:19:09.776]
through the presinusoidal
(Phonetic) capillaries.
[00:19:11.906]
So they're stuck in the liver, and your
body says wait a minute, that's not me.
[00:19:17.306]
That's foreign.
[00:19:18.796]
Now why they didn't say that about
the worms is a good question.
[00:19:21.626]
But they say that about the eggs.
[00:19:24.036]
So your body responds and
makes this great big lesion
[00:19:27.706]
up here called a granuloma
around the eggs in your liver.
[00:19:31.546]
And eventually in some people, they go
[00:19:35.216]
on to form what's called peri-portal
fibrosis in the right-hand picture.
[00:19:40.266]
Now what's wrong with that liver?
[00:19:42.656]
It's not in somebody.
[00:19:46.846]
They had to kill -- somebody
had to die to get that.
[00:19:49.086]
And they died because schistosomiasis over is a
long period of time built up a lot of fibrosis
[00:19:57.466]
around the vessels in your liver, and your
blood can't get back up to your heart.
[00:20:03.326]
So that's the real problem.
[00:20:05.176]
It's the response of your own body against
the products of the worm, the eggs.
[00:20:13.776]
So this is an ultrasound picture of somebody
with just beginning peri portal fibrosis.
[00:20:20.146]
And you can see the little -- sort of
donut-like shapes up there and down below here,
[00:20:25.916]
a little bit of banding on the right.
[00:20:28.246]
It's not so bad.
[00:20:30.546]
But it will get worse of the and
it will end up looking like this,
[00:20:35.056]
and your whole liver is blocked off
in terms of returning blood flow,
[00:20:39.026]
and that's the worst scenario in schisto.
[00:20:42.656]
There's another kind of schisto that
doesn't effect your liver so much
[00:20:47.106]
but events your bladder and
your uri-genital tract.
[00:20:50.446]
And if you look at the -- up on
the right-hand side we have a very,
[00:20:56.266]
very old picture that was
taken -- it's simply an x-ray.
[00:21:00.216]
There was no material injected into this person.
[00:21:03.216]
And yet you can see the outline of the bladder.
[00:21:06.306]
That big, almost sort of circular thing.
[00:21:09.696]
If your bladder is calcified like that
[00:21:11.996]
because you have schisto eggs
in it, it doesn't contract.
[00:21:15.726]
Bladders are supposed to go
down and up, down and up.
[00:21:20.496]
This just sits there.
[00:21:22.256]
Which means you have a really bad problem.
[00:21:24.896]
So the three main species are hematobium
(Phonetic), which is what causes this.
[00:21:29.236]
Japonicum (Phonetic), and mansani (Phonetic).
[00:21:31.006]
And they can cause a lot of trouble.
[00:21:34.106]
But this is what it really
looks like in the field.
[00:21:38.026]
What you see in the upper left is
a young man in Cairo who has -[00:21:45.186]
had systemic schistosomiasis, the worst form.
[00:21:48.186]
But what you see on the right lower part is a
picture of kids in a village outside of Cairo
[00:21:56.096]
where the prevalence of schistosomiasis
is about 70%.
[00:22:00.136]
Certainly in this age group, except for that
jerk over there that got in the picture.
[00:22:04.176]
But in this age group it's
basically a 70% prevalence.
[00:22:08.806]
So 70% of those kids have schistosomiasis.
[00:22:12.256]
And one of them is going to get sick
like this kid if we don't treat them.
[00:22:17.256]
I'm not going to spend any time on this,
[00:22:23.236]
but I think it's important to
talk about subtle morbidity.
[00:22:27.546]
There's a guy named Charlie King (Assumed
spelling) who's done a number of studies.
[00:22:30.676]
One of them has really shaken the
schistosomiasis world called Meta Analysis,
[00:22:35.856]
where you bring together hundreds and hundreds
of papers and try to analyze them all together.
[00:22:40.456]
And what Charlie did, and his colleagues did,
was go through all the literature looking
[00:22:48.096]
for measuring, in this case, hemoglobin
in people with schistosomiasis.
[00:22:54.916]
And the -- what you get out of a meta
analysis is called a forest plot.
[00:23:00.016]
And if things are on the left-hand side
of that vertical line, that's not so good.
[00:23:05.306]
And what he found was that people
[00:23:07.416]
with schistosomiasis had
significantly less hemoglobin
[00:23:11.686]
in their blood than did non-infected people.
[00:23:15.506]
Now people where they have schistosomiasis
have a lot of other things too.
[00:23:21.526]
So maybe this wasn't all due to schistosomiasis.
[00:23:25.346]
So the other thing they did was they looked for
other papers, and there weren't nearly as many
[00:23:29.836]
of them, but other papers where they
looked at the change in hemoglobin
[00:23:33.996]
after you treat with Praziquantel.
[00:23:36.616]
And praziquantel will only cure schistosomiasis
and one or two other worms, but not malaria,
[00:23:42.906]
not other things that cause hemoglobin loss.
[00:23:45.986]
And what they found is afterwards you
moved things over to the right-hand side
[00:23:49.886]
of this forest plot, which is good.
[00:23:53.026]
So they came up with this kind of
evidence from a meta analysis that says
[00:23:58.016]
that schisto really has perhaps even a broader
public health impact than the serious disease.
[00:24:05.746]
Now if you have the serious
disease and you're going to die,
[00:24:08.286]
you don't care about the population.
[00:24:10.276]
But if you're talking about public health
the main impact may be this subtle morbidity,
[00:24:15.556]
not just the 5% or so that die.
[00:24:20.526]
So we still have to diagnosis schisto by looking
in the stool and doing -- looking in the urine.
[00:24:27.246]
But these are the eggs.
[00:24:28.646]
The one with the sort of funny-looking spine
on the side is an S-mansonite (Phonetic) egg,
[00:24:33.806]
and the one with the turned-out
spine is hematobium.
[00:24:38.156]
So this is kind of messy.
[00:24:39.716]
This keeps most people out of parasitology.
[00:24:42.466]
I don't know why it didn't keep me out, but
you know, you can make your own conclusions.
[00:24:46.996]
I did toilet train normally,
but -- this is where you get it.
[00:24:54.046]
You get it where it's blue and where
it's green and where it's yellow.
[00:24:59.796]
And one interesting sort of
side fact from this map is
[00:25:05.016]
that in the new world we didn't have
schistosomiasis until the slave trade.
[00:25:09.956]
S-mansonite and hematobium both live in Africa.
[00:25:16.086]
Both came over on the slave trade, but only
one of them established in the new world.
[00:25:21.886]
Only S mansonite.
[00:25:23.116]
There's no hematobium in the new world.
[00:25:25.306]
Came over with the slaves, didn't last.
[00:25:28.206]
Why? We don't have that snail.
[00:25:32.636]
It's snail-specific.
[00:25:34.176]
We have the snails in Brazil
and Venezuela and Puerto Rico
[00:25:38.026]
that can transmit S mansonite,
they just happen to be there.
[00:25:42.846]
But we don't have the right
species to transmit hematobium.
[00:25:46.856]
So it didn't make it.
[00:25:49.476]
So here I am telling you about
the snails, and you know,
[00:25:56.616]
this shows you all the different
kinds of snails.
[00:25:59.996]
Now isn't that really interesting?
[00:26:01.816]
However, I have a friend here who
said wait a minute, wait a minute,
[00:26:06.686]
I -- this is a disease of snails.
[00:26:10.686]
Well, Suzy Sudanica here is right.
[00:26:13.736]
This is a disease of snails!
[00:26:17.986]
They get sick too.
[00:26:19.636]
So I think it's important
that Suzy gets her due.
[00:26:23.806]
So we do have something on here that
says this is also a disease of snails.
[00:26:29.326]
Suzy wouldn't let me get by without saying that.
[00:26:33.626]
So what -- why do you get schistosomiasis?
[00:26:37.116]
Well, we know why Suzy does,
it's the same reason we do.
[00:26:41.026]
Somebody poops in the pond or pees in the pond.
[00:26:45.146]
And you have human, and with one of
the species you have animal reservoirs.
[00:26:52.626]
Water is essential.
[00:26:54.616]
Has to have water.
[00:26:56.326]
You have to have fresh water.
[00:26:57.666]
You have to have fresh water because
that's where these snails live.
[00:27:00.906]
Not this one, but most of these snails.
[00:27:03.206]
You have to have the right snail host,
they have to have some place to live,
[00:27:08.236]
it has to be someplace that
people defecate or urinate.
[00:27:13.306]
Adult worms.
[00:27:16.236]
Adult worms contribute because
they make the eggs.
[00:27:18.676]
And they make the eggs for a very long time.
[00:27:22.736]
So if you're talking about a chronic infection,
you have lots of chances for transmission.
[00:27:28.136]
And that's important.
[00:27:30.236]
But it's a very focal disease.
[00:27:32.226]
So one village may have 60%
prevalence, and down the road 30% or 5%.
[00:27:38.996]
So it's really hard to map out where
you have to go to treat everything.
[00:27:44.526]
So the transmission dynamics look like this.
[00:27:47.126]
You have water, you have
snails, you have people.
[00:27:51.266]
You have people contaminating the
water and people contacting the water.
[00:27:55.486]
You have to have both.
[00:27:57.706]
And when you do in that little
intersection you get great transmission.
[00:28:03.156]
It sounds a little tenuous, but I'm here to
tell you it works really well in the field.
[00:28:08.956]
So how would you attack this?
[00:28:11.686]
Well, sanitation and water and health education.
[00:28:16.486]
That's a good idea.
[00:28:17.956]
It probably doesn't work very well if
you don't give people alternatives.
[00:28:23.156]
The sanitation has to be there or
the clean water has to be there.
[00:28:26.636]
Snail control can work, but the things we poison
snails with also kill fish and other stuff,
[00:28:32.816]
and they wash out, and they're very expensive.
[00:28:36.516]
Hemo therapy is the current control.
[00:28:40.566]
And that means drugs.
[00:28:42.236]
Praziquantal.
[00:28:43.686]
So the current control isn't to stop
transmission, it is to stop people being sick.
[00:28:50.366]
If you give Praziquantal about
once a year to children in school,
[00:28:56.296]
they don't get sick from schistosomiasis.
[00:28:58.746]
Their subtle morbidity is lower,
although it's hard to measure that.
[00:29:04.206]
[00:29:05.576]
So we'll come back to public
health control part in a minute.
[00:29:08.496]
First we're going to just
mention some of the research.
[00:29:11.336]
So as an immunologist there are lots of
fascinating parts about schistosomiasis.
[00:29:15.666]
Lots. This host-parasite relationship has
developed over a very, very long time.
[00:29:21.786]
And I think it's a large amount of hubris for us
to think that we're just going to interrupt it.
[00:29:26.486]
But even if it wasn't a bad disease, which it
is, it would be interesting to an immunologist.
[00:29:34.436]
So what are the major basic bio-medical
research questions about human schistosomiasis?
[00:29:40.626]
Well, we'd like to know what correlates
and what the mechanisms are to resistance.
[00:29:45.896]
There is some resistance, and I
would say show you a little of that.
[00:29:49.156]
What are the correlates and
mechanisms of subtle morbidity.
[00:29:51.966]
We're not sure how to measure it.
[00:29:54.996]
What are the correlates and
mechanisms of severe morbidity.
[00:29:57.846]
Why do 5% get sick and die
and everybody else doesn't.
[00:30:02.246]
We don't know that.
[00:30:03.876]
Does schistosomiasis prevent auto
immune diseases and atopic allergy?
[00:30:08.816]
Well, there's some evidence that that's so.
[00:30:11.376]
Now does that mean everybody ought
to go out and get schistosomiasis?
[00:30:14.786]
No, it means basic scientists ought to
figure out why, and then be able to apply it
[00:30:19.746]
to auto immune diseases and allergies.
[00:30:22.056]
Transplantation.
[00:30:23.736]
If that worm that lives for 40 years, if I could
do that with a kidney, I'd be rich and famous.
[00:30:30.906]
How does it stay in there?
[00:30:32.206]
We don't know that.
[00:30:33.946]
So asking those sorts of questions
in schistosomiasis can shed light
[00:30:38.376]
in other areas of bio-medical research.
[00:30:42.336]
[00:30:44.466]
So what's our lab's current research?
[00:30:47.956]
Well, it takes place in Kenya.
[00:30:50.046]
And we work with a group called Sand Harvesters,
[00:30:54.776]
and another group called Car
Washers and then children in school.
[00:30:58.986]
So these are the three groups.
[00:31:01.436]
The car washers wash cars.
[00:31:04.176]
Well, big deal.
[00:31:06.116]
Down at the car wash -- no, in Tasuma
(Phonetic) that's lake Victoria.
[00:31:12.886]
So they drive the cars into Lake Victoria, in
this case most of them are trucks and vans,
[00:31:17.986]
they drive them in, then they
slosh them down with water.
[00:31:20.326]
And they're standing in the water the whole
time, which is how you get schistosomiasis.
[00:31:26.466]
The sand harvesters are even more exposed.
[00:31:29.066]
They're standing chest-deep with a shovel,
harvesting sand off the bottom of the lake
[00:31:33.676]
into their boat, pull the boat over
to the shore, empty it out by standing
[00:31:37.506]
in the lake and shovelling it on to shore.
[00:31:39.936]
Haggle with somebody about the price,
and then load the dump truck up.
[00:31:44.966]
That's harvesting sand.
[00:31:47.166]
The kids are in school right there, but
they're also in the lake much of the time.
[00:31:52.906]
So Tasuma in the western part of
Kenya, my post-doc and technician -[00:31:58.256]
one of my technicians is there right now.
[00:32:00.666]
I'll be joining them -- I'll be there Saturday.
[00:32:04.716]
Leave Thursday.
[00:32:05.846]
Takes a long time to get to Tasuma.
[00:32:08.036]
So these are the people who
do most of the research.
[00:32:10.616]
We also have field teams -- large field
teams and laboratory teams in Kenya.
[00:32:17.996]
But here we have Carlo Black, Michael
Gallen, and Jen Carter (Assumed spellings)
[00:32:22.906]
who are post-doc gradate
student technician in the lab.
[00:32:27.016]
Evan Seccor is a collaborator left over from CDC
days, and Diana Kurangen and Paula Winsey are
[00:32:33.606]
on site all the time, fortunately,
because I'm not.
[00:32:38.216]
So the epidemiologic question
in the beginning was
[00:32:42.846]
if we treat this guy how long does
it take before he gets reinfected.
[00:32:46.936]
And you can only do that by longitudinal
studies, which have a whole different feel
[00:32:53.356]
to them than everything else I've ever done.
[00:32:56.696]
And what we found by treating these guys,
following them up by doing stool exams
[00:33:03.656]
about every four weeks to see when
they got eggs in their stool again.
[00:33:09.576]
So we did this for years and years, we've
been doing this for 14 years out there.
[00:33:13.266]
Some of these guys have worked
with us for 14 years.
[00:33:17.176]
And in the paper that we published a couple
of years ago, now six years ago in lancet,
[00:33:23.586]
what we found by following these guys
was a little bit surprising to us.
[00:33:28.916]
We found that the time it took for
them to get reinfected differed.
[00:33:33.376]
We thought everybody might be the same.
[00:33:35.366]
We hopped they weren't, but they
turned out not to be the same.
[00:33:39.106]
Some got reinfected quickly,
some got reinfected more slowly.
[00:33:42.986]
Took more cars, and we called them resistant.
[00:33:46.436]
And it was exciting, because the bottom
line here was that when we treated them
[00:33:53.956]
and retreated them because they got reinfected,
retreated them and retreated them, they got -[00:33:59.556]
some of them got more and more resistant.
[00:34:03.036]
And when you do a longitudinal study
[00:34:08.006]
in basic science areas what you find
may or may not ever repeat itself.
[00:34:14.566]
So you've worked five or
six years to get these data,
[00:34:17.366]
then you have to do it all
over again and see if it works.
[00:34:20.606]
Well, fortunately for us, it did.
[00:34:23.206]
And what this slide shows is that some
people have to wash a lot of cars,
[00:34:29.076]
over 450 cars before they get reinfected.
[00:34:31.586]
That's the red line at the top.
[00:34:33.536]
And some people get reinfected
after only about 300 cars.
[00:34:36.856]
And that's the blue line.
[00:34:38.836]
And the number of reinfections
is across the bottom.
[00:34:41.316]
That's a lot of reinfections and retreatments,
but if you do that, some of the people who start
[00:34:47.406]
out low slowly but surely become more resistant.
[00:34:52.986]
And for an immunologist, that's exciting.
[00:34:56.436]
So it did happen again.
[00:35:00.186]
We found what we found the first time.
[00:35:02.226]
And the hypothesis that we work on is that
killing worms is what induces resistance.
[00:35:10.486]
Just having worms doesn't seem to do it.
[00:35:13.366]
But having dying worms in
your blood vessels seems to.
[00:35:17.306]
At least that's what correlates with the data.
[00:35:18.986]
If that's a mechanism or not, we don't know.
[00:35:22.036]
So we proposed that on worm death,
multiple worm deaths over time,
[00:35:30.836]
you end up getting more resistant.
[00:35:33.276]
And we wanted to look at the immune
responses that correlate with that.
[00:35:37.396]
So how do we do this research?
[00:35:40.456]
Okay, you work with the people,
always have to work with people.
[00:35:44.646]
You explain what you're going to do.
[00:35:46.616]
You've already gotten IRB
approval and everything
[00:35:48.946]
for what you do, but that doesn't get it done.
[00:35:51.276]
You have to deal with people, and you have
to convince them to stick their arm out
[00:35:55.356]
and give you blood every once
in a while and to give you stool
[00:35:58.636]
and you may think, yeah, that's cheap.
[00:36:00.596]
It's not so easy.
[00:36:01.956]
So you have to work with people.
[00:36:05.126]
Get their consent, all of that stuff.
[00:36:09.316]
Then you diagnose them for schisto,
other worms, malaria, and HIV,
[00:36:13.996]
because they're all common there.
[00:36:16.446]
And if you don't understand what's going
[00:36:18.886]
on with those you don't know what's
going on with schistosomiasis.
[00:36:22.956]
Then you bleed them, take the
blood back to the laboratory.
[00:36:27.436]
So here we are, bleeding out by the car wash.
[00:36:31.296]
And then going back -- we have regular
laboratory with biological safety hoods,
[00:36:36.396]
you know, cabinets, the whole thing.
[00:36:40.226]
Deal with the blood carefully, because
30% of the car washers have HIV.
[00:36:45.436]
Deal with the blood, put
up cultures, do immunology.
[00:36:50.136]
That's what you do.
[00:36:51.626]
Then you get the data from those
cultures or whatever you're doing,
[00:36:54.526]
the phenotyping by flow cytometry or whatever.
[00:36:57.306]
And then you try to analyze it in
relationship to what you know about that patient
[00:37:02.416]
and what you know about that group of patients.
[00:37:05.016]
And the more you know about them
epidemiologically and background-wise,
[00:37:09.986]
the better you're going to be
able to interpret your numbers.
[00:37:13.066]
Because without that, you just got numbers.
[00:37:16.646]
And then you publish papers
and try to get more funding,
[00:37:20.886]
and each time you try to improve your question.
[00:37:24.506]
That's what this is about.
[00:37:26.666]
So I'm not going to spend any
time on the results of that.
[00:37:30.126]
Just that over the last six years we've been
publishing papers about things that seem
[00:37:37.116]
to correlate or don't correlate with
resistance, and we are still doing so.
[00:37:43.466]
That's why Kara and Hillary
are out there right now.
[00:37:47.326]
And why Jen is trying to figure out an assay.
[00:37:52.286]
Did she finish in time to get here?
[00:37:53.626]
I don't know.
[00:37:54.296]
Anyway, figure out an assay that I
will take out when I go on Thursday.
[00:38:00.256]
So you get all these correlates.
[00:38:02.226]
So what? Well, you publish
papers, you get grants.
[00:38:05.506]
Cool. But that's only part
of why you're doing this.
[00:38:09.666]
This is too much trouble to do just for that.
[00:38:13.316]
So that's a good question.
[00:38:14.806]
So what. What we hope is to learn enough
to form a composite of what is needed
[00:38:22.636]
to really give you substantial
protection against schistosomiasis.
[00:38:28.076]
Because those are the responses that we would
like to engender with a vaccine some day.
[00:38:33.936]
Just any old -- as you heard from Steve
Hoffman if you were here in January,
[00:38:39.326]
just any old response isn't what you want.
[00:38:41.996]
You want certain immune responses.
[00:38:43.946]
So we're trying to define what those immune
responses are that correlate with protection
[00:38:49.176]
so that you can go after those responses.
[00:38:52.556]
And also immunology, as I
said before, is immunology.
[00:38:55.646]
What we learn here are the same mechanisms
that are going on in any immunologic situation.
[00:39:02.216]
Infectious or otherwise.
[00:39:03.626]
And I think that's a very important point.
[00:39:08.216]
So the heart of our research in Kenya
is -- oh, goodness, not that one.
[00:39:13.686]
Yeah, there.
[00:39:14.696]
Transmission sites.
[00:39:16.606]
So we have the children, we
have the sand harvesters,
[00:39:21.106]
we have the car washers,
and we have the village.
[00:39:26.156]
This is what the village looks like.
[00:39:27.566]
Now we only study villages some,
because you can't control it as well.
[00:39:32.366]
You don't know the exposure like we do with
the car washers an the sand harvesters.
[00:39:36.446]
But you can see that the women
are down washing clothes.
[00:39:39.606]
This is what they do.
[00:39:40.936]
That lake has schistosomiasis and
they have the potential of getting it.
[00:39:46.446]
So now we'll put on a different
hat , not as a basic immunologist,
[00:39:51.616]
not as a basic immunologist
doing schistosomiasis,
[00:39:55.536]
but as a global health researcher.
[00:39:58.116]
And someone that's involved in the other end of
what I call the research to control spectrum.
[00:40:05.996]
Now this spectrum or -- we
hope it's a spectrum anyway -[00:40:11.816]
goes from basic research at the
bench all the way to intervention.
[00:40:17.126]
Or you could say bench to
bedside if you're talking medical.
[00:40:22.576]
But bench to intervention if
you're talking public health.
[00:40:25.456]
And what you have are several levels of what
people do to control these kinds of diseases.
[00:40:32.916]
You have control, which is
what we do for schistosomiasis,
[00:40:36.876]
and we're only controlling morbidity by
this annual treatment with Praziquantal.
[00:40:42.226]
You have elimination as a public health
problem, or in a given area completely.
[00:40:47.966]
You have -- and that's the infections.
[00:40:50.996]
Or you have eradication.
[00:40:53.116]
Now we've eradicated small pox.
[00:40:56.216]
We haven't yet eradicated
guinea worm, but we're close.
[00:41:00.956]
We haven't yet eradicated
polio, and it keeps jumping up
[00:41:07.156]
and biting us, but we're still working at it.
[00:41:09.916]
But in parasitic diseases (Inaudible)
is as close as we get to eradication.
[00:41:15.116]
Extinction is when it's gone.
[00:41:17.956]
Small pox is gone.
[00:41:19.426]
It's in a lab -- a couple
labs, hopefully securely.
[00:41:24.456]
So what you do public health wise depends a lot
on what you want to do, what you have the tools
[00:41:30.846]
to do, what you have the public will to do.
[00:41:34.216]
Conceptually, these are very different things,
[00:41:36.936]
and they often get mixed up,
but they're very different.
[00:41:39.916]
So guinea worm is an eradication program.
[00:41:43.296]
Onicacyasis (Phonetic) is a control program,
lymphatic filariasis, which you've heard
[00:41:48.546]
in this series about, is elimination.
[00:41:51.376]
Schistosomiasis is morbidity control, and
that's what we're going to talk about.
[00:41:56.846]
So a few years ago the world health assembly,
which is all the ministers of health from all
[00:42:02.736]
over the world, sat down
in Geneva and decide aid
[00:42:07.356]
that they would pass world health assembly
5419, which is a resolution on schistosomiasis
[00:42:14.726]
and soil transmitted helminths (Phonetic).
[00:42:17.946]
The burden of disease is huge.
[00:42:19.676]
For soil transmitted helminths
it's over a billion people.
[00:42:22.916]
Yeah I know, it's -- in 2009, a billion
doesn't sound like much any more.
[00:42:27.426]
We're talking hundreds of billions
here and there and everything else.
[00:42:30.346]
But 2 billion people is still a lot of people.
[00:42:33.886]
To do these things you really
have to have lots of partners.
[00:42:40.566]
That's probably one of the biggest hurdles.
[00:42:42.946]
But these partners all have to get along,
and they don't all have the same goals.
[00:42:46.736]
Well, they all have the same final answer goals.
[00:42:49.666]
They don't all have the same
reasons for doing it.
[00:42:52.516]
So it's difficult to put these things,
these resolutions, into action.
[00:43:00.146]
And one of the things that we'll talk
about in a minute is operational research.
[00:43:05.716]
Because there's still questions that you have,
even though you have an eradication program
[00:43:10.426]
or an elimination program or a control program,
there's still questions that we don't know
[00:43:15.096]
about that will help that program.
[00:43:19.306]
So this -- about six years ago the Gates
Foundation funded something called the
[00:43:26.036]
Schistosome Control Initiative, or SCI.
[00:43:29.076]
It operates out of Imperial College in London,
[00:43:32.166]
and over the years they have
had 40 or $50 million.
[00:43:37.646]
And what they do is they buy Praziquantal,
they donate that to ministries of health in six
[00:43:44.616]
or eight countries Sub-Saharan Africa.
[00:43:46.666]
And they help the ministry of health deliver it.
[00:43:50.326]
They figure out the organizational needs,
logistical needs, and they help get it done.
[00:43:56.026]
And they facilitated over 50 million
treatments with Praziquantal in that time.
[00:44:01.606]
So that's a lot of treatment.
[00:44:05.256]
And they've dewormed more people
for soil transmitted helminths,
[00:44:08.486]
which kind of goes along
with it, with albendazole.
[00:44:12.666]
So in the countries listed on the
bottom there are country-wide programs.
[00:44:19.226]
And they're in place and they're being shored
[00:44:21.856]
up by this enormous amount
of Gates and now USAID money.
[00:44:25.386]
And that's a good thing.
[00:44:28.496]
Because if we can do it, we should be doing it.
[00:44:31.166]
There are a lot of people
that benefit from this.
[00:44:34.286]
But the Gates Foundation has also
just funded a program here at UGA.
[00:44:39.106]
It's called the Schistosomiasis Consortium
For Operational Research and Evaluation.
[00:44:45.556]
Or SCORE! I left off the
exclamation points on the slide.
[00:44:50.626]
So this is a new program.
[00:44:54.676]
It's just starting.
[00:44:56.816]
It's hectically just starting.
[00:44:59.336]
But it's a consortium to
do operational research.
[00:45:03.806]
Now that's not basic science,
it's operational research.
[00:45:07.576]
It's defined, it's finding out
what control program managers
[00:45:13.366]
in the field need to know
to do their job better.
[00:45:15.936]
And their job right now is handing out pills.
[00:45:19.676]
So part of what SCORE will do will be try
to figure out better ways to hand out pills.
[00:45:26.336]
How we convince people to take these
pills if they don't think they're sick?
[00:45:30.546]
Well, that's a job.
[00:45:33.666]
So it will be run out of UGA but
it will involve investigators
[00:45:38.506]
from around the world through sub awards.
[00:45:40.756]
So there will be a lot of sub awards.
[00:45:44.016]
And I should mention that the president's
venture fund here at UGA gave me some money
[00:45:50.266]
to help me set this consortium in
motion before the Gates came through,
[00:45:54.416]
because that was a huge help.
[00:45:56.026]
Let you travel around and talk to people
rather than do everything by e-mail.
[00:46:02.666]
So SCORE. There were some
ground rules established
[00:46:06.306]
when the Gates called me and
asked if I would do this.
[00:46:09.676]
And they were really pretty
firm about their ground rules.
[00:46:13.366]
Operational research only.
[00:46:15.686]
You know, no amount of wheeling and
dealing with them would make me -[00:46:19.846]
allow me to study lymphocytes
jumping through hoops.
[00:46:23.016]
This is not what they do.
[00:46:24.826]
This is operational research.
[00:46:26.826]
Not basic science.
[00:46:30.086]
We're not supposed to deal with
estraponicum, which is the one in the far east.
[00:46:35.986]
I may have some people on my advisory
board who deal with estraponicum,
[00:46:39.796]
but that's not where the money's going.
[00:46:42.036]
There's no drug development, no vaccine studies,
[00:46:45.456]
and we're to work with existing
control programs.
[00:46:48.036]
Well that makes sense.
[00:46:49.516]
And we're also supposed to work as broadly
as possible with the schisto community,
[00:46:53.326]
which sounds really good until you try to do it.
[00:46:56.076]
Anyway, those are the parameters
that I was given.
[00:47:00.036]
Now all of this is in relationship to mass
drug administration, M D A, with Praziquantal.
[00:47:07.496]
So these will be collaborative studies,
they will be complimentary studies.
[00:47:13.016]
They will be done in relationship
one to another.
[00:47:16.836]
So the -- there are three in the Gates
terminology, there are three objectives.
[00:47:24.406]
Each one has a series of activities below it.
[00:47:28.106]
The first objective is to evaluate alternative
approaches to control schistosomiasis.
[00:47:34.656]
And to eliminate schistosomiasis in
settings with low or seasonal transmission.
[00:47:39.586]
Well, elimination is really, really hard.
[00:47:42.636]
So we'll see about that.
[00:47:44.246]
But the activities.
[00:47:47.106]
The first two activities actually go
together and we'll be having a meeting here
[00:47:51.046]
with about 25 people from
around the world in April to try
[00:47:55.956]
and get a handle to the existing data.
[00:47:58.596]
What do we know works or doesn't
work in control of schistosomiasis.
[00:48:03.276]
So these people are going to come together.
[00:48:05.556]
I sent the letter of invitation
out about two hours ago.
[00:48:10.176]
Third week of April, come together for three
days, and try to sort out what we already know,
[00:48:15.886]
so we don't start trying to reinvent that.
[00:48:20.026]
[00:48:21.336]
The next activity is how do you sustain control?
[00:48:25.826]
Okay, the schistosomiasis control initiative
did a great job in those six countries
[00:48:30.176]
and brought the prevalence way down.
[00:48:32.426]
If you leave and come back in five years,
it will be right back where it was.
[00:48:36.086]
We know that.
[00:48:37.346]
So how do you keep the slope
of return as low as possible
[00:48:42.066]
without spending $10 million every year.
[00:48:46.086]
So we'll be comparing different delivery
systems, and that will be research,
[00:48:50.436]
but it's very practical research.
[00:48:52.816]
The next one will be how do you
achieve real elimination in some place
[00:48:58.396]
that already has low transmission.
[00:49:00.576]
I call this the kitchen sink approach.
[00:49:04.036]
We'll throw everything at it.
[00:49:05.496]
We will do snail control, we will do
latrines, we will do lots of health education,
[00:49:11.056]
and we'll use drugs, and we'll
do everything we can think of.
[00:49:14.406]
Maybe reroute some water ways,
engineering kinds of things.
[00:49:18.416]
And the next one is even a bigger challenge
in that how do you for least amount
[00:49:26.226]
of money get prevalence load from starting
from someplace like that village in -[00:49:32.776]
outside of Cairo that I showed
you that had 70% prevalence.
[00:49:36.196]
How do you get it down, how
do you really get it down.
[00:49:39.546]
And we'll be doing that in relationship
to another series of questions
[00:49:43.526]
that are a bit more basic
science that I'll mention now.
[00:49:47.896]
Oh yeah, we'll also be doing
community health education
[00:49:50.806]
and cost (Inaudible) throughout all of this.
[00:49:53.056]
So the second objective is to develop
the tools needed for global effort
[00:49:58.036]
to control and eliminate schistosomiasis.
[00:50:01.066]
And we have a bunch of activities
that are more on the diagnostic side,
[00:50:05.696]
because we don't have good diagnostics.
[00:50:07.466]
We're still looking at stools, and it's 2009.
[00:50:11.216]
Now come on, we can do better than that.
[00:50:13.166]
So this money will fund some people
to try and do better than that.
[00:50:18.906]
For diagnostics in snails, I guess
Suzy Sudanica gets her day too.
[00:50:23.676]
And in people.
[00:50:25.026]
Because that's one way you
can monitor it in the snails.
[00:50:27.806]
And they're cute, too.
[00:50:30.266]
One of the things that we're going
to have a meeting on even before
[00:50:34.376]
that bigger meeting is we're going to have,
like, five people from around the world who look
[00:50:38.746]
at population structures of schistosomes by
micro satellites, et cetera, come together,
[00:50:43.796]
work out a unified protocol
-- I hear you chuckling -[00:50:47.426]
we will work out a unified protocol
because that's what we'll fund.
[00:50:52.286]
And then we'll be able to look
at the population structure
[00:50:54.956]
about which we know nothing at this point.
[00:50:57.886]
Under mass drug administration.
[00:51:00.106]
Mass drug administration, one
drug -- does this sound familiar?
[00:51:03.896]
Sounds bad.
[00:51:05.206]
Sounds like resistance.
[00:51:07.376]
So we don't know the mechanism
of Praziquantal action,
[00:51:11.316]
so we don't know what to
look for, for resistance.
[00:51:14.346]
But at least if we have a population structure
[00:51:17.116]
under study while we're doing mass drug
administration we may see some changes
[00:51:22.076]
in the genetics of the population that will
give us some clues that something's going on.
[00:51:26.916]
And then we're going to look at subtle
morbidity and try to come up with some outcomes
[00:51:31.476]
that are better than what we have.
[00:51:32.856]
And the third objective is
really simply to try and take -[00:51:37.176]
this won't kick in until like the third
year, where we try to take the findings
[00:51:41.316]
and actually move them into
guidelines at WHO and places like that.
[00:51:48.496]
So the management structure will be
-- there will be three components.
[00:51:52.276]
The sec tear Yacht, which will be myself,
consultant from Atlanta named Sue Binder,
[00:51:58.386]
Charlie King who is the guy who did
that meta analysis, associate director
[00:52:03.396]
for management, and an administrative assistant.
[00:52:06.596]
And then we'll have the technical
working group that will meet every year
[00:52:10.136]
to compare what we're finding, which will be
the 15 or 20 PIs of the various sub awards.
[00:52:16.106]
Then we'll have an advisory group
which I'm just now inviting.
[00:52:19.556]
So how is it going to work?
[00:52:23.476]
We're going to have these meetings, we're
going to select solicitations and proposals
[00:52:29.866]
to do the protocols that
come from those meetings.
[00:52:33.966]
Those will be awarded.
[00:52:34.986]
Then they have to get out the door,
then people will start doing something.
[00:52:41.646]
We'll have annual meetings to
compare what we're getting.
[00:52:45.196]
And it will be a lot of meetings,
that's what a consortium means.
[00:52:52.656]
So very quickly, global health
and global health research.
[00:52:55.626]
Do you know these public health workers?
[00:52:59.496]
Hmm. They're the best-known public
health workers in the world.
[00:53:04.976]
Bono and Bill Gates.
[00:53:07.946]
Global health has changed
enormously over the last ten years.
[00:53:12.426]
And a lot of it is because of these two guys.
[00:53:15.546]
And Melinda.
[00:53:16.486]
Don't leave Melinda Gates out.
[00:53:19.246]
So Senator Arlen Spector said when they
were looking at the FY 2008 budget,
[00:53:26.006]
a healthy world is a good thing for America.
[00:53:29.746]
Health diplomacy must be the
foundation of our foreign policy.
[00:53:34.556]
It's called winning hearts and minds.
[00:53:38.656]
It's called showing your best side.
[00:53:42.326]
So the question for the people in the
audience, especially the undergraduates
[00:53:46.346]
and graduate students and post-docs,
how do I get to work in global health?
[00:53:50.386]
Now I'm going to start by saying how
Dan Colley got to work in global health.
[00:53:56.286]
As David pointed out, I went to
high school in western New York.
[00:54:01.106]
I went to an even smaller
college in central Kentucky.
[00:54:05.376]
I married the right woman who would put
up with all this stuff when I was there.
[00:54:09.726]
Was worth the trip, folks, let me tell you.
[00:54:12.856]
Went to graduate school at
Tulane, in transplantation
[00:54:16.176]
and immunology, and microbiology.
[00:54:18.596]
They actually had a really
good tropical medicine group
[00:54:23.406]
at Tulane then, and I shunned those people.
[00:54:27.606]
They were the ones who dealt
with those yucky worms and stuff.
[00:54:30.606]
You know, they had display cases
full of horrible-looking things.
[00:54:35.766]
We stayed away from them as much as possible.
[00:54:37.546]
And then I went up to Yale and did my
post-doc in very basic science -- very basic.
[00:54:43.146]
I mean, this was before we knew a lot of stuff.
[00:54:47.686]
Then I took a kind of a wiggle,
and I went to Brazil.
[00:54:52.056]
I had this opportunity to go to Brazil
and teach a course in immunology
[00:54:56.636]
and reorganize some research that was going on.
[00:54:58.916]
And the research was in schistosomiasis.
[00:55:00.876]
And I couldn't spell it.
[00:55:02.856]
So I went anyway.
[00:55:04.526]
And I came back to a real job that
I rose through the academic ranks,
[00:55:10.496]
did all those things that
David said in Nashville.
[00:55:13.376]
And then I took another wiggle.
[00:55:16.716]
I'm not really sure why I
did this wiggle, but I did.
[00:55:19.316]
And I went to the CDC, and lo and behold
I was the director of the division
[00:55:24.396]
of parasitic diseases -- not ever having had
an epidemiology course or parasitology course.
[00:55:29.796]
He didn't ask.
[00:55:32.596]
It wasn't like I, you know, lied
to him on my resume, you know?
[00:55:35.816]
And then I came here, for
which I am very, very grateful.
[00:55:42.686]
Because it was time to leave CDC.
[00:55:44.556]
I learned a lot and I had done a lot, and
I was real pleased with my time there,
[00:55:47.926]
but I didn't want to end up there.
[00:55:50.086]
And so Rick Carlton made a
place for me here, and I came
[00:55:55.786]
and I've been living happily ever after.
[00:55:58.806]
So do you see a well thought out path here?
[00:56:04.146]
When someone comes in my office
and wants to know how they can work
[00:56:07.076]
in global health they always
want me to tell them a pathway.
[00:56:11.566]
Well, this one skipped around a bit.
[00:56:14.726]
I don't see a path here.
[00:56:18.326]
So how you get to work in public
health, in global public health.
[00:56:22.696]
What kinds of opportunities are there
for people like you in public health.
[00:56:29.746]
I beg you to remember the continuum, that
spectrum that I very strongly believe in,
[00:56:36.816]
but which is really hard to make happen.
[00:56:39.786]
The spectrum from bench to implementation
and intervention is fraught with problems.
[00:56:47.016]
Not very many people speak the whole language.
[00:56:50.296]
You don't have to speak the whole language.
[00:56:51.796]
You just have to be able to
speak the one over from you.
[00:56:55.076]
At least go out and have a beer with them, you
know, maybe you'll find they're interesting.
[00:57:00.116]
But remember the continuum.
[00:57:01.476]
Because there are things for people to
do all the way along that continuum.
[00:57:06.656]
Whether they're a health economist or a
journalist, even they do global health.
[00:57:14.306]
They actually do a lot for global health,
because without them nobody hears about it.
[00:57:18.906]
So you can do global health whether
you're a basic scientist or an MD,
[00:57:24.066]
or a public health official, or a publicist.
[00:57:28.556]
The whole continuum.
[00:57:32.196]
What education and training do
you need to work in global health?
[00:57:35.226]
It depends on which part
of that spectrum you want.
[00:57:37.986]
Now you may not know which part.
[00:57:39.756]
So cover your bases.
[00:57:41.246]
Now if you want to treat people -[00:57:43.576]
okay, if curing people is your
important thing you've got to get an MD.
[00:57:47.116]
It's against the law to do it if you don't.
[00:57:49.836]
I don't treat people.
[00:57:50.796]
I'm a Ph.D..
[00:57:52.606]
I give people pills to give to
people, but I don't treat people.
[00:57:57.276]
Okay? So if treating people is
important, you go to medical school.
[00:58:01.366]
You do your house staff training,
become a real physician.
[00:58:05.296]
Then you do a fellowship, and you do it in
anything but -- maybe infectious diseases,
[00:58:09.796]
maybe something else, maybe in pediatrics.
[00:58:12.976]
And then you do that research and
things that get you into that.
[00:58:18.436]
Now if you want to do research on global
health issues, you go to graduate school.
[00:58:23.386]
You can do research if you go to medical school.
[00:58:25.766]
No reason you can't.
[00:58:27.826]
But if you go to graduate
school you can't treat people.
[00:58:30.216]
So got to remember those things.
[00:58:32.686]
But you can go to graduate
school in almost anything
[00:58:35.886]
and end up doing global health
-- almost anything.
[00:58:38.996]
It doesn't have to be immunology like me.
[00:58:42.526]
Although I recommend that highly.
[00:58:46.126]
If you want to set policy, well, you
can be an MD, a Ph.D., have an MPH,
[00:58:52.296]
have just experience -- lots
of different things.
[00:58:55.836]
You can work at WHO, you can work at your -you know, at your local health department.
[00:59:00.696]
If you want to teach, depends
on what level you want to teach.
[00:59:04.796]
If you want to teach this stuff, fine.
[00:59:07.556]
We need people to teach this stuff.
[00:59:10.166]
So how do you want to make your
contribution to improving global health.
[00:59:15.206]
You just need to think about all the different
options, and there are a zillion of them.
[00:59:20.106]
So here in the Center For Tropical and Emerging
Global Diseases we try to turn research
[00:59:24.606]
into medical and public health interventions.
[00:59:26.646]
We try to promote global
and bio-medical research,
[00:59:30.106]
and our educational programs here at UGA.
[00:59:35.926]
We in CTG are doing global health.
[00:59:39.516]
And so are a lot of other people at UGA.
[00:59:42.856]
That's the nice thing about this.
[00:59:44.716]
That's actually what makes it fun.
[00:59:48.436]
Takes lots of people with
lots of different talents.
[00:59:51.806]
So (Inaudible) of schistosomiasis,
200 million people.
[00:59:55.566]
They can't be wrong, must be a real problem.
[00:59:57.706]
And it is.
[00:59:59.276]
They live in their blood vessels.
[01:00:01.676]
We can do something for them now.
[01:00:04.516]
We can give them Praziquantal.
[01:00:06.816]
If we just give them health
education, it doesn't help.
[01:00:09.816]
They know the life cycle at
the car wash better than I do.
[01:00:13.616]
They've been doing this for
14 years, some of them.
[01:00:15.356]
They know all about schistosomiasis.
[01:00:16.946]
But they don't have an alternative.
[01:00:19.166]
They wash cars in the lake because
unemployment in adult males in Tasumu is 40%.
[01:00:25.446]
And they have a job.
[01:00:28.326]
So they're going to go in that lake.
[01:00:30.106]
You have to give them an alternative, not
just tell them they shouldn't do that.
[01:00:36.346]
Research is needed, even
in eradication programs.
[01:00:40.426]
If you talk to Don Henderson,
the guy who was the head
[01:00:44.936]
of the global program that got rid of small pox.
[01:00:48.426]
He will tell you that during the
campaign there were findings from research
[01:00:53.226]
that helped them make the final run.
[01:00:56.246]
We need research.
[01:00:57.846]
And the research control
continuum needs to be real.
[01:01:02.416]
Which means people with many
different skills need
[01:01:05.416]
to work together, go out
and have a beer together.
[01:01:09.176]
Talk about what you do.
[01:01:11.726]
Now going to finish up on a couple of
slides that prove that it's not all work.
[01:01:17.776]
This is where I wrote this talk last week.
[01:01:24.566]
[01:01:25.776]
That's Lake Tahoe.
[01:01:26.936]
We're at Hullwood (Assumed spelling),
one of the ski areas around there.
[01:01:30.896]
It's really pretty.
[01:01:33.306]
But this was -- this was about three days later.
[01:01:35.806]
It's also very pretty.
[01:01:37.516]
And you forget if you're from
Buffalo, you should know this,
[01:01:40.636]
but you forget how quiet it is when it snows.
[01:01:43.806]
Good to come home from, though.
[01:01:49.476]
Really, really pretty.
[01:01:51.696]
Now -- now we're out in Kenya.
[01:01:54.346]
These are Kenyan elephants and a
Tanzanian mountain in the background.
[01:01:58.206]
These are the kinds of things that you can
do on the weekend, if you work in Kenya.
[01:02:07.596]
Don't -- this is -- this is the Mara River.
[01:02:11.676]
You should not be like wildebeests and cross
the river in this lower left-hand corner.
[01:02:17.416]
It's not a good place to cross the river.
[01:02:19.466]
Anybody even know what the one in
the lower right-hand corner is?
[01:02:28.446]
Got it. Nailed it.
[01:02:30.156]
Cerval cat.
[01:02:33.116]
Took me lots of trips to Kenya to see that.
[01:02:35.996]
And we have Kilimanjaro on the left, Mount
Kenya on the upper right, the plains of Africa
[01:02:44.496]
on the left, and then that's the sunset
from where I usually stay when I'm there.
[01:02:48.996]
It's a really tough job,
but somebody's got to do it.
[01:02:52.536]
So that's all folks.
[01:02:53.996]
Thank you very much.
[01:02:56.516]
( Applause )
[01:03:05.500]
[01:03:13.360]