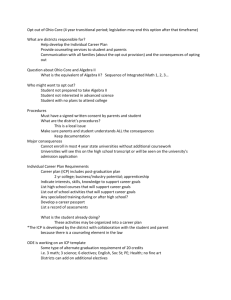
Understanding patient and provider experience and
advertisement

North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Understanding patient and provider experience and communication Yannis Pappas, Agnieszka Ignatowicz, Jessica Jones Nielsen, Athina Belsi, Nikolaos Mastellos, Nicola Costin-Davis, Sue Patterson, Geva Greenfield, Felix Greaves, Matthew Harris May 2013 Contents 1. Introduction .......................................................................................................... 3 Background............................................................................................................ 3 Aims ....................................................................................................................... 3 2. Methods................................................................................................................. 4 Non-participant observations ................................................................................. 4 Focus groups ......................................................................................................... 5 Semi-structured interviews .................................................................................... 5 Semi-structured interviews with providers ............................................................. 5 Semi-structured interviews with patients ............................................................... 6 Provider and patient surveys ................................................................................. 6 Analysis of patterns of communication in the MDGs ............................................. 8 Inter-coder and intra-coder reliability ..................................................................... 9 3. Findings and results .......................................................................................... 10 Non-participant observations ............................................................................... 10 Degree of clarity around governance ................................................................... 10 IT and data collection........................................................................................... 10 Technical measurement issues ........................................................................... 10 Buy-in and sustainability ...................................................................................... 11 Provider perceptions and experiences of ICP implementation ............................ 12 Appropriateness, quality and effectiveness of ICP interventions ......................... 15 Sustainability of the ICP....................................................................................... 22 Patient perceptions on provision and continuity of care ...................................... 24 Provider survey .................................................................................................... 29 Patient survey ...................................................................................................... 32 MDG communication ........................................................................................... 35 5. Discussion .......................................................................................................... 37 References .............................................................................................................. 42 Appendix 1: Patient survey ................................................................................... 43 Appendix 2: Professional survey.......................................................................... 45 Appendix 3: Patient interview guide ..................................................................... 47 Appendix 4: Professional interview guide ........................................................... 49 Appendix 5: Professional focus group protocol ................................................. 51 The North West London Integrated Care Pilot is a large-scale, innovative programme designed to improve the coordination of care for people over 75 years of age and adults living with diabetes. A team of researchers from Imperial College and the Nuffield Trust was engaged to carry out evaluation of the first year of the new integrated care programme. This is a report of Work Programme 4 only. This report forms one chapter of the wider evaluation report which consists of four separate work programmes. Work Programme 4 was undertaken by Imperial College London. All four work programmes and a summary of them can be downloaded from www.nuffieldtrust.org.uk/publications/evaluation-nwlondon-icp 2 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 1. Introduction Background Integrated care pathways have long been advocated as a means to improving provision and continuity of care, as well as promoting interdisciplinary working. A more integrated health care system is thought to: provide greater continuity of care; care is organised across levels and settings, involving several professionals working together as an extended team reduce barriers for patients and offer faster access; care is redesigned so that patients flow through the system, removing artificial barriers and speeding up the patient journey reduce the number of visits to hospital; care is delivered in one-stop clinics with a range of professionals from several disciplines all working together within one co-ordinated system improve work processes for professionals; information flows better between providers and levels of care, through using interoperable systems and shared guidelines (Curry and Ham, 2010; Kodner and Spreeuwenberg, 2002). The overall success, not only of the North West London (NWL) Integrated Care Pilot (ICP), but also of future initiatives of integrated care, depends on several conditions, including the development and implementation of: a) appropriate pathways that support the seamless delivery of care and enhance patient experience; b) re-organised work processes that support interdisciplinary work, facilitate workflow between and within levels of care and create a richer professional experience; and c) delivery models that work for both patients and providers. At a practical level, the ICP involves three key interventions: the IT tool, the patient care plan and the multidisciplinary groups (MDGs). The IT tool facilitates the care planning, sharing of patient information between providers, and enables the stratification of patients with respect to their underlying condition and their estimated risk of hospitalisation. The aim of the patient care plan is to define multidisciplinary pathways incorporating both health and social care to assess the users’ needs in a single-point process and also to enable better monitoring of patients. Finally, the MDGs convene to discuss patient cases and comprise of GPs and representatives from the acute, mental health and social care trusts. MDGs are seen as key facilitators of integration, as moving from individual to multidisciplinary decision making, and from a focus on individual patients to a focus on patient groups, is the ICP’s overall objective. MDGs are opportunities for participants to discuss, reflect on and develop strategies to change systems and processes within the local health economy. Therefore, communication in the MDGs is important to cultivating an integrative model of working, such that communication patterns may be useful to describe how the MDGs are working. Although the effectiveness of the above interventions is key to meeting the ICP’s immediate objectives, sustainability of integration requires careful planning facilitated by realistic incentives, increased awareness and comprehensive costing. To ensure that the proposed model is feasible and sustainable, it needs to be able to address significant challenges and maximise limited resources to obtain better value for money, while improving the quality of health care and patient outcomes. To improve the sustainability of the ICP, it is important to understand the experiences of patients and professionals. Aims The overarching aim of this work package was to investigate the human perception, experience and involvement of providers and users in the ICP. To achieve this, we employed a mixed method 3 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 approach to understand: the patients’ perceptions of provision and continuity of care; the providers’ perceptions of the implementation and sustainability of the ICP; and the patterns of participant communication during MDGs – one of the key interventions of the ICP. 2. Methods In addressing these broad themes of investigation, we employed a mixed methods design drawing from five techniques: non-participant observations, interviews with participating providers and patients, focus groups with providers, surveys, and analysis of communication patterns in MDGs. The techniques are summarised in Figure 1. METHODOLOGY Figure 1: Summary of methods Non-participant observations IMB, weekly provider meetings, various ICP committees Focus groups with providers 4 focus groups with providers Interviews with professionals and patients 25 providers 25 patients Survey 200 providers 2,029 patients/users* *(sent) Analysis of patterns of communication in the MDGs 4 MDGs audio recorded 23 case discussions coded Non-participant observations Non-participant observations of various ICP committee meetings were conducted between early September 2011 and April 2012. We observed the proceedings of the following meetings: Integrated Management Board (IMB) (three meetings) Operations Team (five meetings) Performance and Clinical and Education (seven meetings in total) MDGs (10 meetings). The observations constituted a first level of understanding, which provided us with early lessons on implementation and visions of success. The observations were used to inform the design of the interview and focus group guides, as well as the survey questionnaire. 4 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Focus groups Four focus groups were conducted in total each lasting approximately half an hour. Three were undertaken with MDG members and engaged a mix of professionals including GPs, consultants, practice and community nurses, mental health representatives, social workers, and primary and secondary care managers. They provided rich data due to the open interaction with the researcher and other members of the group and facilitated spontaneous discussion amongst different ICP providers (Powell and Single, 1996). Following Krueger and Casey (2000), the focus groups were facilitated by one moderator using the discussion protocol (see Appendix 2) and sometimes accompanied by other members of the evaluation team. A minimum of three professionals were present (each from a different professional group) and a maximum of six at each session. One focus group was held with the MDG managers and the Operations Team. The focus group discussions were recorded after informed consent was given by participants and recordings were transcribed verbatim by a professional company. Transcripts were analysed using deductive (themes identified from the group discussions themselves) and inductive (themes grouped by those already identified from early analysis of the interview transcripts) approaches (Fereday and Muir-Cochrane, 2006). It had originally been intended to undertake the focus groups as an information gathering exercise to inform the content of the one-to-one interviews with providers. However, logistical complexities of arranging the groups meant they were delayed and undertaken in parallel with the interviews and so they were analysed in tandem. As a result, the opportunity arose to shape the focus groups to compliment the interview content and enrich the interview analysis by deepening our understanding of the analysis relating to key drivers of the evaluation, into understanding professional experiences overall. Semi-structured interviews We conducted 50 semi-structured interviews with a purposive sample of providers and patients between March and June 2012. Semi-structured interviews with providers We contacted 75 providers via email and/or telephone and invited them to take part in the interview. The 25 providers we interviewed included GPs, practice nurses, community matrons, mental health representatives, social workers and practice managers. All interviews were conducted in a private space. Thematisation of questions and probes for the interview plan emerged from three sources: a) the relevant literature; b) previous non-participant observations; and c) our experience and involvement in interventional and public health. The questions were designed to support the development of an understanding of structure and process of the ICP with a view to exploring the ways in which the three interventions of the pilot promote integration of care and, ultimately, efficiency and improved patient outcomes. A copy of the professional interview guide can be found in Appendix 4. Interviews were voice-recorded and transcribed verbatim. Analysis of data was thematic, using a constant comparison (Glaser and Strauss, 1967) within a modified framework approach (Ritchie and Spencer, 1994). The analysis of the interviews was supported throughout by analytic workshops where a multidisciplinary team of researchers consisting of social scientists, medical doctors, public health consultants, nurses and social care specialists reviewed the thematic categories. Thematic saturation was reached quite early in the analysis. 5 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 The findings from the providers’ interviews were organised and written up around the following key ICP areas: 1. Provider perceptions and experiences of ICP implementation and sustainability with an emphasis on organisational and governance issues. 2. Appropriateness, quality and effectiveness of ICP interventions (patient care plans, IT tool, multidisciplinary groups). As described in the earlier section, findings from the analysis of focus groups complemented the interview content and broadened the analysis of providers’ perceptions and experiences with regards to our key areas of analysis. Semi-structured interviews with patients We also recruited 25 patients, who were contacted via the ICP Patient and User Committee and several GP practices. In the former, patients were approached at the end of a committee meeting, informed about the study and invited to an interview. We also asked practice managers to identify patients who were registered with the ICP and invite them to have an interview with us. We employed this indirect recruitment approach because we did not have access to the patients’ demographic data and therefore their addresses. The interviews took place at the Reynolds Building in the Charing Cross Campus of Imperial College. The participants were people with diabetes, people over 75 and some fell within both categories. Although the semi-structured interview guides were designed to explore the patients’ perceptions on provision and continuity of care in the ICP, the variable degree of awareness that the patients showed around the pilot steered the interviewers to explore the patients’ views of overall quality of care. A limitation of the method is that the qualitative data collected through the semi-structured interviews represent the perceptions of a non-randomised sample of patients and providers. For example, we acknowledge that those who decided to talk to us may have been driven by either positive or negative experiences with the ICP. In the absence of a randomised sample of participants, we cannot exclude this bias. Provider and patient surveys Two structured, five-point Likert-scale (1=strongly disagree to 5=strongly agree) questionnaires were developed to assess patient and provider experiences of the ICP. Provider questionnaires explored issues such as the perceived impact of the ICP on patient care and inter-professional working; but also included questions specific to themes raised from non-participant observations, to ensure that the survey reflected the challenges faced by various providers during the implementation stage. Patient questionnaires examined, amongst others domains, the perceived impact of the ICP on patient care, provider-patient relationship and patient involvement in care planning (Appendix 1). Two hundred professional questionnaires were disseminated at the beginning of MDG case conference meetings that took place between April and June 2012. Attention was taken to avoid response duplication and maximise representativeness by selecting meetings from different MDGs (i.e. Hammersmith & Fulham, Kensington & Chelsea, Acton, Chiswick, Central London Healthcare). Overall, 51 professional questionnaires were returned giving a response rate of 25.5%. The majority of respondents were GPs (n=31) followed by consultants (n=5), social workers (n=4), community nurses (n=2) and pharmacists (n=2). This is explained by the 6 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 prominent participation of GPs in the MDG meetings compared to other healthcare providers. Figure 2 shows the relative representation of various professional areas. Figure 2: Distribution of participants according to their professional role GP Social worker Medical consultant 4.26% 4.26% Community nurse Pharmacist Other 6.38% 10.64% 8.51% 65.96% Also between April and June 2012, 2,029 paper-based, self-completed questionnaires were sent to randomly selected patients across all ICP areas in NWL, who had consented to participate in the pilot. Four hundred and five (405) valid patient surveys were returned, giving a response rate of approximately 23%. Another 67 questionnaires were returned with only demographic data and no responses to other questions. Figure 3 shows the distribution of participants per patient group. Most respondents were people over 75 years old without diabetes (n=184), nearly 32% were people with diabetes under the age of 75 (n=127), and approximately 22.5% were over 75 with diabetes (n=90). Questionnaires were analysed using the Statistical Package for Social Sciences (SPSS) version 19. Items were scored from 1 to 5 and were reverse-scored when negative questions were asked. Descriptive statistics were used to outline the relative proportion of providers and patients who were (dis)satisfied with different aspects of the pilot as per each item on the questionnaire. In addition, the analysis involved cross-tabulation to determine whether the scores for each item varied across different professional and patient groups. As a result of the low participation of nonGP respondents, professional groups were merged into two main categories: GPs and non-GP providers. Figure 3: Distribution of participants per patient group 31.67% 22.44% Over 75 with diabetes Over 75 only Diabetes only 45.89% 7 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Analysis of patterns of communication in the MDGs In this qualitative component, we included an analysis of patterns of communication in MDG meetings, looking at the type of conversations between participants and assessing who dominates. MDG meetings involve the participation of GPs, hospital consultants, community and social service professionals each from different organisations within the local health economy and are therefore different to MDGs within hospital settings. We explored whether traditional power relationships and communication patterns exist and persist, or are broken down leading to a more integrated way of working between the professional groups. Did the discussion of the complex clinical cases brought to the MDG meeting lead to or foster opportunities to consider the wider health economy and ways to improve and identify efficiencies in and between participants’ respective organisations? The method involved recording and transcribing MDG meetings and coding the utterances that occurred. More specifically, we conceptualised the utterances recorded in MDGs according to three mutually exclusive domains which we call the Valence, Level and Focus. Although they are distinct from each other, when used in combination provided us a ‘three-dimensional’ view of the meeting with respect to, what we posit as its ‘integrative potential’. For the Valence domain, we draw on Bales (1950) and aggregated utterances that were indicative of solidarity, tension release, agreement, and the giving of suggestions and opinions as ‘solutions’; forward-facing and problem-solving, and therefore likely to improve integration between participants. Conversely, utterances that indicated antagonism, tension, disagreement, or seeking of suggestions and opinions were coded as ‘problems’ – at best these kinds of utterances raised questions and at worst hinder collaborative working. We coded the simple giving or requesting of orientation as ‘information’. For the Level domain, we coded utterances that pertained to individuals, patients, providers and patient care as ‘individual’; to groups of patients or providers as ‘collective’; and to services and organisations as ‘systems’. For the Focus domain, we coded utterances that bear an indication of reflection, or reflexivity on the part of the speaker as ‘abstract’ and those that did not as ‘concrete’. We aggregated the three codes for each utterance into an Event Code, of which there were 18 permutations (Table 1). We posited that Solution Valence has a greater integrative potential than the Information Valence, which has a greater integrative potential than Problem Valence. We also posited that System Level has a greater integrative potential than Collective Level, which has a greater integrative potential than Individual Level. Finally, we posited that Abstract Focus has a greater integrative potential than Concrete Focus. We ordered these permutations into an average weighted ordinal scale. Table 1: Weighted ordinal scale of integrative potential with domain permutations with examples of utterances. Utterance I reckon these meetings will help us to decrease admissions I had the impression the trust will roll it over to the next financial year This would probably help our communication with them a lot The GPs write better quality letters than one would expect Have you considered whether Metformin would be more appropriate? It’s probably because the hospital needs the income Level System Valence Solution Focus Abstract Av Weighting 2.00 System Information Abstract 1.69 Collective Solution Abstract 1.69 Collective Information Abstract 1.65 Individual Solution Abstract 1.65 System Problem Abstract 1.65 8 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 It’d help if the MDG meetings were held on a monthly basis We’ve often wondered whether it’s because they communicate poorly The patient’s HbA1c of 7 is surprising, really Last year, the hospital was £3million in debt We should send the letters direct to the diabetologists The hospital is screwing things up terribly! The referral letters are written by the GPs In this case, Metformin would be a better choice of drug I’m really not sure whether we are treating this patient appropriately Diabetologists in general fail to impress This patient is 49 years old and has diabetes Your treatment of the patient was appalling! System Solution Concrete 1.48 Collective Problem Abstract 1.47 Individual Information Abstract 1.47 System Information Concrete 1.45 Collective Solution Concrete 1.45 System Problem Concrete 1.41 Collective Information Concrete 1.41 Individual Solution Concrete 1.41 Individual Problem Abstract 1.30 Collective Problem Concrete 1.23 Individual Information Concrete 1.23 Individual Problem Concrete 1.06 Full verbatim transcripts were obtained within a week after the meeting from a certified medical transcribing company under strict confidentiality, which were then quality assured. We divided dialogue into utterances or units of meaning, of approximately equal length (Gee, 1999) and coded according to the speaker type and the integrative potential of the utterance. We generated a standardised weighted mean representing the integrative intensity of the discussion at each time decile within each case discussion. As case discussions always began with a presentation of an individual case, we explored whether during the discussion the group progressed to ‘higher’ levels of abstraction, discussing issues shared and common to similar cases and, furthermore, issues shared and common to all participants and their organisational domains. Inter-coder and intra-coder reliability Inter- and intra-rater validity using Kappa scores – a statistical test that determines whether there was sufficient agreement beyond that which would be expected by chance – showed excellent agreement between and within the two coders (Table 2). Table 2: Agreement, Kappa, Prevalence and Bias adjusted Kappa and Kappa max. L=Level, V=Valence, F=Focus, E=Event Code Agreement % A1 vs B1 A1 vs A2 B1 vs B2 A2 vs B2 Kappa PABAK Kappa max L V F E L V F E L V F E L V F E 79.1 73.0 72.2 50.4 .552 .496 .468 .369 .762 .692 .583 .477 .794 .903 .883 .724 74.8 77.4 78.3 46.1 .527 .555 .532 .320 .712 .742 .674 .431 .886 .829 .720 .736 81.7 84.3 80.9 57.4 .587 .700 .639 .446 .792 .821 .713 .551 .903 .900 .902 .796 73.9 79.1 73.0 48.7 .501 .575 .428 .340 .708 .762 .596 .456 .784 .982 .742 .765 9 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 3. Findings and results Non-participant observations Non-participant observations of ICP meetings were conducted between September 2011 and April 2012. The observations constituted a first level of analysis, which provided us with early lessons on implementation and challenges; this was used to inform subsequent interviews, focus groups and questionnaires. Observation of the meetings demonstrated a number of themes that appear to cut across the different groups, whether they were strategic planning meetings or considering the actions of the ICP at the frontline. In particular, the issues of accountability, measurement of success, IT performance, and sustainability appeared on multiple occasions and across all of the settings. Degree of clarity around governance Many participants have discussed accountability, particularly the uncertainty that comes from working across some traditional boundaries of the healthcare economy. Committees have been working out their own levels of accountability and autonomy, and deciding what decisions to make internally and which to pass up to the board. There is a common concern about swamping the IMB with too much information. There are also questions of accountability and oversight for the ICP overall, including arrangements for formal audit processes. These have been openly discussed and have been consensually agreed over the year: ‘Should we be sharing all of this with the IMB?’ (Member of Finance and Performance Committee) IT and data collection Management of information via the purpose-developed IT tool – a central intervention of the pilot – was also a topic that reverberated around the various groups observed. Although there was a common desire for innovation in IT, and a hope that the tool could provide a valuable solution to issues of information sharing, there have been continuing concerns expressed about the performance of the new tool in practice. This issue has manifested itself in several forms, ranging from the experiences of frontline clinicians using the tool – in particular with regards to the problem of integrating the tool with existing electronic patient records – to the negotiations of the ICP team with the IT providers. Some participants at the frontline have expressed a sense of impatience at the continuing failure to get the data collection systems right, and the lack of communication around it: ‘The data’s not coming through in the extract’ ‘There’s a feeling in [Named GP group] that people aren’t communicating enough’ ‘We’ve had some quite painful conversations about getting the data refreshed’ (Members of the Finance and Performance Committee and the Operations Team) Technical measurement issues There are some unresolved issues with regard to the technical nature of measurement of activity and, in particular, exactly what outcomes should be measured. Setting the ‘baseline’ of performance prior to the start of the pilot has proved to be a difficult undertaking, particularly as the pilot progressed. Several participants commented on the fact that although key overall aims 10 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 were set at the start of the project (such as an improved clinical quality and reduced admissions and costs), there was comparatively little agreement initially on how to measure the impact, and what to compare the change against. There has also been debate about who should be setting the performance metrics – the evaluation team, the finance and performance committee or the clinical and education committee. The debate took place in a collegiate and constructive atmosphere, but there was a frequent suggestion that these metrics should have been more clearly defined at the start of the process. ‘A year for evidence of success is academically flawed’ ‘How do we tease out the other real world phenomena happening at the same time?’ ‘We need to nail the baseline now’ (Members of the Finance and Performance Committee and the Operations Team) Buy-in and sustainability Many discussions across the various committees and meetings were related to the scale, buy-in and sustainability of the pilot. Initial concern focused around recruiting sufficient numbers of participants to the pilot. As sign-up of participants to the pilot increased over the second half of the year, and the pilot began to increase in size, the focus changed to how sustainable the intervention would be as it scaled up. The nature of the incentives offered to GPs to sign patients up was a particular area of focus – and in particular whether the pilot’s novel incentive payment systems would be tenable in a substantial scale-up. In addition, the buy-in of various professional groups was noted to be variable in some areas, and several groups highlighted the need for constant communication from the centre. The link between the healthcare economy and local government controlled social care was a difficult issue on a number of occasions. ‘There are 304 patients consented’ ‘In total, everywhere?’ (Members of the Finance and Performance Committee and the Operations Team) ‘We’re building up cost pressures for the future’ (Finance and Performance Committee member) In addition, concern has been noted about the variable level of skill and capacity around management functions in MDGs and practices. In particular, these were concerns about MDGs commissioning their own additional services from the pilot budget, how these would be held accountable and how conflicts of interest would be managed. MDGs were keen for the freedom to improve local services, including spending ICP resources. However, there is an unresolved tension of balancing autonomy of local practitioners with control from the centre of the pilot. All committees observed argued for an agenda of, and displayed a genuine commitment towards, transparency around the ICP, its decision-making processes and its approach to conflicts of interest, such as commissioning services from their own practices. ‘MDGs may not yet be mature commissioning organisations’ (Finance and Performance Committee member) 11 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Provider perceptions and experiences of ICP implementation The following sections present the findings of the analysis of interviews and focus groups with ICP providers. The analysis revealed a number of themes which were organised and are presented here as organisational and governance issues, and appropriateness, quality and effectiveness of the three ICP interventions (IT tool, patient care plan and MDGs). Organisation, governance and provider engagement An overarching finding was that the ICP aims extended beyond the overt aims of reduction of hospital admissions, administration of care plans and integration of care. However, the specifics of these were not always clearly articulated. Providers reported that the ICP represents a new, innovative way of thinking and working, and commitment to traditional values, while recognising that many of the established practices need to change and transform in order to improve patient outcomes, staff satisfaction, care models and financial position of the NHS. Most providers agreed that the broad principles of enabling integrated, patient-centric care is a holistic approach to addressing patient needs and are in the right direction and timely. Providers have largely recognised the need for a shift towards preventative, holistic practice where professionals from various levels of health and social care collaborate in a ‘joined-up system’. They told us that because of the fragmentation of care systems, single agencies are not well placed to resolve difficulties inherent in providing the comprehensive care required by people with complex conditions and multiple needs. Collaboration between diverse stakeholders was seen as essential to delivering the desired transformation of the structure and culture of care. The ICP vision of improving patient care through better communication between and within levels of care was largely supported: ‘It’s good to have these ideas. The ideology is good. The aspiration is good … We have to be cautious to get it right, I think, that’s why it’s this commitment’ (Social worker) ‘You know, certainly in London, with diabetes, you can’t have everyone being looked after by a specialist in secondary care. It makes no financial sense, it doesn’t make good medical sense, so clearly you need to be integrated with a level you can fasttrack people up and down the system and access the system when need be’ (Hospital consultant) Commenting on the merit of the ICP’s vision, some providers mentioned that this level of integrated practice should be instilled in all practitioners and in order to transform the culture of care engagement with the principles of integration, it should start in medical schools: ‘I think the broader [aim] is to improve the quality of care that the patients get and to provide a more holistic approach… Because working in the job that I do… I see the end product of poorly integrated care, I see the end product of… I’ll go onto a medical ward and I’ll see somebody whose diabetes is being cared for… So I really see at this end how soiled care has become so… I mean, I think that the main way of addressing that is to get right back down to undergraduates and get them all working together’ (Hospital consultant) 12 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Some of those who have been part of the pilot since the initial set-up and implementation stage demonstrated a feeling of pride and commitment to the programme and its success by commenting on their positive experiences from their involvement, and expressed their sense of ownership over certain aspects of the pilot: ‘I was part of the group that was very first involved with the pilot... I’ve connected with the doctors that ended up promoting it in the whole area, so I sort of… led part of the promotion and spread it around practices... But the reason why I was involved fundamentally was that... I saw that this… could very well be a benefit’ (GP) This dissonance between providers’ expectations and what they perceived as the ‘reality’ of the ICP was mostly articulated in context of the delivery of the ICP in real time and negotiation of budgets: ‘They made you feel that this was all going to be your pilot and anything you wanted would be down to you locally. So they made you feel that you could negotiate the funding that went with it… the minute we first went to the negotiation, all this was completely different’ (GP) Yet, some reported that the rationale of the ICP and its model of integration were not always adequately and explicitly articulated. The result was that key drivers for implementation and evaluation of the ICP and its interventions were ambiguous. ICP providers were aware that there was an intense pressure to achieve, and for the pilot to succeed, but they were confused by what they were to be measured against or what exactly the outcomes were supposed to be: ‘Right at the beginning, I was sort of told, oh get on with it. We didn’t know anything about it [the ICP]’ (Diabetes specialist nurse) ‘I’m confused about what the actual target is’ (Operations manager) The governance and leadership of the ICP was not clear either: ‘I suppose two questions that I would like to know the answer to and I don’t know the answer to is who are the responsible officers of the ICP, and what is its legal entity’ (Hospital consultant) The following narrative is not only characteristic of the alleged lack of clarity of operations and governance, but also of a distinction between sides (implementation team versus health and social care providers): ‘…managing the set-up of it – I think initially there was a lot of confusion from both sides about what was involved and how we were going to get there’ (Secondary care manager) In addition to the lack of clarity of the ICP objectives, there was also a distinct lack of belief of its potential impact overall and the appropriateness of its interventions such as the MDGs: ‘They keep saying this is going to save money but most hospitals have deficits so people don’t go to hospital – and that reduces funding and closure of the wards and hospitals’ (Hospital consultant) 13 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 ‘It is rare to have a major impact on patient care, and I cannot think of any in whom an admission has been avoided as a result of discussion [in the MDG meeting]’ (GP) Conversely, there were narratives on the early phases of the ICP that present operations as quite prescriptive and formulaic. But, over time, this changed for the better and flexibility was introduced that enabled adaptation to local processes: ‘It was very prescriptive to start with. We were told exactly how we should run and how we should do it… it’s a lot free-er, so we can structure it better how we want now’ (Secondary care manager) The sharing of clear objectives and processes of the ICP as well as the establishment of a culture of collaborative working are seen as important drivers for success. In the following interview extracts, a consultant and a manager talk about the lack of an ‘adhesive material’ which would keep the various elements of the ICP together and a lack of knowledge/training of key members of staff who come into contact with patients: ‘I mean, I know the pluses of that system – I’m not, you know, hostile against it, but you can’t just suddenly impose that system without bricks and mortar and have the critical mass of people working together.’ (Hospital consultant) ‘Getting staff to understand what the whole thing was about, and I think still now, you would ask some of our staff and probably they’ve been getting consent and all of that, and they won’t understand fully what ICP is, so they’re not that prepared to answer questions from patients, when they’re contacting patients’ (Primary care manager) Some of the providers that we interviewed mentioned that a strong political impetus, mostly within their respective organisations, was the reason for them to sign up to the pilot. Some interviewees attributed their engagement with the ICP to a momentum of wider engagement in NWL which might have had a political underpinning: ‘The pilot was going ahead anyway… we had reservations about the design and organisation of the project but were told it was the only option, there would be no other investment in primary care that it would look very bad for our consortium if we didn’t take part’ (GP) ‘There is a lot of political impetus behind it. Imperial wants it. Kensington and Chelsea want it... So we decided that politically it would make sense to join’ (GP) ‘It was seen as a bit of a, we’ve got to do this, I’ve got to be honest, and I think our kind of executive is very, is very keen on this. So whether that’s for political reasons or ideological reasons, I don't know, but it seemed to be a very good thing to be involved in. I think for those on the ground, I think we’ve got slightly different views about that’ (Hospital consultant) There was also recognition that in order for the ICP to be successful it would have to reach a critical mass with a number of participating organisations supporting its aims, which were inherently based on wider collaboration: 14 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 ‘We got involved… because it was recommended… the ideas were good and we were all encouraged to sign up, collectively, to make it more likely to be a success and so we came on board’ (GP) Providers began to attribute value judgements to financial incentives and practical arrangements as benefits (or not) of their engagement with the ICP. Even though the majority reported being satisfied with funding arrangements, some providers raised questions about the potential for return on investment. We were told by many that the payment did not reflect the time and effort that needed to be invested in order to achieve the pilot’s aims. Subsequently, this was perceived as clouding the positive experience of providers we interviewed: ‘I simply judge it on how much work it is and what we’re paid for’ (GP) ‘So [person’s name] found a system whereby we break even on the elderly [care plans], right? But break even? GPs don’t really go for it… But the key thing is that, when you look at it, [person’s name] said that you’re really making a loss on it, if you are employing nurses, so you can’t ask GPs to take on something new which is either going to break even or lose them money’ (GP) Appropriateness, quality and effectiveness of ICP interventions This section presents the providers’ perceptions on the appropriateness, quality and effectiveness of the three key interventions of the NWL ICP: MDGs, IT tool and patient care plans. Multidisciplinary group meetings The interviews and focus groups with providers indicated that the participation in the MDG meetings was generally perceived as worthwhile. The MDG members told us that the meetings were valuable to them personally and professionally, facilitating networking, education, knowledge-sharing and best practice: ‘It was very nice to get out of hospital, it was nice to go and meet GPs, put faces to names. It was good to have in depth clinical conversations about complex patients. It was rewarding professionally’ (Hospital consultant) ‘I learnt a lot about diabetes. I don’t remember it all, but definitely my understanding of diabetic issues has improved and I’ve learnt about other services and how they work and what they do and what their remit is’ (GP) The majority of participants expressed a view that having other providers present whilst discussing a patient case was helpful. In addition to finding clinically-related advice of benefit, providers reported that meeting colleagues in person and ‘putting faces to names’ was likely to improve their working relationships: ‘The MDG meetings are the best part of it really... It’s quite nice to meet your neighbouring practices and for them to bring along a clinical case, for us to bring a clinical case, to have just as the name suggests, different people from different disciplines. We did network and we did manage to get few things done this way’ (GP) 15 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Some providers were enthusiastic about their learning from the MDGs, in particular with regards to the services available in the community and locally. The legislation and policies influencing the provision of mental health and social care were also mentioned as having value for providers’ practice: ‘It has made me more aware of the medication aspects, because I glean lots of good pearls of wisdom, coming here, because pharmacy isn’t a major point in nursing … there’s so much to learn and just take note, when I’m taking my history and thinking, oh that will be interesting – I wonder if the GP might change something’ (District nurse) ‘The other thing I’ve found useful is getting to know all the things that are available in the communities … they talk about things I didn’t realise were up and running’ (District nurse) However, in general, providers described their participation and engagement in the MDG meetings as varied. Their positive experience was often conditional and contingent on a number of factors. Some, particularly GPs, told us that they attended meetings regularly. Others, however, mainly consultants, reported being frustrated about having to attend several meetings in different locations, sometimes at very short notice. As the MDG meetings evolved and became increasingly embedded in providers’ practice, the expectations and experiences of providers also changed. Some expressed concerns about the quality of leaning and value for money that the MDGs represented. Single-handed GPs, for instance, were concerned about the opportunity-cost. While recognising that they were paid to attend meetings, many GPs described taking time away from the surgery, as problematic: ‘I’m essentially now a single handed GP here, that’s just... I know we get paid to go, but actually I’m not seeing my patients… it does take quite a lot of time’ (GP) This was also echoed in the interviews with secondary care providers: ‘My trust is paid £100 for every hour that I spend in the MDG meeting. I am scheduled to work 12 hours a week in our community service here. So MDG takes up 20% of that time, or ICP takes up 20% of that time. Now, the trust is funded for that, but we can’t buy in another consultant time for these three hours. You can’t backfill for a short period’ (Hospital consultant) The time implications of attending MDG case conferences were certainly high priority for the providers: ‘No concept of the fact that my diary’s booked up three or four weeks in advance and having a very short notice to attend some MDGs, I think a major concern for me. And completely inexplicable is why they have different MDGs but at the same time on the same day, because I can’t split myself in half’ (Hospital consultant) However, they were keen to express how much the group working had developed, tailored to the local needs and becoming more efficient: 16 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 ‘It’s more clinical now and we even have an education session at ours… people attend more regularly, more willingly now and they do bring cases so we get through a lot more than we ever did at the start and I think that can only be a benefit’ (GP) Some reflected on the balance between being able to confer with colleagues in and MDG to improve care in the future, and the resulting backlog of work that would affect patients directly: ‘It’s the benefit – sitting there and discussing half a dozen patients at a fairly significant cost when you consider all of the people that are resident at the meeting and the 20 patients each one of those clinicians probably would have seen if they were there. It’s the balancing isn’t it – between the two?’ (GP) Some reported that there was still work to be done to make the meetings more efficient and that it would be beneficial to reflect on whether the meetings need be so regular in the future. ‘I definitely think there’s a lot more work to be done in terms of people still bringing more cases and getting through them faster’ (GP) ‘If we could space out the meetings… maybe having meetings once every two months… one of the things we were discussing was having a telephone link or email link at certain times during the week, where if there were an issue that you wanted to raise, having a direct link rather than having to wait until the next meeting’ (GP) The majority of the interviewees reported that are optimistic about the potential of the MDG meetings to improve service delivery and patient outcomes: ‘The suggestions they have are really gold-standard things we should be doing for our patients. And it’s always good to practice to that very high level and it inspires you to practice to that high level on all your patients to be honest’ (GP) ‘And the benefit of it was the fact that you may have six cases discussed. All of those six cases could’ve been one of your patients, you know. This is obviously the whole nature of medicine, they follow similar patterns, so although you only bought one case, it felt like you were talking about six of your patients. So you could make notes and suggestions and apply them to patients that you couldn’t bring. So I think indirectly you could say that that had an impact on admissions, you might like to say’ (GP) However, some providers told us that on the whole, what was happening to the patient remained unchanged, and it is too early for patients to see any specific changes to the ways the care is provided to them. However, they also noted that they had initiated new links with other providers and are now able to resolve issues about specific patients through these new networks: ‘…all this is doing is replacing existing models of care, which I don’t think were working badly. And I think that on the whole… I think… yes, I think on the whole what is happening at the patient level is pretty much unchanged’ (GP) ‘That’s the thing about good integration… when you’re working with your colleagues you know you can drop them an email or you could give them a call on their mobile’ (GP) 17 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 While reports about the value of networking, knowledge exchange and education were prominent, a minority reflected critically on the outcomes of the MDGs and whether they facilitate their indented purpose, which was to facilitate integration of services, a ‘joined-up’ working, which will affect the care of many patients not just the only the ones that are discussed in situ: ‘So you are sitting there a lot of the time and there might be a glimpse of a question around issues regarding vulnerable adults, that way you fit in and then you can offer. It’s difficult really and in terms of social care representatives going there it’s... they will politely say, oh it’s an interesting experience, but for others it’s four hours waste of their time’ (Social care representative) ‘The MDGs were good for the educational element of them, but it was restricted to only one doctor, and that doctor did not share information with the rest of the practice, so it didn’t really alter the behaviour of the rest of the team. And that’s what everybody else in the MDG said, it wasn’t just my practice’ (GP) The IT tool The ICP IT tool was one of the more ambitious aspects of the pilot, seeking to integrate numerous complex systems, services and expertise into one networked system. Not all the providers that were interviewed or part of our focus groups had used the tool regularly, with many delegating relevant tasks to others. It is likely that the importance of the tool and high expectations of its performance are, in part, responsible for the disappointment providers expressed in its failure to deliver: ‘The key aspect of the pilot I thought was vital was the tool to enable good sharing of information across different primary, secondary [and] social [care services] because one of the problems in the past has been the difficulty of getting information for patients moving to the right people’ (GP) ‘Unfortunately that’s something that’s not quite working yet, but I think it is a vital aspect for this project to work well… to have good lines of communication, and that’s why I was hoping the tool itself would help’ (GP) For GPs in particular, the delay in rolling out the system and its underperformance led some to lose faith in it being fit for purpose and disengage with its use: ‘We really need an IT tool that worked to do the care planning. But it took ages to get it up and running. Then it wasn’t working well and we didn’t know how to use it. I lost interest after a while’ (GP) ‘.. it’s like a million tonne super tanker going down – it can’t be stopped… despite countless occasions of trying to get people to see sense this is never going to work – this tool’ (GP) ‘A washout from start to finish. [The ICP] couldn’t be more different to what we were promised… Mars and Jupiter…’ (GP) The providers told us that the IT tool was mainly used to identify the eligible patients and as a means of overseeing the care planning activity. The majority of the healthcare professionals that 18 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 participated in our research believed that the lack of interoperability between providers’ IT systems was a substantial barrier to meeting the ICP objectives. Some also commented on the lengthy process and difficulties of linking health and social care data, while others questioned the IT tool’s impact on achieving the integration between the primary and secondary healthcare providers: ‘So far the entire length of the pilot, the only person who entered any of our patients care plans on the IT tool been either me or one of my colleagues. We’ve never had a message or anybody ever looked at one of our patients’ records. We still operate in the same way so you couldn’t do any referrals properly on the system… made zero impact literally’ (GP) ‘I don’t think that if one of my diabetic patients is going to go to Charing Cross Hospital tomorrow, and check their care plan, and it’s going to tell them anything more than they would already know… It just tells them, diabetes review in three months, or yes, he’s been referred to hepatic screening. Is that really going to change anything?... I don't think it tells us much information as they want, and I don't think any consultant or any doctor has the patience to go through all the entries. They’re not even labelled, so you have to go one by one, to see what it actually is’ (Primary care manager) Providers were frustrated that they were not able to refer patients to services by directly using the tool and were not confident in using it for documenting decisions about changes to a care plan or referral needs. This was an area of stark disappointment, which generated considerable criticism of the tool’s functionality and purpose. Some noted that it created a duplication of work, filling in the necessary aspect of the IT tool for the pilot and then having to separately refer via their existent systems: ‘There was a lot of talk at the outset about being able to internally refer on the tool … so you can tick a box, it sends a referral and you can even have put down in the care plan that you’d like a district nurse to go round to do a competence assessment or DVT assessment or whatever, but then you have to do another referral outside that, because it doesn’t count as a referral, so it’s a duplication’ (GP) The lack of interoperability between the IT tool and existing systems in use is creating extra workload by duplicating tasks such as logging referrals twice: ‘I’m using the template on EMIS, which is our computer system, then just inputting the data onto the IT tool and then having to do separate referrals. So it creates a lot of work, which is fine because you’re being proactive and you’re, you know, identifying concerns that the patient might not say to you, but it does create a lot of work. If it was more integrated – which is the whole point – it would work a lot better’ (GP) The insufficient usability of the IT tool was presented by some as a major barrier for its use. Various problems with graph production, readability and complexity in its use were reported: ‘It’s difficult. The graphs that are produced – you can’t read, and it’s been, to all intents and purposes, a bit of a disaster. I don’t know how much it cost but…’ (GP) ‘It’s a very complex tool to use in a narrow timeframe that … has been operationally laughable at times… and duplication of some other initiatives that are already 19 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 happening … might mean that you’re not fully utilising the tool because we will [do the work] for that patient through another window’ (GP) Frustration regarding the tool’s functionality extended to the information it contained and many felt it was a costly re-invention of existent systems. There was an underlying annoyance and suspicion, reflected in many comments from providers, that the tool had not been developed in consultation with those who were going to use it and that its failure to deliver was a costly exercise; this engendered an overall feeling that this integrated electronic system was not going to work in the long run: ‘It doesn’t have anything like the information that you would have if you were able to [access] our practice to look at the notes … it’s frustrating when you see that this is the line its gone down’ (GP) ‘The problem is the person who wrote this programme obviously didn’t sit down with any decent GP because all the information is on our computer systems’ (GP) ‘They’re now redesigning it, at another enormous cost, and it’s never going to match the computerised data that CPGs have’ (GP) The patient care plan The care planning process received mixed views and was generally perceived by providers as failing to enhance their practice or the care of their patients. Some comments reflected the frustration that the process was an exercise to meet prescriptive targets. Providers often complained that the plan’s format and functionality added to its weaknesses and that it did not correspond well with the MDG case conferences objectives: ‘... and the care packages, which needed to be done in a certain way… we were told that was how we were to do them… it didn’t feel like it was the best way of approaching it’ (GP) ‘From a clinical perspective I think the care planning has actually been quite disconnected from the case conferences… the care plan seems a bit of a chore. It’s a tick box and it’s somehow hard to connect the two together’ (GP) However, many were conscious that working through the care plan was a mechanism that would allow facilitating their consultation with patients and to take a more multidisciplinary and integrated approach to providing care: ‘There’s this sense of – oh my gosh – there’s all of these things which I need to get covered within this consultation because… of our care plans. So that feels difficult but its good, holistic care’ (GP) ‘Actually I’ve got to say as a result of the care plan, some of the patients have come straight from the nurse who does them to one of the clinicians… that’s good’ (GP) 20 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 The patient care plans were also regarded as of value, because they both offered a good way to make sure patients were being proactively monitored, as well as enable GPs to establish a better understanding of patients’ needs: ‘I think that the fact that we were keeping a closer eye on our diabetic patients, the fact that we’re getting in touch with some of our elderly patients that weren’t coming, just to know how they’re doing, even if they’re still doing well. It’s good to know that they’re actually doing well, so that’s been a positive, I’d say’ (Primary care manager) ‘I think this is a really good way for me to get to know my patients. I can’t know every patient, so the patients that sometimes I don’t know, and are being seen by other members of the practice, if they’re in the top five per cent, high risk, then I can have a look and see, it’s almost like a peer review, see what’s going on, what’s being done, we can then discuss it in our clinical meetings, and then take that to the case conference and then there’s learning. So that really triggers off a lot of things in the practice, is the patient getting the right treatment, what are we learning from it, and improving patient care. So getting that really integrated approach’ (GP) There were also comments from some expressing confusion about what the care plan was aiming to achieve and that given its wide remit that they were not adequately designed to provide better quality care and they did not want it to be simply a hoop they had to jump through: ‘Is it recording of the care already planned? Or systematic screening of those at risk for certain conditions? Or a complete reassessment of each patient care done by a nurse who has never met the patient in 20 minutes with a pro-forma that does not address many patient concerns’ (GP) ‘It does create a lot of work… You don’t just want it to be a, kind of, simple tick, you know, if you really thought you could help, but you need to make life easier for the clinician doing it’ (GP) Overall the providers demonstrated a commitment to what the care plans were hoping to achieve, but felt they needed more work to develop into a tool that would be able to achieve those aims. They also commented that the care plan could promote more patient-centred care by letting the patient see what is planned and what progress is expected. Some providers mentioned that the plan itself supported the principle of involving patients in their care and meeting the commitment of ‘no decision about me without me’. When asked to reflect on what they think patients may have experienced since the pilot began, providers told us that they recognised that many would not really be overly aware of, or concerned by, the pilot or its new mechanisms and instead were more concerned by the care they were able to access. ‘I don’t think patients are interested actually – they just want you to tell them what to do [to get better] or where to refer them’ (GP) However, they were generally in agreement that patients would like it because the pilot enables numerous services to work together and that their issues were being discussed by a group of experts deciding how best to support them: 21 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 ‘I think our patients like it because its multi-service’ (GP) ‘There was one patient… who was quite pleased that her case was being discussed amongst a group of multi-professionals’ (Hospital Consultant) And this was seen as having a potential impact on patient self-empowerment and selfmanagement, which was welcomed by the providers we interviewed: ‘I think the care plan could have improved the way the patients viewed selfmanagement, because it’s more or less, they’d say to them, you know, you need to manage this and these are the things we’re doing, and this is what you’ve got to do, which verbally we’re always saying to them. And I suppose if it’s written down… it might improve that’ (GP) Some also told us that the care planning, and being part of the ICP overall, had a positive impact on their professional practice. This was often articulated with regards to being able to provide a more holistic care for patients: ‘I think with the elderly patients, being prompted by doing the care planning to look at end of life issues and to directly assess falls and cognitive things, quite a lot of that... quite a lot of that was done on the basis of, ooh, did they look like an obvious clinical need, whereas now, by being part of this tool, this, sort of, whole thing, I am, just by matter of routine, because I need to do it for the care planning, asking those questions which I probably wouldn’t have asked as many of the patients before. And I found that positive, that hasn’t been a bad thing, it’s been quite useful to do that and pick up some sort of... a bit more cognitive decline and falls risks and so, yes’ (GP) ‘It’s changed my management in a way, for example, I visited a patient where I’m now actually thinking, rather than just her blood pressure and her cholesterol… I’m now going, what’s her continence like? What’s here social care like? What’s her memory? What’s her mood? In my mind I’ve far more of the memory clinics, the district nurses; it’s sharpened my mind very much to what’s there, a more holistic approach’ (GP) Sustainability of the ICP The feasibility and potential of the ICP to extend beyond its initial pilot phase were discussed with providers during interviews and focus groups. Some told us that their decision to continue to be part of the ICP would be contingent on a number of factors. These factors included: Aims for the next stage of the ICP Level of engagement or influence they might have in shaping the direction of this new phase Financial incentives that would be made available Results from the evaluation and new plans of value for money Impact the next stage of the programme would have on their workload Plans to support the programme as it continues to grow. A collection of extracts exemplify the summarised views: 22 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 ‘I think it’s quite hard to say. If you knew that it was effective and that… there were actually savings or there were actually admissions that had been reduced because of what we’re doing’ (Secondary care manager) I don’t know yet. I’m waiting to see what they want us to do, and what they pay, and without that information one can’t know. I will judge it simply on how much work it is and what we’re paid for it. I mean it will be a sort of commercial relationship, as I see it’ (GP) They are massively missing the trick if they don’t tap some of that potential in the right way, because at the moment, it’s like we’re horses and they’re dragging us to water and the more they drag me, the less I will actually drink. They have to, they have to make it easy for me to want to make it work, and that’s the opposite of what I feel they’re doing at the moment’ (GP) The providers’ comments and suggestions for the future of the programme focused on practicalities, evidence of change and organisational logistics of their time, and the functionality of the systems the programme was dependent on the IT tool. Because of the delays in the IT tool being in place and fully functional, many expressed scepticism about its success going forward and were critical of the costs incurred to get the tool working the way they felt it should have from the outset: ‘I think that the new ICP tool is actually not going to be a 50/50 ownership, which the existing one has been. I think it’s going to be owned by somebody else... I think there’s a lot of uncertainty, and I’m sure they’ve got [ICP] very challenging timelines to meet. I wish them well, but I think I feel sad to see the resource squandered, as I see it’ (GP) ‘I think the IT is really important, because there’s less continuity of care from doctors themselves. We’re all busier running CCGs, going on courses, doing our appraisals. There are more people who are part-time doctors, for one reason or another, and therefore, I think continuity of care is probably less present amongst human contact than it used to be’ (GP) Communication and engagement seemed to be key considerations of providers when asked about their willingness to be part of the ICP. Comments ranged from discontentment with a lack of feedback about performance to outright suspicion that frontline expertise had not been involved in developing certain aspects of the pilot. The message was that they wanted to be engaged and felt that a ‘grass roots’ level approach to developing the programme was urgently required. Many felt they had not been engaged and that there was a disconnection between the IMB decisions, MDGs and the work in practice. ‘I just think we [GPs] live in another world; it’s like living in a bubble. They don’t understand that… you know, I’ve even been to some of the IBMs or whatever you call them... You know, they say, you know, we really, you know, admissions are going down... they can’t implement anything medically without the rigour of statistical analysis and back up and they’ve absolutely no evidence whatsoever. So it just didn’t ring true... [They are] more pestilent than actually helpful. You haven’t done this, you haven’t sent your case yet for the MDG, you know, you haven’t done enough care planning; it was all that’ (GP) 23 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 What we found in the analysis of the focus groups proceedings was that providers were keen to be part of the development of the ICP’s future objectives and their frustration for not having been sufficiently engaged so far: ‘[it feels like] there’s very little anyone can do to impact the way it’s going forward… decisions have already been made… I don’t feel that we’ve been sufficiently involved in those decisions’ (GP) ‘I’ve given so many hours to this thing. Like, more than any other kind of non-work… it’s a sort of non-core work project. So I do lots of other little bits outside, kind of, the job here, but nothing has come close to how much time I’ve given to this. So actually, I feel quite invested in it in lots of ways’ (Hospital consultant) Interestingly, a psychiatrist mentioned with conviction that if the bureaucracy and the workload remain as they are, the GPs will not be part of any extensions of the ICP. ‘I think the biggest challenge the ICP will face is if it does not make it more… it does not make it a leaner, more salient process for the GPs, they’ll walk actually. I’m pretty sure of that’ (Hospital consultant) Providers were also keen to see the IT systems integrating with existing systems so that they could make referrals between services, between primary and secondary care and reduce the duplication of work that was necessitated by using the IT tool and the software they already had. They also had suggestions for more open access for hospitals into the notes to further integrate the information sharing of patient records. ‘From secondary care it’s incredibly useful to be able to identify information about a patient because sometimes the patients get admitted out of hours and don’t have anyone with them… they may be acutely confused so you end up admitting them until you can get the information… if you had access [to] their care package…’ (Hospital consultant) ‘Maybe a more elegant solution would be for the hospital to directly access the records as and when they needed it’ (Secondary care manager) Patient perceptions on provision and continuity of care The following sections describe patients’ responses regarding their registration with and understanding of the ICP, the process followed for their registration and the impact the ICP had on their care. Patients’ views on their current care and their expectations from it are also described. Registration and consent One of the main themes explored in the interviews were the patients’ experiences with their ICP registration, which involved signing a consent form after they received relevant information by their primary care provider. While some patients reported being registered with the pilot, the majority of them did not at all recall it, despite the fact that they were identified by the GP practices as registered patients: ‘No I don’t know nothing… I’m only registered with my doctor and that’s all I know’ (Female, over 75) 24 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 We asked the patients about the procedure that was followed for their registration with the ICP. Their responses indicate inconsistent patterns amongst practices and suggest the lack of clear pathways in the registration process. More specifically, the analysis of the interviews revealed different approaches to registration in terms of the person (doctor/nurse/GP manager/receptionist) who informed the patients about the ICP and took consent for their registration; the way that they were approached (via telephone, in person in the practice or by giving them leaflets) as well as the time spent explaining the ICP and registering them. Some patients were informed and registered by their GP. The registration for some of them happened during a regular appointment, whereas others were invited to the practice in order to be registered, without, however, the patient always realising the purpose of the visit, or even what they consented for: ‘How did I find out about it; I just turned up, regular GP appointments at my GP surgery… and the doctor said to me, ‘by the way do you want to partake in the ICP project’? I said what’s that? And she just said it’s a parallel computer system which will have all your data on it should you turn up and need medical treatment at a hospital or whatever. And I said yes, that’s great, that’s a good idea. That’s how I found out, initially’ (Male with diabetes) ‘Well, I think I was invited to go there, and I didn’t go. But to be honest with you, I don’t know why was that, because the doctor saw me and just asked me my name, put it into the system, and that’s it’ (Female with diabetes) For some other patients it was the nurse who actually informed them about the ICP and registered them in the pilot. However, there were also patients who recall being registered by the GP manager or the GP’s receptionist. As for the way they received information, this varied from being given a face-to-face explanation, to receiving a phone call or a letter, or even being given ICP leaflets to read and find out about the pilot: ‘For the first time I met the nurse here. Then the nurse, called, I think [nurse’s name], she explained to me, and gave me more time, she said whatever I don’t understand, I should ask…’ (Male with diabetes) ‘… I was given a leaflet, and then I read on about it, and to my conclusion it’s interesting and patients will benefit with it… No, he (the doctor) didn’t tell me about’ (Female over 75) As for the time spent for the registration, this is the one aspect of the process where there seems to be a conformity across settings, as patients’ responses from different practices indicate that overall it was a fairly quick process, as demonstrated by the quotes below: ‘I think it wasn’t more than two minutes’ (Female with diabetes) ‘I thought well, you know, there’s going to be a lot of information which he’s going to have to put into a database, but instead, it took about six or seven minutes and it was only one page of data to go in, it was the very basic…’ (Male with diabetes) 25 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Understanding of the Integrated Care Pilot The patients’ understanding of the pilot was vague, as they didn’t seem to have a clear understanding of the programme or its aims. Some remembered hearing something about it but weren’t certain what exactly, or confused it with another scheme. The findings indicate a lack of clear explanations of the pilot from the GPs or from the overall information given to patients: ‘Yes I know, but I don’t know exactly what it means. But is it something like the GPs are merging with the local hospitals or something like that?’ (Female over 75) ‘…Yes, (it’s) like an insurance or pension kind of thing, isn’t it?’ (Male with diabetes) However, the majority of those patients who recalled being registered with the ICP reported having a good understanding of the pilot and its aims, as demonstrated by the following quotes. Some of these patients were not only able to describe the ICP, but also the wider benefits and positive impact on their healthcare and quality of life: ‘Well, I can tell you what I think it is; basically, it’s a pilot of information system for diabetics so that if I turn up at any casualty or hospital in the country they will be able to access a complete profile of my health via the computer screen and also with access to my GP’s clinic if they wish to contact a person with my knowledge of my medication and my history’ (Male with diabetes) ‘…Yes, according to the explanation the nurse I met gave me it is to pilot my healthcare to know, especially with the diabetic patients, to know, to take proper care of us, and you detect every of our test, and file them to give us every information regarding our health’ (Male with diabetes) ‘I think, what I understand the integrated pilot is, it’s a team of doctors that will have to work together, and it’s a patient’s benefit that she will be well taken care of, with regards to whatever medicines she takes. And whatever sickness, illness she has’ (Female over 75) Patient care plans We then asked the patients who recalled being registered with the ICP to reflect on the care plans that had been put in place, following their registration. Not all patients recall having a care plan. The quote below demonstrates the patients’ understanding of their care plan: ‘What do you mean ‘care plan’? No… Whenever I come to the GP, she sends whatever I need, she sends to the specialist, or the hospital, all that. That's all I know’ (Female over 75) Nevertheless, there were also patients who knew that they had a care plan, understood it and were able to describe it: ‘The plan she [nurse] gave to me, she told me from time to time she would be calling me for tests, blood tests, or to take my blood pressure, or check my weight, and ask me about my diet’ (Male with diabetes) 26 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Impact of ICP in the provision of care Subsequently, we asked the patients who recalled being registered whether they had noticed any changes in their care after they became part of the pilot. Some patients didn’t report any changes, a fact they attributed to the relative short time they had been registered with the scheme. For those however who did notice changes, these were overall positive and involved the sharing of information between the different healthcare providers, minimising bureaucracy, increasing cooperation between providers and creating better channels of inter-professional communication. Even more so, the findings suggest a positive impact extending beyond the provision of care into patients themselves, as they reported feeling more empowered, better protected and safer. In the heart of this theme was the patients’ perception that the ICP would increase communication between patients and providers and create the opportunity for a more holistic and betterorganised approach to care, with improved communication channels between the different providers. It was also perceived that the ICP had the potential to help the patients lifting the burden of trying to coordinate their medical care in terms of appointments and diagnostic tests, and that this was now in the hands of people within the system who could do it more efficiently while using the correct resources. The extract below exemplifies this finding: ‘I really think that is very good, it’s a very good idea to have different people involved with your healthcare, and you don’t have to book appointments by yourself, to call in for different, or to make appointments for you. But when you see the first doctor, either a doctor or a nurse, they know where to send you to and they have already shared your information to see what they would do for you’ (Male with diabetes) Furthermore, the view was expressed that integrated care is a positive development, as it brings together healthcare professionals across a range of different specialities with the aim of focusing on and providing patient-centred care. A new element of possible collaboration that according to this patient is missing from the current system is the integration of research into daily practice: ‘Yes, integrated… I personally believe that that could revolutionise the whole medical process, not just diabetes but across the board because it’s a fundamental different shift in emphasis. Because the whole nature of science is divide, sub-divide, specialise, getting to know more and more about this and it all becomes so fractioned. And you have all these wonderful experts doing fantastic research but nobody’s tying all the bits together…’ (Male with diabetes) Some patients reported feeling being cared for, safer and more protected within the ICP and that one of the additional benefits of the pilot was that they were now encouraged by the system to care more for their health and act in order to improve it: ‘They are pushing, calling me and writing me a letter, they push me, they encourage me to do it. I really find that very positive’ (Male with diabetes) ‘Yes, I feel safer, like… I feel like they care for me, for my health’ (Male with diabetes) Quality of care delivery in general During the interviews we also explored patients’ perspectives regarding their care overall, irrespectively of their involvement in the ICP or not. 27 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Some patients seemed to appreciate the quality of the services they receive within the NHS: ‘The quality of the services? Ten out of ten… Because you get exactly what it says on the label. They do your blood pressure, they do your HPA, they examine your eyes, they do blood tests and you get meaningful results back’ (Male with diabetes) ‘I mean when I’ve been getting treatment it’s been first class’ (Male over 75) For some patients, a main ‘quality indicator’ was access to seeing a doctor within a reasonable timeframe. In the following interview extract the patient advocates that doctors have time to see more patients and that being asked as a patient to make two appointments to be seen for two complaints does not resonate well: ‘Well, I think everyone is entitled to see a doctor straightway if they need to. The doctors, they have time, because they could see many, many people during the day or during the hours they have. But they only said I only have ten minutes. If you want to see me for something else, you have to make a double appointment…’ (Female with diabetes) Although walk-in clinics may be offering immediate access, according to the patient below continuity of care may suffer as the patient does not know which doctor they are going to see: ‘Yes, at my GP’s clinic it generally takes two to three weeks to get an appointment to see your GP. They have a, kind of, urgent medical appointment facility in the afternoon, but to do that you have to go down to the surgery at two o’clock, queue up, the appointments are allocated at 14:30, you don’t know what doctor you’re going to get to see and you don’t know what time you’re going to get; generally you’ve only got five to ten minutes max to see the doctor. So that’s pretty unsatisfactory’ (Male with diabetes) Other patients reported the challenges and difficulties they faced organising their care because of lack of communication between levels of care in the NHS: ‘Oh, definitely frustration… I felt like hitting my head against a wall. I thought why don’t they talk to one another?’ (Male over 75) Also, various practicalities such as a poor performing booking system may be perceived by patients as a barrier to quality and continuity of care. In the extract below, the patient touches on the issue of responsiveness, highlighting that waiting times, either for booking an appointment or for seeing the relevant provider, is important to patients: I think the bureaucracy of the National Health booking system I think is… needs an overhaul. That speaks for itself. I think… now if that were to improve and they were able to give you more information at the time… instead of leaving you for months not knowing what’s happening…’ (Male over 75) 28 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Patients’ narratives on ideal care We asked patients to tell us about their views of ideal care and what this care would entail. Prominent themes were improved communication with providers and a sense of continuity of care, especially concerning keeping in communication with one doctor: ‘Well, to be able to communicate with my doctor or to the nurse, asking them things or they suggesting things. I think that would be a nice thing’ (Female with diabetes) ‘…One of the most maddening things of all is you go into the GP’s surgery and there’s about ten different GPs in the practice, you don’t know who you’re going to see, you know, and it’s a diabetic clinic or they’re checking up on your HbA1c reading or your blood pressure, or whatever, and they make a comment on your HbA1c and say it’s a bit high or it’s a bit of this or a bit of that. And I just feel like they’re pulverising you into the next dimension because there’s so much judgment in that, I feel punished…. Because they’re giving me no respect at all… That’s the old regime and that still happens, it happened just two weeks ago; ignorance…’ (Male with diabetes) Finally, patients expressed openly the need for medical care with less bureaucracy and with clear care pathways as well as transparent communication patterns with patients: ‘Something that I would like to change?… that bureaucracy business. If only, if only they would take time to think that they’re talking to people and people want to know what’s happening to them, instead of this terrible silence between even booking clerks who make appointments for you. It’s just the lack of… the length sometimes between the treatments and knowing what’s happening and not being told what’s happening is probably the most valid… It’s infuriating, because you get so fed up with them you want to scream at them sometimes: wake up, wake up! It’s me. It’s my life!’ (Male over 75) As most patients were largely unaware of the objectives of the ICP, we described the objectives to them and asked about what they think about its potential to affect care. The patients responded that if the ICP worked as intended, it would solve issues of communication, enhance care and facilitate time management: ‘Well, if it works it will be a heaven: if it works. You know, I mean that would be… that would be ideal!... that would solve a lot of problems: in fact the main problem, which is communication’ (Male over 75) ‘(If it worked)…it would be wonderful’ (Female with diabetes) ‘And I think that that would really facilitate speedier treatment and more confidence for them, less time wasting, misrepresentation, it just seems to make a lot of sense’ (Male with diabetes) Provider survey The data show that providers feel that integrated care has the potential to deliver its objectives, but this requires tools that simplify its processes and facilitate care planning. Specifically, the dominant perception resulting from the surveys was that the ICP improved professional communication and collaborative working across different levels of care, enhanced knowledge sharing and resulted in moderate improvements in patient care and shared decision-making. On 29 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 the other hand, it generated extra work and frustration for providers due to the inefficiency of the IT tool. Overall, health providers expressed a positive view about the new model of care, but concluded that it needs time before it extends to other chronic disease areas. The main findings from the professional survey are summarised in Table 3. Table 3: Overall impact of the ICP 1. Improved communication and collaborative working across different care levels 2. Enhanced knowledge sharing and inter-professional working through the MDG case conferences 3. Moderate improvements in patient care and shared decision-making 4. Extra work for all those involved in care planning (especially GPs) 5. General frustration due to the inefficiency of the IT tool Perceived ICP impact Overall, 68% of respondents shared the view that the ICP resulted in better collaboration across different care levels, with an equal representation among the two main groups (GPs=67.7% and non-GPs=68.4%). In addition, the data reveal a perceived moderate improvement in patient care (53.1%) and an increase in patient involvement in decision-making (51.1%). In contrast, integrated care did not have a positive impact on care delivery, with 51% of respondents reporting that it did not change the way they provide care to patients. Despite the general agreement between all professional groups, there was variability in their responses regarding the impact of the ICP on service duplication – 51.6% of GPs answered that the ICP resulted in less duplication, compared to 23.5% of non-GP participants. Table 4 presents the perceptions of GPs and other providers in relation to the overall impact of the integrated care pilot. Table 4: Perceived impact of the ICP per professional group Other providers GPs Combined Agree % 45.2 Disagree % 22.6 Agree % 66.7 Disagree % 11.1 Agree % 53.1 Disagree % 18.4 Reduced service duplication 51.6 21.8 23.5 41.2 31.3 41.7 Improved collaboration 67.7 9.7 68.4 10.5 68.0 10.0 Eased patient identification 45.2 29.0 52.9 23.5 47.9 27.1 Was liked by patients 25.8 22.6 6.7 20.0 19.6 21.7 Strengthened joined decision-making 48.3 27.6 55.6 5.6 51.1 19.1 Changed the way care is provided 19.4 54.8 33.3 44.4 24.5 51.0 Improved patient care Patient care plans The findings also show that the electronic care plans complicated the professionals’ work and added to their workload. In particular, nearly 58% of respondents (GPs=61.3% and nonGPs=50%) felt that the new model of care had a negative impact on their workload and 42% agreed that care planning has become complex. Table 5 lists the participant responses in relation to the impact of the ICP on care planning, patient experience and clinical work. 30 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Table 5: Providers’ experiences of ICP care plans GPs Other providers Combined Agree % 32.3 Disagree % 45.2 Agree % 21.4 Disagree % 35.7 Agree % 28.9 Disagree % 42.2 Was well received by patients 19.4 22.6 15.4 7.7 18.2 18.2 Simplified clinical work 16.1 61.3 21.4 50.0 17.8 57.8 Made care planning easy MDGs Providers also expressed a positive opinion about the MDG meetings and the opportunities to share knowledge through discussion of patient cases. More specifically, 78.7% and 76.1% of participants reported that the MDG case conferences enhanced inter-professional learning and professional knowledge. This view was shared among all medical consultants, social workers, community nurses and other healthcare staff. In total, nearly 90% of non-GP respondents agreed with the previous statements. Participants also replied that the MDGs improved inter-professional collaboration in practice (71.7%), reinforced existing communication patterns (58.7%) and made their voice heard (55.6%). Table 6 shows the perceptions of GP and non-GP professionals on the effect of MDGs on inter-professional learning, collaboration, knowledge sharing and communication. Table 6: Perceived impact of MDGs per professional group GPs Been a good use of professional time Facilitated professional collaboration Improved knowledge of patient care Provided learning opportunities Made clinical voice heard Reinforced communication Other professionals Combined Agree % Disagree % Agree % Disagree % Agree % Disagree % 60.0 30.0 52.9 17.6 57.4 25.5 63.3 16.7 87.5 0 71.7 10.9 76.7 20.0 75.0 6.3 76.1 15.2 73.3 16.7 88.2 0 78.7 10.6 48.3 20.7 68.8 0 55.6 13.3 63.3 20.0 50.0 6.3 58.7 15.2 The IT tool Responses by professionals in the survey indicate that the training which was provided for the IT tool was not adequate (56.8%). In addition, providers reported that the new system did not offer access to all the required information to provide high-quality integrated care (56.8%) and it did not integrate with other clinical information and communication technology (ICT) systems (55.6%). Because GPs were the main users of the system, they expressed their dissatisfaction with the tool in all IT-related questions, while hospital consultants and other health professionals took a milder view. Table 7 presents the responses of the participants’ regarding the IT tool. 31 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Table 7: Providers’ experiences of the IT tool GPs Enabled retrieval of incentives Provided access to all the required data Enhanced information sharing Integrated well with other clinical ICTs Required more training Is essential to provide integrated care Other providers Total Agree % 25.8 Disagree % 38.7 Agree % 16.7 Disagree % 33.3 Agree % 23.3 Disagree % 37.2 12.9 61.3 7.7 46.2 11.4 56.8 29.0 45.2 28.6 35.7 28.9 42.2 16.1 54.8 14.3 57.1 15.6 55.6 67.7 6.5 30.8 38.5 56.8 15.9 25.8 51.6 35.7 35.7 28.9 46.7 Patient survey The findings from the patient survey show that patients are happy with most aspects of the ICP. However, the data reveal that most patients do not have or are not aware of having a care plan. In addition, only one in ten patients reported that they have a copy of their care plan. Overall, patients responded that the ICP increased patient involvement in decision-making and improved their relationship with their GP. There was also a general consensus that providers should share their care plans with each other in order to deliver high-quality integrated care. The main findings from the patient survey are presented in Table 8. Table 8: Patients’ experiences of the ICP Overall impact of the ICP 1. The majority of patients are not aware of having a care plan 2. One in ten patients has a copy of their care plan 3. Increased patient involvement in decision-making 4. Improved GP–patient relationship 5. Inter-professional communication is highly appreciated by patients Perceived ICP impact All patient groups expressed a positive opinion about the ICP and its impact on different aspects of care. Nevertheless, they also reported that they did not experience any changes in the provision of care itself. The dominant perception was that the new model increased their involvement in decision-making. Nearly seven in ten respondents shared this view, compared with 10.3% who did not feel more involved in decisions about their care. In addition, the majority of participants from all patient groups replied that the ICP provided an opportunity to develop a better relationship with their GP (61.7%) and increased their understanding of the role of different health and social care actors (53.5%). They also felt that the ICP improved inter-professional communication (49.6%) and resulted in healthcare staff asking fewer questions about their medical history (54.40%). All patient groups reported that they can have easier access to NHS services (57.6%) and that they have reduced the time that they used to spend to book appointments to see their GP and other health professionals (46.1%). However, despite the general agreement among all patient groups on the positive impact of the ICP, 53.6% of 32 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 respondents said that they did not experience any changes at the point of care provision. Table 9 summarises the patient perceptions of the ICP and its impact on different aspects of care. Table 9: Perceived impact of the ICP per patient group Over75/Diabetes Increased patient involvement in decisions Improved patient care Enhanced knowledge about professional involvement Improved relationship with GP Increased awareness of the role of health/social care workers Improved communication among professionals Reduced effort to organise care Improved access to NHS care Reduced the times that had to explain their medical history Changed nothing about their care Over 75 only Diabetes only Agree % Disagree % Agree % Disagree % Agree Disagree % % 67.9 9.5 72.4 6.5 64.8 58.3 11.9 52.8 6.9 51.9 16.0 52.8 67.5 14.5 50.6 Combined Agree % Disagree % 16.4 68.9 10.3 54.1 14.8 54.4 9.7 14.3 46.2 21.8 50.7 17.3 62.4 8.5 57.0 13.2 61.7 11.8 13.3 58.2 9.2 48.7 16.8 53.5 12.5 48.8 12.2 53.0 9.8 44.6 20.7 49.6 14.0 51.9 19.8 48.1 17.5 38.8 24.0 46.1 20.3 56.5 20.0 62.5 12.5 52.1 24.4 57.6 18.2 56.6 24.1 55.8 13.0 52.1 18.5 54.4 17.5 60.7 14.3 53.9 17.1 47.5 22.5 53.6 18.3 Patient care plans The findings from the patient survey reveal that nearly eight in ten respondents (77.6%) at the time of the study were not aware of having a care plan. In addition, only 9.3% of patients reported that they have a copy of the care plan that was created with their GP. More specifically, 82.7% of patients with diabetes said that either do not have, or do not know (DK) that they have, a care plan. The situation was slightly better in the other two categories with 23.4% of patients over 75 years and 29.1% of the elderly with diabetes reporting that they have created a care plan with their GP. However, just 8.4% and 12.0% answered that they have a copy of their plan, respectively. Table 10 presents the proportion of respondents who reported that they have a care plan according to different patient groups. 33 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Table 10: Care plans per patient group Over 75/ Diabetes I have a care plan I have a copy of my care plan Over 75 only Diabetes only Total Yes % 29.1 No/DK % 70.9 Yes % 23.4 No/DK % 76.6 Yes % 17.3 No/DK % 82.7 Yes % 22.4 No/DK % 77.6 12.0 88.0 8.4 91.6 8.1 91.9 9.3 90.7 One in five patients reported that they had a care plan (CP), while a high proportion (77.6%) replied that either had not created a care plan with their GP or that they were not aware of having one. Patients with a care plan demonstrated a great enthusiasm towards the new way of care planning (Table 11). Specifically, they felt that were involved in the design of their care plan in the way they wanted to be (65.1%) and that they had a clear understanding of how care planning works (78.8%). Table 11: Patients’ experiences with ICP care plans With a CP Without a CP Total Agree % 78.8 Disagree % 7.1 Agree % 7.0 Disagree % 42.6 Agree % 26.1 Disagree % 33.3 Involved in care planning 63.4 12.2 8.6 41.2 23.0 33.6 Were for the GPs to decide 63.8 13.8 39.7 29.5 45.8 25.4 Understand how care plans work Increased feeling that health professionals talk to each other Involved in the desired level 62.2 11.0 40.0 23.0 46.0 19.8 65.1 8.4 12.8 38.3 26.9 30.6 Not involved in care planning 36.4 41.6 29.9 24.8 31.4 60.6 Professionals should talk to each other 94.1 3.5 72.1 9.2 77.7 7.8 CP Patients – Total Agree% Disagree Understand how care plans work 78.8 7.1 Involved in care planning 63.4 12.2 Were for the GPs to decide 63.8 13.8 62.2 11.0 65.1 8.4 Not involved in care planning 36.4 41.6 Providers should talk to each other 94.1 3.5 Increased feeling that health professionals talk to each other Involved in the desired level In contrast, non-CP respondents reported very low levels of involvement in the planning of their care (6.0%). Overall, CP and non-CP respondents provided conflicting answers to nearly all CPrelated questions. There was a general agreement, though, in relation to one fundamental principle of integrated care: inter-professional communication. Nearly 94% of patients with a care 34 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 plan replied that providers should share their care plan with each other. This view was also prevalent between non-CP respondents (72.1 %). MDG communication We observed four MDGs over time and audio-recorded 23 case discussions, resulting in 4,209 utterances each of which was coded three times – Level, Valence and Focus. This corresponded to around 400 pages of verbatim discussion in the MDGs. Table 12: MDGs included in the study MDG 1 2 3 4 Date Type No. GP No. Duration No. Utterances/case practices participants cases Mean(SD) 14022012 Diabetes 10 14 2 hours 7 170.7(52.6) 23022012 Elderly 6 16 2 hours 8 145.4(76.2) 01032012 Elderly 5 15 2 hours 4 193.0(135.9) 15032012 Elderly 4 11 1 hour 4 269.75(140.5) Total 23 183.0(98.8) Case discussions were dominated by the consultants and the presenting GPs, with little involvement from GPs that were not presenting the case. Allied health professionals contributed as much as consultants overall, however because there are routinely many more allied health professionals in an MDG than consultants, their contribution per person is much less. There was no significant difference in this pattern across the four MDGs. Figure 4: Distribution of utterances (%) per participant type across all MDGs (standard error bars shown). (For all MDGs consultants=2, PGP=1, Chair=1; For MDG 1 NGP=6, MDG 2 NGP=4, MDG 3 NGP=3 and MDG 4 NGP=4; For MDG 1 Allied=3, MDG 2 Allied=3, MDG 3 Allied=5, MDG 4 Allied=2) Figure 4 shows the distribution of utterances according to their integrative potential across all the MDGs. The integrative potential of MDGs was generally low. Emphasis was on the exchange of patient or individual level information and orientation. Although some time was spent on higher levels of abstraction at the collective and systems levels, this was much less preponderant. Overall, there was more emphasis on solution-oriented talk compared to problem-oriented ones 35 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 however because this was predominantly at the individual level, it scores lower on the integrative potential for the group as a whole. There was little difference in this pattern between the MDGs. Figure 5: Proportion of all utterances (all MDGs) by Event Code domain (does not include uncodeable utterances) The emphasis on the lower integrative potential event codes was driven, largely, by the presenting GP and consultant. Allied health professionals contributed much less to the discussion than the other participant types however, they do account for a disproportionate amount of the higher Event Codes (Figure 6). Figure 6: Proportion of Event Codes by participant type for all MDGs (does not include un-codeable utterances. Finally, Figure 7 shows the distribution of the utterances with respect to their integrative intensity throughout the duration of the case discussion. Here we have used standardised weighted means of integration intensity for each decile across all MDGs. In each MDG, the integrative intensity of each case discussion exhibited broadly similar characteristics – beginning at a low level, a function of the case presentation, and rose to greater levels of abstraction during the course of the discussion. As found in the interviews and surveys, this represents the shared learning and 36 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 discussion of best practice that respondents found useful in the MDGs. However, only two of the several dozen action points identified during the case discussions were ‘beyond’ the care of the individual case – to distribute a directory of services and to send some information on community care alarms to the MDG participants. This represents a missed opportunity for participants to consolidate their discussions into actions for outside of the MDG and for the benefit of broader groups of patients. Figure 7: Average standardised Integration Score per time decile of case discussions 5. Discussion The King’s Fund report, The case for integrated care (Ham and others, 2011) highlights the major challenges that the NHS is facing in terms of using resources more efficiently to meet the needs of an ageing population and of people with chronic conditions. To meet the above challenges locally, the NWL ICP implemented a new model of care in which health and social care professionals would work more closely to meet the needs of patients and to coordinate services so that patients experience a more ‘joined-up’ care. The high-level objectives of the NWL ICP are to prevent ill health, support self-care and increase collaborative working between primary care teams and specialists as well as between health and social care. In their report, Ham and colleagues (2011) discuss the multiplicity of barriers to the implementation of integrated care, including organisational complexity in the health and social care sectors, divisions between GPs and specialists, perverse financial incentives, and the lack of a single electronic system for the management of patient health records. Our analysis of patient and provider perceptions showed that although the vision of the ICP was largely shared and supported by most of the stakeholders, including the patients, all of the barriers outlined above were quite prominent in the implementation and execution of the NWL ICP. Our research revealed an enthusiastic new organisation, keen to succeed, but having to solve a number of complex organisational issues along the way, whilst already delivering the pilot. Multiple changes to the size of the pilot, and the number of organisations involved also added to the complexity, as did the turbulent political and policy environment of the national health economy. 37 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 The launch of the ICP was met with enthusiasm by providers, as the value of integration to support the care of local patients was apparent to all. Participants told us that the ICP was developed with a reasonable implementation plan, which was supported by three appropriate interventions: patient care planning, patient case conferences in MDGs and a fit-for-purpose IT tool. As with any pilot, particularly one that requires extensive organisational re-structuring, provider buy-in, IT investment and operational management, time is of the essence, both an adjustment and a normalisation period, where operational processes, incentives and infrastructure get re-fined, are expected. Professionals, especially clinicians, reported that they were sceptical about whether the ICP had set objectives that would not possibly be met in the short timeframe that they had available for implementation. Despite the wide engagement of local providers from all specialties and levels of care in the IMB, MDGs and several ICP sub-committees, our analysis of interviews and focus groups with providers revealed a quite prominent perception of division between those who ‘implement’ (the ICP management) and those who ‘execute’ (health and social care providers). Those who implement are seen as decision-makers and being responsible for the smooth operations of the ICP. When an ICP operation is not working as smoothly or as successfully as it was initially expected, those who execute tend to disengage with the ICP and its objectives. One characteristic example of the above finding is the widespread frustration around the operation of the IT tool. As intended, providers perceived the IT tool as a fit-for-purpose intervention, which was developed to facilitate the clinical and operational objectives of the ICP. The IT tool was expected to support communication and sharing of information between levels of care as well as to minimise the providers’ workload by being interoperable (able to communicate with existing IT systems), reliable and user-friendly. We know from our engagement with the ICP and from our analysis that not only did the IT tool not support the above functions but it also caused widespread frustrations, which were directed towards the management team. While frustration with the IT tool and its failure to deliver has been a constant, the surrounding perceptions have been tidal and altered alongside the progression of the pilot itself. The providers’ views of MDGs were largely positive with their attendance having, over time, generated new networks and knowledge, facilitated learning and the desire to formulate new informal practices of engaging across the care spectrum with their colleagues. We found that the MDGs were beginning to generate small practice changes and optimism that they might facilitate more in the future. However, our participants were mindful of the cost of their time, the backlog of work from attending meetings and the need to optimise efficient working of the case conferences in order to ensure they continue to demonstrate value. Investment of time in attending the MDGs was felt to increase sharply and as the work began to feel like duplication some felt their time was not valued and they were expected to drop their normal commitments to meet the time limited targets of the pilot. Other than identifying ways to improve the care of the individual case/patient brought to the discussion, the objective of the MDGs is mainly to foster a cultural change in ways of working and improving integration more broadly. This is important for a range of operations in the ICP but particularly essential in a forum such as an MDG where the integrated care context, case conferences are potential touch points for examination of the broader inefficiencies and challenges in the inter-organisational environment. Early in the implementation stage of the ICP, this objective was clearly articulated: 38 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 ‘the MDGs are a vehicle for delivering productivity and efficiency improvements within and across the various providers…[participants should] move away from stereotypes, get to know each other, be reflective and responsive, increase the level of trust, coordination and collaboration across providers working together towards better patient care…..’ (IMB Chair, IMB presentation August 2011 [authors’ emphasis added]). Some providers commented positively about the MDGs and their potential impact. However, our analysis of communication in the MDGs suggests that the predominant focus during case conferences was on the individual patient care. There was evidence that participants were working in an ‘integrative’ mode during the case conferences (i.e. during a discussion, there was a gradual shift from the presentation of the complex case, to shared learning around collectives of similar patients, and issues within the local health economy). However, this did not translate into actions moving forward and, more typically, the group would identify improvements in individual patient care only. Interaction in the case conferences and in the MDGs in general was mostly between the consultants and the presenting GPs. Although each group consists of more allied health professionals than GPs and consultants, they tend to participate much less in the discussion. Also, GPs who were not presenting a case contributed very little to the discussion and this is a missed opportunity to comment, discuss and reflect on, similarities between the presented case and their own patient groups, which again would improve MDG performance and enhance the overall aim of actual integration. Drawing from our analysis of communication, we characterise the MDGs as having consultative characteristics with some trend towards collaboration. Their characteristics resemble CommunityBased Ward Rounds, with little tangible integration occurring within and, by extension, outside of the meeting. At first sight, it appears that the MDGs perpetuate traditional communication patterns of medical dominance, missing an opportunity to work more inclusively, collectively and in a truly multidisciplinary way. In our interviews of MDG participants, we found that there was no clear explanation of MDG goals and objectives – this may have undermined the collaborative potential of the MDG. This suggests that more could be done to sensitise participants to the value of full participation from all members of the group, and for the chairperson and MDG coordinators to capture opportunities to explore learning from individual cases to other similar cases and how services could work better together to improve the care generally. This could range from simply the identification of a new pro-forma to, at the other end of the spectrum, a new service – all working towards an improved and more integrated way of working between autonomous organisations. A central aim of the ICP is the prevention of ill health via careful care planning with the active involvement of the patients. The care plans were perceived by some providers as an opportunity to take a more structured and multidisciplinary approach to care. Those providers demonstrated a commitment to what the care plans were hoping to achieve but felt they needed structural amendments to develop them into a tool that would be able to achieve those aims. They also commented that the care plan could promote more patient-centred care by involving the patient in the planning and reviewing process. Some providers mentioned that the plan itself supported the principle of involving patients in their care and meeting the commitment of ‘no decision about me without me’. However, there is some evidence from focus groups and interviews with providers, which suggest that some viewed the care plans as a ‘box ticking’ exercise that was developed to 39 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 meet ‘prescriptive targets’ and that the actual effect on patient care and outcomes is minimal. We also found a lack of understanding of the objectives of the care plans amongst providers. We recorded wide variability in the time taken to complete a care plan, ranging from a few seconds to half an hour. Also, care plans have been administered by a range of professionals, sometimes by some who were not adequately informed about their scope and as a result could not relay appropriate information to the patients. This might explain the very low number of patients who were aware that they had a care plan – only one out of ten could recall that such encounter had taken place. Patients were largely unaware of their participation to the ICP and of the aims of it. As a result, it was very difficult to retrieve any meaningful information about their perceptions of the ICP from our interviews with patients. Remarkably, when we asked the same question via our survey, more than 60% of respondents replied that they were involved in the process of developing their care plans and that they have a clear understanding about how their care plan works (78.8%). We asked all patients to tell us about their perceptions of ideal care and what this care would entail. The most common answers were around improving both communication with their doctors and continuity of care particularly via receiving care from the same doctor over time. As most of the patients we interviewed could neither recall whether they had a care plan or whether they were registered in the ICP, we described the ICP’s objectives to them and asked them to comment on whether they think the ICP would have an effect on the care they receive. Most patients responded that if the ICP worked as anticipated, it would have a dramatic effect on their care. The small percentage of patients who could recall having a care plan commented very positively on the ICP and its objectives. We also found that patient satisfaction with the ICP was strongly related to the patients’ rapport with their GP reinforcing the view that primary care is a natural ‘hub’ for the ICP. The sustainability of the ICP is mostly dependent on the willingness and drive of a critical mass of providers to extend their involvement in the second year. Providers told us that their future participation would be contingent on a number of factors: Aims for the next stage of the ICP Level of engagement or influence they might have in shaping the direction of this new phase Financial incentives that would be made available Results from the evaluation and new plans of value for money Impact the next stage of the programme would have on their workload Plans to support the programme as it continues to grow. Nevertheless, the most critical question surrounds the sustainability of the integration drivers beyond the lifespan of the pilot. However, this is under significant threat, as most providers associate sustainability with an expectation for financial incentives. Little work has been done so far to plan ahead, beyond the pilot stage, on how integrative work will be sustained in the absence of an organisation that drives the operations and distributes incentives. In the light of these findings, culture change becomes an increasingly important driver, not only for the immediate effectiveness, but also for the sustainability of integrated care initiatives. Increased provider involvement in decision-making may also have a positive effect in facilitating ownership, which may lead to more effective local management. Also, patient and public involvement in designing the care pathways should increase awareness among patients and most importantly enable the clinical team to develop pathways that meet patients’ needs. Some important work is 40 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 currently being undertaken by a team of researchers at Imperial College, who are exposing patients to a series of simulated patient journeys scenarios before they ask their views on how to improve the service. Each of these drivers however, relies on collaborative working – both between and within diverse systems (human and IT). Organisations and professions must recognise this interdependence and define, shape and enact new roles and responsibilities to optimise patient outcomes at minimal necessary costs. Effective communications in relation to strategic, operational, technical and clinical matters, timely sharing of information, as well as cultural change in the way care is provided, appear to be crucial to this. 41 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 References Curry N and Ham C (2010) Clinical and Service Integration: The route to improved outcomes. The King’s Fund. Fereday J and Muir-Cochrane (2006) ‘Demonstrating rigor using thematic analysis: A hybrid approach of inductive and deductive coding and theme development’, International Journal of Qualitative Methods 5(1). Glaser BG and Strauss AL (1967) The Discovery of Grounded Theory: Strategies for Qualitative Research. Aldine Publishing Company. Ham C, Imison C, Goodwin N, Dixon A and South P (2011) Where Next for the NHS Reforms? The case for integrated care. King’s Fund. Kodner DL and Spreeuwenberg C (2002) ‘Integrated care: meaning, logic, applications, and implications – a discussion paper’, International Journal of Integrated Care 2, e12. Krueger R and Casey MA (2000) Focus Groups: A practical guide for applied research (Third edition). Sage. Powell RA and Single HM (1996) ‘Focus groups’, International Journal of Quality in Health Care 8(5), 499–504. Richie J and Spencer L (1994) ‘Qualitative data analysis for applied policy research’, in Bryman and Burgess, eds., Analysing Qualitative Data. Routledge, 173–94. 42 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Appendix 1: Patient survey North West London Integrated Care Pilot: A qualitative evaluation PATIENT SURVEY QUESTIONNAIRE I don’t know I disagree strongly I disagree somewhat I neither agree nor disagree I agree somewhat Section 1: Your experiences I agree strongly Part 1: About the pilot and your care. Please rate how much you agree with each of the following statements about the various components of the Integrated Care Pilot and your overall experience. Please tick one box which best represents your agreement with each statement. Since becoming part of the Integrated Care Pilot... 1 2 3 I feel I am involved in decisions about my care I feel my care has overall improved I know more about which health professionals are involved in my care 4 my relationship with my GP has improved 5 I know what to expect when I see a health or social care worker 6 I have a sense that people providing my care talk to each other about my care needs 7 I need to do less work to organise my care (e.g. chasing up people to organise appointments) 8 I feel I am able to get access to the care I need with no struggle 9 I have had to explain my medical history less often to the healthcare professionals that I see 10 nothing about my care has changed Section 2: Your care plan 11 I have a care plan yes no 12 I have a copy of my care plan yes no I don’t know I don’t know 13 14 15 16 I understand how my care plan works I was involved in planning my care The care plan is really for the GP to decide I feel that decisions about me are not made without talking to me 17 I was involved in planning my care in the way I wanted to be 18 I was not involved in creating my care plan 19 All healthcare professionals that are involved in my care should talk to each other 43 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Part 2: Information about you Please tick one box 1. I am over 75 years old Yes I have diabetes Yes Please enter your age 2. Age ______ Please tick one box 3. Gender Male Please tick one box 4. How long have you been part of the pilot? Less than six 6-12 months months No No Female More than 12 months I do not know Please enter the name of your GP practice (if you do not know, please tick the box) 5. What GP Practice are you registered with? ________________________________________ I do not know Thank you. You have now finished this questionnaire. Please post your responses to the research team at Imperial College London using the stamped, addressed envelope provided. 44 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Appendix 2: Professional survey North West London Integrated Care Pilot: A qualitative evaluation PRACTITIONER SURVEY QUESTIONNAIRE Disagree strongly Disagree somewhat Neither agree nor disagree Agree somewhat Your experiences Agree strongly North West London Integrated Care Pilot: A Practitioner Survey Questionnaire Based on your experiences of providing services to people within North West London Integrated Care Pilot, please rate how much you agree with each of the following statements about the various components of the Pilot and your overall experience. Overall, the Integrated Care Pilot has… 1 2 3 4 improved patient care reduced service duplication improved collaboration across different care levels made it easier to identify patients that need intensive management 5 been well liked by my patients 6 strengthened joined decision making 7 not changed the way I provide care to patients Care plans ICP care plans have… 8 made care planning easy 9 been well received by patients 10 simplified my work MDGs MDGs have (only for those who have attended)… 11 12 13 14 15 16 been a good use of my time facilitated interprofessional collaboration in practice improved my knowledge of patient care provided learning opportunities made my voice heard reinforced existing communication patterns IT tool The IT tool … 17 has enabled retrieval of monetary incentives 18 provides me with access to all the information that I need to deliver integrated care 19 has enhanced information sharing among healthcare professionals 20 fits well with other tools that I use (e.g. Electronic Patient Records, ePrescribing) and in combination helps me to provide a better service 21 requires more training in order to use it effectively 22 is essential to provide integrated care 45 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Section 5: General 23 My role and responsibilities within the ICP are clear 24 I have all the information I need to provide a safe service (e.g. discharge summaries, clinical notes, test results) 25 The ICP should be extended to other chronic disease areas Information about you (please tick all boxes that apply) Professional role Agency What was your role in the planning/development of the ICP? I attend the IMB meetings GP Social Worker Medical Consultant Health Care Assistant Community Nurse Social Care Provider Other (please specify) ______________ GP surgery PCT Research Organization Mental Health Trust Local Authority Community Services Third Sector Agency Hospital or Acute Sector Other (please specify)_______________ I was not involved at all I had some involvement I was well involved All the time Sometimes Never Thank you. You have now finished this questionnaire. 46 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Appendix 3: Patient interview guide NWL Integrated Care Pilot Qualitative Evaluation Patient interview guide Warm-up questions: Q1. Experience of care Thinking about your experiences, how do you find the care that is provided to you? Themes to explore: a. b. c. d. e. f. Access Convenience Appointments (Where is it normally held and by whom?) What is the best /the worst thing about your care? And why? Awareness of what kind of services are available? Level of overall satisfaction g. How do you perceive an effective delivery of care? h. What aspects of care are the most important to you? i. Are they currently available? Q2. If you judge from your care, what can be improved? ICP-related questions Q1. Care Plan Introduce/explain the NWL ICP and then follow with the question: Q1. ‘Do you have a care plan?’ Yes Continuity of care (Do you feel that professionals talk to each other about your care? What makes you think that? (probe for examples if possible, probe about not having to tell the story) do we want to know how they feel about that? Noticing changes in experiencing care (changes to how the care is organised, improvement of care? Care plan: Who spoken to you about the care plan, do you feel you were involved in making it?) No Further explanation of a care plan Yes Continuity of care (Do you feel that professionals talk to each other about your care? What makes you think that? (probe for examples if possible, probe about not having to No Did you notice any changes in the way your care is delivered? (Probe: How is care organised? Do you feel your care improved? 47 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 tell the story) Noticing changes in experiencing care (changes to how the care is organised, improvement of care) Care plan: Who spoken to you about the care plan, do you feel you were involved in making it? 48 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Appendix 4: Professional interview guide NWL Integrated Care Pilot Qualitative Evaluation Professional interview guide Theme 1: Clarity of understanding of pilot aspirations and aims 1. What do you think are the aims of the ICP? a) High quality care and improved outcomes (e.g. reduced admissions, self-care outside of hospital, financial savings) b) Increased coordination and collaboration across different care levels c) Improved patient and professional engagement (i.e. involvement in the care planning/development of care protocols) and satisfaction 2. Why do you think the pilot was extended? Do you agree? What do you think the achievement of the continuation of the pilot will be? Theme 2: Motivation for engagement 1. What made you decide to take part? Theme 3: Impact on practice 1. What has been the impact of the ICP on your practice? a) impact on patient care (what do you believe has been the impact on the way that you provide care to patients?) b) impact on administration of care in your practice c) impact on role/responsibilities outside of practice (MDG meetings) d) What has been the patient’s reaction to the ICP? Theme 4: Benefits and challenges 1. Did you gain anything from being part of the ICP? a) patients (see more patients?) b) financial incentives/money (if possible probe about the ways the backflow money was spent: How do you usually use this money?) c) communication with others -Any impacts on clinical practice perhaps? By exchanging and sharing info? d) time (unnecessary service duplication) 2. Have you used the IT tool? If yes, what has been your experience with the IT tool? If no, why? a) ‘ Has it enabled better a) care planning (care plans, pathways, appointments etc.) and b) communication/information sharing between professionals?’ b) How does it fit with your everyday work (routine practice, time/workload)? 49 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 c) How does it fit with other tools you use? Are you happy with the design and functionality (e.g. timely access to care plans) of the tool? What would you like to change/what is missing? 3. You said XYZ, but in your opinion, has the pilot delivered? What can be improved? (refer to earlier vision in Theme 1, probe if they felt engaged in the process) Have there been any unexpected outcomes? 50 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Appendix 5: Professional focus group protocol NWL Integrated Care Pilot Qualitative Evaluation Professional Focus Group: Protocol Date/Time: Location: Facilitation Team: NAME 1 (Lead-Facilitator), NAME 2 (Co-Facilitator), NAME 3 (CoFacilitator/Note-taker) Welcome/Introduction: Thanks for coming today. I’m (NAME) and I’m going to be the facilitator for this group. I would also like to introduce (NAMES OF CO-FACILITATORS, OTHERS). Informed Consent, Oral Notification of Taping: Before we begin, I need to ask you to sign the informed consent document you have in front of you. Do you have any questions about it? We mentioned this before but just to remind you, this session is being audiotaped. We will be using these only for making the transcripts, which will not contain your last names. Does anyone have any questions or objections? Ground Rules for Group: Let me give you a few quick ground rules for the group. First, everyone’s opinion is valued and it’s OK to disagree with each other or with me. We are very interested in hearing about all points of view. It’s OK to talk to each other and not just to me. It’s OK to get up for more coffee or to go to the toilets and since our time is limited I may need to ask you to stop and change topics from time to time. I’ll give you the ‘Time out’ sign if we need to do that. Introduction of Participants/Icebreaker: Now I’d like to go around the table so each person can give me their first name only and tell me in a few words about their involvement in the NWL ICP to date. Again, no last names or other information that would identify you and please keep it short. Introduction of Subject of Group: The primary reason we are here today is to discuss your experiences and perspectives since joining the NWL Integrated Care Pilot as a professional who provides care to patients in NWL London. Additionally, we would like to gather your opinions on any recommendations and additional comments about the NWL ICP for the future. 51 North West London Integrated Care Pilot Evaluation: Report on Work Programme 4 Opening Question(s) Q1: I want to start by asking each of you to tell me a little about what made you want to take part in the pilot? PROMPT: Do you think Integrated care is important? Why? Q2: What do you understand are the aims of the pilot? PROMPT: What is the pilot trying to achieve? Their Experience Q3: What has it been like being part of the pilot? PROMPT: What has the impact been on how you work? PROMPT: What have you learnt? PROMPT: How have you found the MDG Meetings? PROMPT: What about the IT tool? Q4: What impact has the pilot had on the care you provide to your patients? PROMPT: Have you changed how you communicate with patients? PROMPT: What difference do you hope your patients have noticed in the care you provide? The Future Q5: Do you think that this model of integrated care is feasible in practice? PROMPT: Do you think the Pilot should continue? PROMPT: Should the Pilot be embedded in normal practice? PROMPT: Would you take part in the Pilot again? Last chance question Q7: Can you give me some examples of benefits or challenges of the Pilot? Wrap-Up Q8: Are there any areas we did not talk about that you think are important for us to know about regarding the Pilot? Questions to Moderator Q9: Do you have any questions about this group or why we held it? Any final comments you would like to make? Thank you Thank you for coming. We learned a lot and it was pleasure talking with all of you. Again, thank you for sharing your thoughts. Final Arrangements Feedback, results, etc. Debrief Facilitator to debrief with co-facilitator(s) 52 Imperial College London South Kensington Campus London SW7 2AZ Tel: +44 (0)20 7589 5111 www.imperial.ac.uk . © Imperial College London 2013. Not to be reproduced without permission.